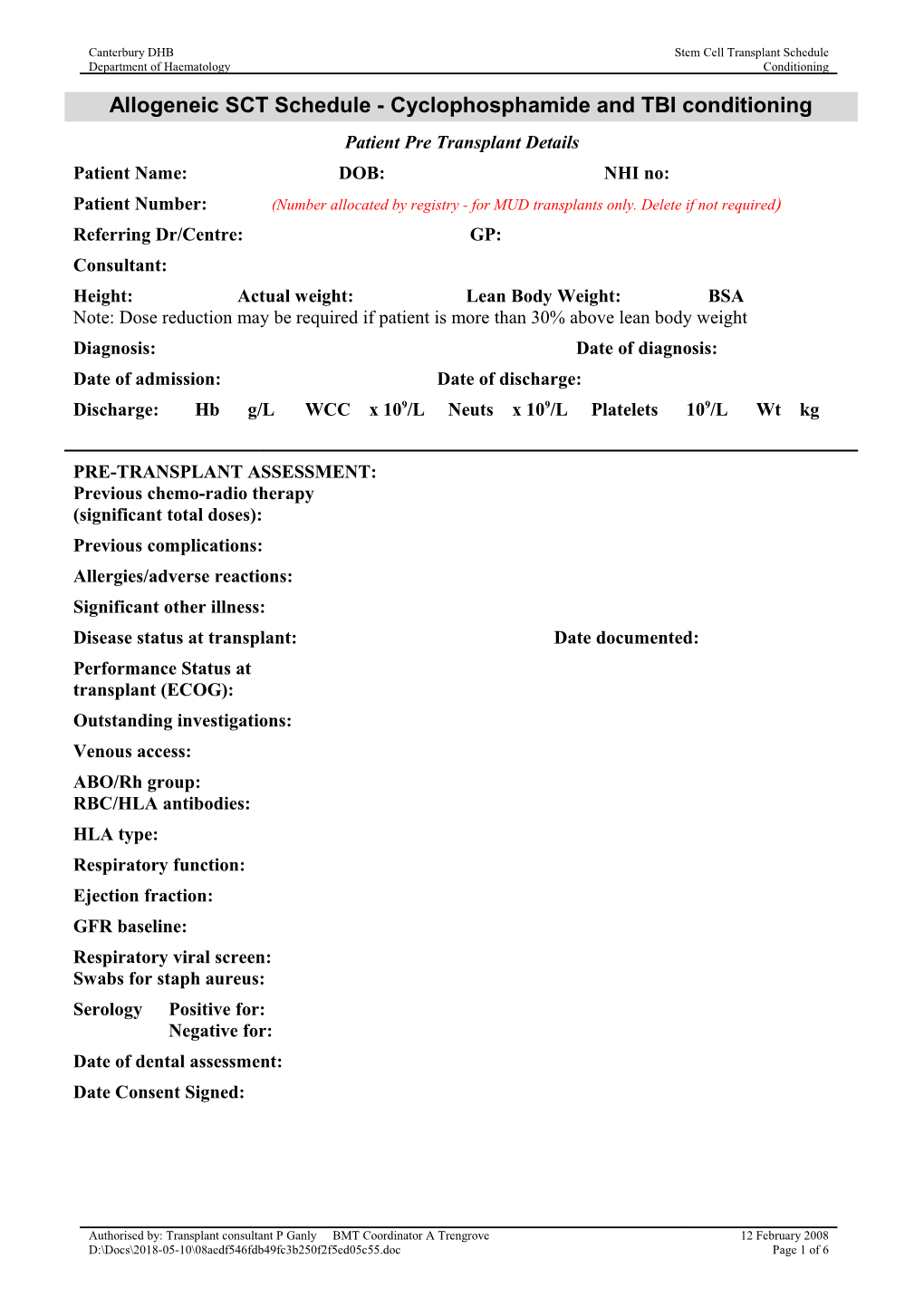
Canterbury DHB Stem Cell Transplant Schedule Department of Haematology Conditioning
Allogeneic SCT Schedule - Cyclophosphamide and TBI conditioning Patient Pre Transplant Details Patient Name: DOB: NHI no: Patient Number: (Number allocated by registry - for MUD transplants only. Delete if not required) Referring Dr/Centre: GP: Consultant: Height: Actual weight: Lean Body Weight: BSA Note: Dose reduction may be required if patient is more than 30% above lean body weight Diagnosis: Date of diagnosis: Date of admission: Date of discharge: Discharge: Hb g/L WCC x 109/L Neuts x 109/L Platelets 109/L Wt kg
PRE-TRANSPLANT ASSESSMENT: Previous chemo-radio therapy (significant total doses): Previous complications: Allergies/adverse reactions: Significant other illness: Disease status at transplant: Date documented: Performance Status at transplant (ECOG): Outstanding investigations: Venous access: ABO/Rh group: RBC/HLA antibodies: HLA type: Respiratory function: Ejection fraction: GFR baseline: Respiratory viral screen: Swabs for staph aureus: Serology Positive for: Negative for: Date of dental assessment: Date Consent Signed:
Authorised by: Transplant consultant P Ganly BMT Coordinator A Trengrove 12 February 2008 D:\Docs\2018-05-10\08aedf546fdb49fc3b250f2f5ed05c55.doc Page 1 of 6 Canterbury DHB Stem Cell Transplant Schedule Department of Haematology Conditioning
Allogeneic Donor Details
Donor name: DOB: NHI no: Donor Consultant: GP: Weight: Date of donor assessment: ABO/Rh group: RBC/HLA antibodies: HLA type: Serology - Positive for: Negative for: Consent signed:
Check List for Patient v Donor
PATIENT DONOR HLA type: ABO/Rh group: ? Blood group incompatibility: ABO major Yes / NA ABO minor Yes / NA ABO mixed Yes / NA Rh incompatibility Yes/ NA CMV status: Red cell Xmatch: Date of donor admission:
Authorised by: Transplant consultant P Ganly BMT Coordinator A Trengrove 12 February 2008 D:\Docs\2018-05-10\08aedf546fdb49fc3b250f2f5ed05c55.doc Page 2 of 6 Canterbury DHB Stem Cell Transplant Schedule Department of Haematology Conditioning
Transplant Protocol – Conditioning and Peritransplant Supportive Care
BLOOD PRODUCT SUPPORT: All blood products to be irradiated from 6 weeks prior to transplant and for at least 12 months following, longer if significant chronic GVHD. CMV negative blood products are not required. Insert relevant instruction for any mