Mercer County Community College Physical Therapist Assistant Program Course Handbook
PTA 210 PTA Techniques & Modalities
Fall 2011
Fall Office Hours:
Holly Alexander Course Director MS 157 [email protected] 609-570-3478
Barbara J. Behrens Course Coordinator
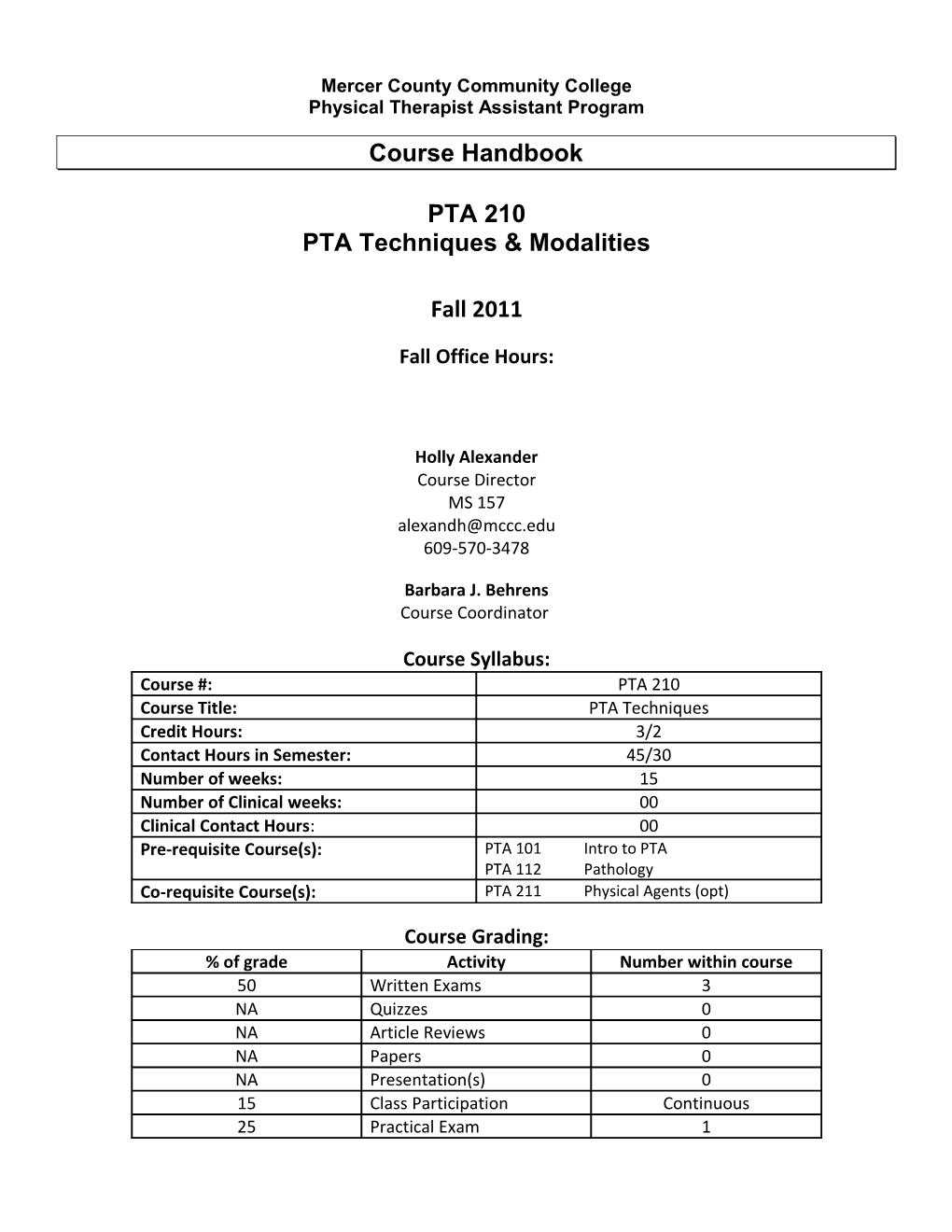
Course Syllabus: Course #: PTA 210 Course Title: PTA Techniques Credit Hours: 3/2 Contact Hours in Semester: 45/30 Number of weeks: 15 Number of Clinical weeks: 00 Clinical Contact Hours: 00 Pre-requisite Course(s): PTA 101 Intro to PTA PTA 112 Pathology Co-requisite Course(s): PTA 211 Physical Agents (opt)
Course Grading: % of grade Activity Number within course 50 Written Exams 3 NA Quizzes 0 NA Article Reviews 0 NA Papers 0 NA Presentation(s) 0 15 Class Participation Continuous 25 Practical Exam 1 10 Competency Tests** 5 ** Please note that competency tests are scheduled outside of regularly scheduled class time** CLASS PARTICIPATION:
Your class participation grade is worth 20% of the course grade and is based upon the possible total of 100 points. It is determined for this course is based upon the following :
_____ Attendance (absence and lateness) (20%) Everyone is expected to be on time and present for all class activities.
_____ Enhancing class discussions (50%) All class discussions are intended to spark dialogue. This includes active participation with the asking of appropriate questions, the addition of pertinent material brought in to share to enrich the discussion. However; inappropriate disruptions caused by learners during class time for whatever reason will result in point deductions.
_____ Preparedness (30%) It is expected that all materials that have been outlined in the course handbook have been read prior to the class meeting time. In order to ensure that materials are being read ahead of time, you will be required to summarize the required reading IN YOUR OWN WORDS. This should be hand written and no longer than 1 page. Up to 25% of the class’ summaries will be collected at random each week and will be graded.
PTAP Policy: Course Grading
One of the goals of the MCCC PTAP is to prepare student/learners to practice as PTAs. In New Jersey, as in many other states, PTAs are required to be licensed. Licensure is granted following the successful completion of a standardized licensing exam, with a score equivalent to 77 or higher. In recognition of this standard, set by a board that is external to MCCC, the PTAP will adopt 77 as the minimal passing grade. Other grade ranges are as follows:
A = 93-100 B = 83-86 C = 70 – 76 A- = 90-92 B- = 80-82 D = 60 - 69 B+ = 87-89 C+ = 77-79 F less than 59
Grades below 77 are not considered passing grades for PTAP courses, and are therefore considered unacceptable. All PTAP courses must be completed with a grade of “C+” or higher. All PTAP courses may be attempted only twice.
Required Texts
Minor, M.A., Minor, S., (2006), Patient Care Skills, 6th ed. Pearson Prentice Hall: Upper Saddle River, NJ. ISBN 978-0-13-208234-1
Bandy, B.D., Sanders, B., (2008), Therapeutic Exercise for Physical Therapist Assistants Techniques for Intervention, 2nd ed. Lippincott Williams & Williams: Philadelphia, PA. ISBN 978-0-7817-9080-2
*Mansfield, P.J., Newmann, D.A., (2009), Essentials of Kinesiology for the Physical Therapist Assistant, Mosby: St. Louis, MO. ISBN 978-0-323-03616-0
**Behrens, B.J., Michlovitz, S.L., (2006), Physical Agents: Theory & Practice 2nd ed., FA Davis Co: Philadelphia. 2 ISBN 0-8036-1134-X
**Behrens, B.J., (2006), Laboratory Manual for Physical Agents 2nd ed., F.A. Davis Co: Philadelphia. ISBN 0-8036-1135-8
*Text previously used in PTA 105 Kinesiology. ** Texts are also being used in PTA 211 Physical Agents
Course Description:
Patient care and handling techniques, including positioning & bed mobility; vital signs; transfers; gait; posture; massage; bandaging; edema management; relaxation; traction; aquatics; continuous passive motion devices; hydrotherapy and aseptic techniques. Strategies for therapeutic exercise will also be introduced and practiced throughout the course. Students develop their skills through practice with each other in the laboratory providing them with the opportunity to both administer and receive care. Skills are tested for competence throughout the semester, and integration skills for these techniques and will be tested during the practical examination at the end of the semester.
Course Goals:
The student/learner will be able to: 1. Explain and demonstrate the importance of the utilization of safe body mechanics for transporting, transferring, and/or lifting patients. 2. Describe the characteristics of a patient’s vital signs at rest and in response to exercise, and appropriately measure and document vital signs. 3. Describe the components of normal gait, and typical abnormalities of gait dysfunction. 4. Formulate a general program of therapeutic exercises to increase ROM, improve strength, and promote endurance for the upper and lower body regions. 5. Measure an ambulatory assistive device for a classmate and instruct the classmate in the appropriate use of that device. 6. Discuss and demonstrate the therapeutic benefits of soft tissue massage within the physical therapy plan of care. 7. Describe the benefits of CPM, mechanical compression, aseptic techniques, wound care, and/or pulmonary techniques for specific patient diagnoses within a physical therapy plan of care.
Course Objectives:
Following the successful completion of this course, the student/learner will possess skills in the following domains:
Cognitive/Knowledge: The student/learner will be able to successfully: 1. differentiate between clean and sterile techniques and describe the difference between them 2. describe the principles and components of a therapeutic exercise program 3. describe the sequence for postural drainage for the lobes of the lungs and differentiate between the need for one position versus another based upon lung sounds 4. describe the sequence for tissue healing 3 5. describe the differences between normal and abnormal tissue healing characteristics 6. identify the components of tissue healing that need to be documented in a patient record 7. describe the principles of body mechanics that would prevent injury to self and others 8. differentiate between safe and unsafe patient handling techniques and demonstrate safe patient handling techniques 9. identify therapeutic exercises to strengthen prime-mover muscles that have been tested and identified as needing strengthening 10. question a patient to determine his or her subjective complaints suitable for the patient record 11. list the possible ambulatory assistive devices that can be utilized for a patient with compromised weight bearing status 12. define the levels of assistance for patient activities and transfers 13. describe non-pathologic gait patterns and differentiate them from pathologic gait patterns 14. describe the components of vital signs (heart rate, respiratory rate, blood pressure) 15. list the components of a continuous passive motion device for the knee 16. describe the use of intermittent compression as a therapeutic intervention for lymph edema 17. describe chest wall expansion and excursion during inspiration and what may limit it 18. describe the characteristics of cough and sputum differentiating normal from infected sputum 19. describe the components of an aerobic conditioning therapeutic exercise program 20. describe the difference between strength and endurance
Psychomotor: The student/learner will be able to successfully: 1. demonstrate appropriate aseptic techniques to control the spread of disease 2. perform safe dependent and assisted patient transfers utilizing appropriate body mechanics 3. demonstrate body mechanics principles, assessment of vital signs and patient positioning & draping techniques that are consistent with clinical practice 4. perform clean and sterile dressing techniques 5. distinguish between bony and non-bony landmarks with accuracy 6. perform a therapeutic massage to the cervical and lumbar musculature to relieve muscle guarding 7. prepare a patient for the application of continuous passive motion or intermittent compression 8. measure a patient for ambulatory assistive devices to accommodate altered weight bearing status 9. demonstrate interpersonal skills to teach therapeutic exercises to patients and family members 10. demonstrate and teach ambulation with assistive devices (walkers, crutches, canes) on all surfaces (level, curbs, steps, ramps, carpets, tile and outdoor surfaces) 11. perform manual postural drainage techniques 12. document treatment techniques utilized with classmates in the formulation of a SOAP note 13. adjust the level of patient activity with therapeutic exercises to maintain patient safety 14. position a patient in supine, prone, side lying or sitting to decrease weight bearing on bony landmarks and to improve postural drainage 15. build a therapeutic exercise program that prepares a patient for activities of daily living (ADL), functional mobility and/or endurance training within the PT established POC demonstrate wheelchair operation for patient education and safety 16. demonstrate wheelchair operation for patient education and safety 17. measure vital signs including blood pressure, heart rate, respiratory rate at rest and during exercise 18. describe the safety and progression of patients while performing gait, wheelchair and mobility activities 19. demonstrate safe patient interaction and support during an emergency episode with a patient communicating with the supervising PT after ensuring the safety of the patient 20. demonstrate and perform passive range of motion exercises with patients on all peripheral joints 4 21. recognize positions, activities and postures that aggravate or relieve pain consult the supervising PT when there is a question about an unanticipated patient response to a therapeutic intervention to preserve patient safety
Affective : The student/learner will be able to successfully: 1. defend a patients right to privacy by protecting the patient record 2. act as an advocate for the patient by draping them to maintain patient dignity and revealing only the treatment area 3. advocate for the value of soft tissue massage as an essential therapeutic tool in the relief of muscle guarding or lymph edema management when appropriate for a patient appreciate patient privacy and dignity issues without prompting 4. advocate for the documentation of objective signs & symptoms in the patient record 5. weigh patient responses to therapeutic exercise and massage to assess patient progress versus the patient’s subjective requests 6. internalize professional behaviors when interacting as a clinician 7. recognize abnormal signs including cyanosis, orthostatic hypotension, dyspnea, tachycardia, bradycardia, etc., and act appropriately to care for the safety of the patient 8. recognize activities that aggravate or relieve edema, pain or dyspnea recognize activities that aggravate or relieve edema, pain or dyspnea and preserve patient safety 9. recognize an emergency situation in the physical therapy clinical environment and care for the safety of the patient, consulting others as appropriate
Course Outline:
Confidentiality Expectations
Patients: During the academic preparation to become a physical therapist assistant, there will be instances when you will be expected to collect data regarding a patient that you have seen or are seeing. This data will be used for educational purposes only. Do not photocopy patient information or identify the patient or individual by the use of proper names.
Sample acceptable data for collection: diagnosis prescribed medications age, gender overall medical condition of the patient previous medical history physical therapy plan of care results of tests
Classmates: Periodically during the course of the semester, individuals among your classmates may be asked to share physical anomalies or previous injuries and treatments with the PTAP class. If an individual chooses to share this information with the class, it is NOT to leave the classroom. If an individual does not wish to share a personal diagnosis or anomaly with the class, it is within his or her rights not to do so.
Volunteers will be solicited for laboratory demonstrations. Information obtained during these lab exercises is intended for demonstration purposes only. It is the right of every individual NOT to volunteer for a
5 demonstration. However, all student/learners are expected to volunteer to be a patient for their classmates. This may involve the removal of minor articles of clothing. In the event that clothing is removed, draping techniques will be employed to preserve patient dignity.
Faculty : Any and all individuals who elect to allow themselves to be the patient during class and lab activities can expect that all information gained during the activity will remain confidential. This extends to all MCCC faculty and staff members who elect to be “patients”.
Policy: Student Injuries during Clinical &/or Lab:
1. Advise your Clinical Instructor and Course Instructor (ACCE Holly Alexander) immediately of the. 2. Prepare an Injury Report and an Insurance Claim Form. Copies of both of these forms can be obtained either in the nursing office on the first floor of the MS building, or from your ACCE (Holly Alexander: MS 157). Submit completed copies of the forms to the ACCE (Holly Alexander). Keep the originals for your records. 3. Attach a copy of the incident report to the insurance claim form and follow the instructions on the form to file a claim. Students are responsible for filing all claims and for any follow up necessary, directly with the insurance company.
Expectations for Lab Sessions:
Student/learners are to come to lab sessions prepared to perform the lab activities assigned for that day. Student/learners are expected to be appropriately attired to participate fully in the lab activities scheduled for that day. Comfortable clothing that allows for full and unrestricted ease of movement, and protects the dignity of the individual (e.g. clothing that does not compromise an individual’s modesty nor expose unnecessary parts of the body) is strongly recommended. These include but are not limited to: sweat pants, gym shorts, tank tops, halter tops, sports bras, sneakers, and rubber soled closed-toe shoes. Student/learners will have locker facilities available for storage of lab clothing and supplies. Student/learners must provide their own combination lock for the lockers. Student/learners are expected to act the role as both clinician and as patient with lab partners for each scheduled lab session.
Class Philosophy:
Participants will be expected to accept responsibility for their learning, and as such will be considered learners.
Learners will identify: • topic areas that are of particular interest to them for the purpose of paper assignments • topic areas that present challenges to them • strategies for meeting his or her individual needs to master the information
Learners will also:
6 • actively participate in the presentation/discussion of course materials • actively participate in the negotiation of a class schedule that meets the objectives for the course and for the learners • respect the interests and needs of other learners or faculty • work together toward a meaningful understanding of the materials presented.
Reasonable Accommodations:
On July 26, 1990, the President of the United States signed the Americans with Disabilities Act (P.L. 101-336). The ADA is intended to remove barriers against the more than 43 million people with disabilities in the United States. If you have a documented learning disability, psychological disability, physical disability, or other hidden disability that requires an accommodation, it is your responsibility to make an appointment to meet with the course director and potentially the PTA program coordinator prior to the due date for any course examinations or assignments to discuss what accommodations might be necessary.
A list of Essential Functions for the PTA program students and graduates is available to all students by request, from any PTA program faculty member or through the program’s website.
Mercer County Community College & the Americans with Disabilities Act:
Any student in this class who has special needs because of a disability is entitled to receive accommodations. Eligible students at Mercer County Community College are assured services under the Americans with Disabilities Act and Section 504 of the Rehabilitation Act of 1973.
If you believe you are eligible for services, please contact Arlene Stinson, the Director of Academic Support Services. Ms. Stinson’s office is LB221, and she can be reached at (609) 570-3525.
Attendance for PTA program Courses:
1. Mercer County Community College does not have a "cut system." Student/learners in PTA program courses are required to attend all lecture, lab, competency testing and clinical affiliation sessions. Attendance records will be maintained.
2. If you are going to be absent from a scheduled class, it is your responsibility to notify the course instructor in writing to inform him or her of the absence and how you will be making up the work for that day. Copies of any class handouts that might have been distributed will be available in the course folders within the classroom. It is your responsibility to check the folder for the class that you would have missed to see if there was a new handout. It is not your instructor’s responsibility to attempt to keep track of what you might have missed.
2. Official college closings or delayed openings are announced on local radio stations, the college radio station WWFM, 89.1 and Mercer County Community College TV Channel 23. On other stations the college may be referred to by name or Code #922. It is the student/learner's responsibility to listen and act accordingly. Notices of emergency closings are also announced on the college website at www.mccc.edu.
7 Continued matriculation following acceptance in the PTA program indicates that the student/learner has agreed to accept and uphold his or her commitment to these policies. Competency Testing
The focus of all health related professions is the patient. As health care providers and educators, we are striving to assure that the safety of our patient is not compromised in any way by the actions of our student/learners. All PTA program laboratory courses involve direct interaction between the students and the PTA faculty. All PTA program student/learners experience both administering care and receiving care, classmates are both “patients” and “clinicians”. PTA laboratory courses also involve individualized competency testing for specified skills that have been identified as entry level skills student/learners should possess. Competency testing presents a method of assuring the clinical community that the PTA student/learner is competent and safe to perform procedures and techniques with patients.
For PTA 210, PTA 211, & PTA 212 Based upon the number of attempts that are required to fulfill competence, the following potential penalties may be employed.
Success on the 2nd attempt Unsuccessful 2nd attempt Successful on 3rd attempt Unsuccessful with 3+ attempts 5 points deducted from It is the responsibility of the 10 points deducted from No more than 3 attempts are competency grade for that student/learner to contact the competency grade for that permitted for competency course course instructor if more than course tests. Failure to perform at a a second attempt is required level of competent indicates for competency testing. that there is a problem and a need for program counseling.
What is the difference between a practical exam and a competency test? During a competency test: the tester interacts freely with the student/learner being tested. the student/learner may ask for clarification from the tester. the student/learner may submit their documentation the day after the test has been completed. Student/learners sign up for competency tests when they feel that they are ready to take them. Student/learners know exactly what test they will be demonstrating competence with.
During a practical exam: the tester does not interact with the student/learner, they take notes. the tester provides no additional information to the student/learner being tested. the documentation for the test is due at the completion of the test. Student/learners are assigned a specific testing time. Student/learners select a patient problem at the time of the test. They do not know the content of the problem in advance.
Responsibilities of the PTA student/learner: To sign up in advance to take a competency test, once he or she feels that the skill has been mastered To provide a suitable patient upon whom to perform the skill. This is most often a fellow PTA program student/learner, who is dressed in a manner that allows the technique to be performed unrestricted by jewelry or extraneous clothing. To prepare and subsequently clean up the appropriate treatment environment at the conclusion of the competency test.
8 To provide the competency tester with the appropriate documentation to sign off that he or she performed the test in a safe and competent manner.
Competency Tests
Vital Signs Objective: To be able to demonstrate safe and effective treatment technique and competence in the measurement of vital signs including blood pressure, heart rate, and respiratory rate and document the findings in a SOAP note format suitable for a patient record.
Equipment: Watch or clock with a second hand Stethoscope Sphygmomanometer Paper, pen with black ink, to record patient data
Preparation: Prepare your patient to have his or her vital signs assessed in sitting
Skill Demonstration: Monitor and record the following vital signs indicating normal values to the tester. blood pressure heart rate respiratory rate
Student/learners must be able to provide a rationale for recording each of the monitored signs, and explain the significance of each.
Documentation: Submit a SOAP note indicating your findings
Aseptic Techniques Objective: To be able to demonstrate safe and effective treatment technique in practicing universal precautions, clean and sterile techniques while changing the dressing of a sacral decubitus ulcer and documenting treatment in a SOAP note format suitable for a patient record.
The student/learner is expected to be able to: don and doff sterile and clean gloves set up a clean environment for the removal of a dressing dispose of medical waste from a soiled dressing measure and describe the size of the ulcer utilizing appropriate terminology for documentation in the patient record set up a sterile environment to apply a clean dressing to a wound apply a clean dressing to a sacral ulcer
The student/learner is responsible for:
9 providing the rationale for clean and sterile environments outlining and defending the importance of universal precautions documenting the treatment intervention utilizing appropriate terminology and measurements in a SOAP note
Therapeutic Exercise Objective: To be able to demonstrate safe and effective treatment technique in selecting, instructing and teaching a therapeutic exercise program for a patient as a part of a physical therapy intervention under the direction and supervision of a physical therapist developed plan of care and documenting the treatment in a SOAP note format suitable for a patient record.
Equipment: exercise equipment as necessary free weights cane theraband
Preparation: assemble the tools that you will need to progress a patient through a progressive resistance exercise program for upper extremity or lower extremity strength and to increase flexibility (ROM)
Skill Demonstration: instruct your patient in a therapeutic exercise program for two of the following muscle groups and their antagonists for strengthening and ROM and progress the exercises as appropriate shoulder extensors trunk extensors knee extensors elbow extensors hip extensors
teach the activities that you would like your patient to perform indicate how you would know when to progress the patient and by how much provide the rationale for teaching progressive resistive exercise activities and how they work
Documentation: Document your treatment session with the patient (SOAP) Identify which CPT Codes you would bill for and why
Transfers & Gait with Assistive Devices Objective: To be able to demonstrate safe and effective treatment technique in demonstrating and teaching transfers and ambulation with ambulatory assistive devices for level surfaces and elevation activities and document the treatment in a SOAP note format suitable for a patient record
Equipment: Wheelchair Walker Crutches Cane
Preparation: transport your patient to the treatment area in a wheelchair measure and fit your patient for each of the assistive devices
Skill Demonstration: teach your patient how to transfer into and out of the wheelchair to standing and then how to ambulate using: *0 walker NWB on L (15 feet x2)
10 *1 crutches PWB on L (15 feet x2 + ↑↓ stairs) *2 cane PWB on L (15 feet x2 + ↑↓ stairs)
Documentation: document your treatment session as if it was 3 separate treatment sessions using SOAP note format & identify which CPT Codes you would bill for and why
Massage Objective: To be able to demonstrate safe and effective treatment technique in administering a therapeutic massage to the musculature of the back to relieve muscle guarding / pain and to the upper extremity to increase mobility of scar tissue and mobility of adhesions related to tendinitis/osis. Document the treatment in a SOAP note format suitable for a patient record.
Equipment: Treatment plinth Linens (sheets for draping, towels) Massage lotion
Preparation: Prepare your patient for Cross Friction Massage or Scar Massage to the left forearm Prepare your patient for soft tissue massage of the right upper trapezius Position & drape your patient appropriately
Skill Demonstration: Forearm: Identify the type of massage that you are administering and its indication o Initiate and terminate the massage appropriately o Instruct the patient appropriately regarding expectations for the massage o Practice safe body mechanics during the treatment intervention Right Upper Trapezius: Identify each of the types of strokes and their indications o Demonstrating at least 3 types of massage strokes o Palpate to identify areas of muscle guarding, nodules, or trigger points o Administer massage to relieve palpable muscle guarding o Initiate and terminate the massage appropriately o Instruct the patient appropriately regarding expectations for the massage o Practice safe body mechanics during the massage
Documentation: Document what was palpated, performed and the patient response in a SOAP note & identify which CPT Codes you would bill for and why
11 Fall Practical Exam Instructions Preparing for Practical Day LEARNERS: Come prepared with 2 outfits. One should be appropriate attire while in the role of clinician. Hair should be up. You should also bring attire to be a patient. You should have shorts, tank tops, etc. Bring a black pen.
Your first arrival to the lab CLINICIANS: Enter the room 20 minutes prior to your scheduled time, go straight to the locker room to store your belongings and to get yourself physically ready (lab coat on, etc). It is your responsibility to enter the lab on time. At a quarter of, sign in on the sign in sheet, (which will be just inside the classroom door on the clipboard) and choose your practical scenario. Otherwise, this will result in a one point per minute deduction from your final practical grade for each class. PATIENTS: Be in the hallway at least 15 minutes prior to your scheduled time. Enter the lab 10 minutes prior to your scheduled time, sign in on the sign in sheet, (which will be just inside the classroom door on the clipboard) and have a seat in one of the wheelchairs in the waiting room. Otherwise, this will result in a one point per minute deduction from your final practical grade for each class. It is your responsibility to enter the lab on time.
15 minute Preparation CLINICIANS: After you select your patient problem, take 15 minutes to read the scenario, make any notes you need to, and prepare yourself, your patient and your treatment area. You may not leave MS 352 once you have selected your patient problem. You can take this time to ask your patient to put on a gown, to roll a pant leg up, put on shorts, tie something around a limb, etc. You will need to give the practical scenario card back prior to getting up from the table. After you are done preparing yourself, your patient, and the treatment area, YOU MUST inform your proctor that you are starting. This must happen BEFORE you wash your hands. PATIENTS: You will have 5 minutes to read a summary of the patient problem while you are waiting in the waiting room, so that you are aware of the situation. The summaries will be collected after 5 minutes. Your clinician may ask you to don a hospital gown, a pair of shorts, a tank top, roll up a pant leg, etc.
Treatment Time CLINICIANS: You have one hour to treat your patient and to clean up your treatment area. You should ideally “release” your patient at 5 of the hour and use that 5 minutes to clean up your treatment area. PATIENTS: You will be graded for being a patient. DO NOT assist the clinician with decision making skills, DO NOT give any hints, and stick to the scenario that you read.
Wrap-Up CLINICIANS: Your SOAP note documentation is due by 15 minutes after the hour and it will be collected at that time regardless if it is complete or not . All patient related documentation must be handed in to your tester (this means all paper that you took any notes on). PATIENTS: When you have been released, you are to quietly retrieve your things from the locker room and leave the lab. Reflections 12 STUDENTS: Reflections are to be completed and either placed in the bin in the lab, or emailed to Barbara (Barbara only!) or [email protected] by 5 pm. Mercer County Community College Learner: Physical Therapist Assistant Program Patient: Practical Examination Rubric Problem:
Date: Course:
Instructions: The learner will select one of the possible test scenarios that he or she will need to perform with an assigned patient. The selection will take place approximately __ 15 ___ minutes before the actual testing time. During that time notes may be made on a separate piece of paper that may be used during the testing. All papers must be turned in at the completion of the practical. Each test will take a total of __60___ minutes to complete.
The tester will be looking for the following: (from the individual being tested) 1. preparation of the treatment/assessment area for the patient (before and after the session)
10 entry level performance for a PTA Set up with appropriate equipment, supplies, assistive devices, gait belt, towels, foot stool, all were put away at end of Rx 9 competent for a PTA learner at this level Set up was mostly appropriate with minor exceptions, the learner needed to leave the patient to get something, the patient was safe & supported 8 frazzled but safe Set up was appropriate with minor exceptions, learner just forgot several things and left pt. but pt. was supported & safe (several times) 7 Inappropriate forgot to clean up or use a sheet on the treatment plinth during Rx 6 Unsafe left the patient unsupported when going to retrieve something needed for treatment 5 fraudulent 4 disrespectful to the patient leaving a patient in the treatment area at the conclusion of Rx, not concluding Rx 3 forgotten or incomplete task performance Comment:
2. preparation of the clinician, hand-washing before touching a patient, lab coat and name tag
10 entry level performance for a PTA hot water, towel to turn on and off water, 15 second scrub with soap, sleeves away from wrists, name tag with his or her name, coat buttoned & neat 9 competent for a PTA learner at this level hot water, towel to turn on and off water, 15 second scrub with soap, sleeves away from wrists, name tag 8 frazzled but safe hot water, towel to turn on and off water, 15 second scrub with soap, sleeves away from wrists, 7 Inappropriate cold water, no towel to turn on and off water, 5 second scrub with soap ,no name tag , continually touching self and re-washing hands (leaving pt.) 6 Unsafe cold water, no towel to turn on and off water, touching oneself after washing hands and not re- washing hands 5 fraudulent wrong name on name tag 4 disrespectful to the patient no lab coat, or no name tag 3 forgotten or incomplete task performance forgot to wash hands, touched self and forgot to wash hands, forgot lab coat or name tag and remembered any of these in Rx Comment:
3. to see how the clinician introduces him/herself to the patient (name & title), (clarity and speed)
10 entry level performance for a PTA My name is “”I am a Physical Therapist Assistant Student and I will be working with you today. Slow, clear, easily audible, acknowledged. 9 competent for a PTA learner at this level as above but the volume, speed or clarity could be improved 8 frazzled but safe as above but Physical Therapy Assistant Student and/or the volume, speed or clarity could be improved 7 Inappropriate as above but Physical Therapy Assistant or Physical Therapist Assistant and /or the volume, speed or clarity could be improved 6 Unsafe 5 Fraudulent My name is “”I am a Physical Therapist Student and I will be working with you today. Slow, clear, easily audible, acknowledged. 4 disrespectful to the patient No eye contact, utilization of poor grammar 3 forgotten or incomplete task performance no introduction 13 Comment:
4. to see that the dignity of the patient is respected by making eye contact at eye level, draping the patient, allowing the pt. to do as much as he/she can do for him/herself
10 entry level performance for a PTA intro at eye level, greet pt., have pt. propel him or herself to Rx area if capable, pt. Hx in Rx area, drape pt. at all times, pt. is responsible for w/c 9 competent for a PTA learner at this level as above, may not remember to speak to pt. only in Rx area 8 frazzled but safe 7 Inappropriate reviewing Hx in Rx area or pushing pt. to Rx area, or not permitting able pt. to perform tasks (one of these) 6 Unsafe 5 Fraudulent 4 disrespectful to the patient Not draping the pt and more than one of the items from “inappropriate” 3 forgotten or incomplete task performance Comment:
5. to see that the pt. is positioned appropriately for what is being done with them and that they are not asked to change positions un-necessarily.
10 entry level performance for a PTA initially positioning the pt so that he/she can perform all activities that can be formed in one position before having a pt. change positions 9 competent for a PTA learner at this level as above but the initial position may need to be changed resulting in more than one position change 8 frazzled but safe the SPTA realized that position changes were necessary and explained the need for a change to the patient accepting responsibility 7 Inappropriate the SPTA had the pt. change position more than 3 times including a return to a position due to poor planning, accepting NO responsibility 6 Unsafe the SPTA repeatedly had the pt change position and failed to guard the changes or explain the reasons for the change 5 Fraudulent 4 disrespectful to the patient 3 forgotten or incomplete task performance Comment:
6. to see that things are explained to the patient in terms that he/she is capable of understanding
10 entry level performance for a PTA the SPTA explained all activities in lay terminology and demonstrated activities before expecting pt. to perform task, asked for ?s 9 competent for a PTA learner at this level the SPTA used medical terminology and demonstrated activities before expecting pt. to perform task, asked for ?s 8 frazzled but safe the SPTA explained all activities in lay terminology and demonstrated activities before expecting pt. to perform task, but may have forgotten side 7 inappropriate the SPTA explained all activities in medical terminology and did not demonstrate or ask pt if he/she had any ?s 6 Unsafe the SPTA explained some but not all of the activities OR did it in an inappropriate format for THIS patient 5 fraudulent 4 disrespectful to the patient 3 forgotten or incomplete task performance No instruction took place prior to the expectation that the pt. would be expected to respond or perform something Comment:
7. to see that session measurements are accurate and in agreement with the testers visual assessment of the measurements and the session, recording only what is done and planned
10 entry level performance for a PTA The SPTA used SOAP note format, was accurate, documented the side, reps, Rx, pt. comments, outcome etc. and signed leaving no blank spaces 9 competent for a PTA learner at this level as above but there might have been blank spaces 8 frazzled but safe as in “10” but the side, # of reps, or professional designation may have been left out. (only one omission) 7 Inappropriate there was more than one omission of information or the measurements were not in agreement with the tester 6 unsafe 5 Fraudulent a side other than the side measured or treated was documented 4 disrespectful to the patient 3 forgotten or incomplete task performance 14 Comment:
8. to see that the documentation is meaningful and accurate, using correct abbreviations, spelling, and documentation format in black ink
10 entry level performance for a PTA 9 competent for a PTA learner at this level 8 frazzled but safe 7 Inappropriate 6 Unsafe 5 fraudulent 4 disrespectful to the patient 3 forgotten or incomplete task performance Comment:
9. Patient Safety: to see that the treatment has been prioritized for the patient with evidence of a physiologically sound and rational plan for the session
10 entry level performance for a PTA 9 competent for a PTA learner at this level 8 frazzled but safe 7 Inappropriate 6 Unsafe 5 Fraudulent 4 disrespectful to the patient 3 forgotten or incomplete task performance Comment:
10. Patient Safety: to see that the demonstration of the selected tasks with the patient is done with evidence of skill and safety in the techniques performed
10 entry level performance for a PTA 9 competent for a PTA learner at this level 8 frazzled but safe 7 Inappropriate 6 Unsafe 5 Fraudulent 4 disrespectful to the patient 3 forgotten or incomplete task performance Comment:
The tester will be looking for the following from the “patient” during the test: that the patient does ONLY what he or she is told to do the patient does NOT try to help the clinician that the patient does NOT ask questions of the tester that the patient does NOT prepare or clean up the area that the patient respects the stress of the clinician and do not try to make it more difficult for the clinician to successfully complete the practical Please note: Patient safety is a critical component for the successful completion of this and all PTA program courses within the PTA curriculum. Items 9 & 10 on the list are considered to be skills that must have a score of “8” of higher for the learner to pass this practical examination.
Summary Total Score for the Clinician: Review Date: 1 2 3 Point Deductions (as a patient): Learner Initials: 4 5 6 7 Final Score: Safe/Unsafe 8 9
15 10 Tester: Total
16 Exam Error Analysis
Course: Exam: Date:
Error Type Misread Didn’t read Didn’t know the Didn’t read Changed my Just answered it the the question information all the choices answer in correctly question Place a checkmark for each time you: Total for this exam
Course: Exam: Date: Error Type Misread Didn’t read Didn’t know the Didn’t read Changed my Just answered it the the question information all the choices answer in correctly question Place a checkmark for each time you: Total for this exam
Course: Exam: Date: Error Type Misread Didn’t read Didn’t know the Didn’t read Changed my Just answered it the the question information all the choices answer in correctly question Place a checkmark for each time you: Total for this exam
17 Mercer County Community College Physical Therapist Assistant Program
PTA 210 PTA Techniques & Modalities Fall 2011 ======Course Schedule: Fall 2011 Monday & Wednesdays: 9-11 Location: MS 352 Thursday: Lab 9 -12 or 1-4 ======
Week Date Topic(s) Objective(s) Chapter(s) 1 8/29 Vital Signs & Aseptic Techniques C1, C4, C5, C14, P1, P18,P,20, A8, Minor Ch 4, 5 A9, A10, CG2, CG7 2 9/5 Patient Positioning & Draping, C4, C5, C6, C10, P1, P4, P5, P15, Minor Ch 4 &8, Wound Care P22, A3, A5, A7, , CG7 and pg 68 3 9/12 Body Mechanics, CG1, C7, C8, C12, P2, P3, P17, P19 Minor Ch 7 and Bed Mobility & Transfers, pg 63-65, 166
9/19-9/22 (M-R) Written Exam # 1 (in the testing center) 4 9/19 Wheelchair Components & Fit CG2, CG4, C2, C9, C10, C20, P10, Minor Ch 6 Therapeutic Exercise P13, P14, P16, P18, P20, A6, A8, Kisner & Colby A9, A10 Ch 1 5 9/26 Normal Gait CG3, C13, Mansfield Ch 12* Abnormal Gait 6 10/3 Gait with Assistive Devices CG3, CG5, C11, C12, C13, P9, P11, Minor Ch 10 P19, A8, A9, A10 10/10-13 (M-R) Written Exam # 2 (in the testing center) 7 10/10 Massage CG6, C10, P3, P5, P6, P7, P13, P22, No required A1, A3, A4, A6, A7, reading 8 10/17 Edema Management CG7, A4, A6, A9 Behrens Ch 7** (Bring Physical Agents Lab Manual to lab this week) 9 10/24 Pulmonary Pathology & Chest PT Kisner & Colby Ch 25 10 10/31 Practical Exam CG1, CG2, CG3, CG4, CG5, CG6, (tentative 11/3 & 11/4) CG7 11,12, 11/7-12/6 PTA 225 Clinical Education I 13,14
15 12/7 Clin Ed Review CG4, CG7, C2, C3, C10, C17, C18, Kisner & Colby Cardiac Pathology & Rehab C19, C20, P1, P3, P12, P13, P15, Ch 7 P16, A8, A9, A10 12/12 Cardiac Rehab & Exam Review CG4, CG7, C2, C3, C10, C17, C18, C19, C20, P1, P3, P12, P13, P15, Kisner & Colby P16, A8, A9, A10 Ch 7 12/14 Written Exam # 3
PTA 210 PTA Techniques 1. Vital Signs Lab Date: 9/1 Test week: 9/12
18 2. Aseptic Techniques Lab Date: 9/8 Test week: 9/19 3. Therapeutic Exercise Lab Date: 9/22 Test week: 10/3 4. Transfers & Gait with Assistive Devices Lab Date: 10/6 Test week: 10/17 5. Massage Lab Date: 10/13 Test week: 10/24
19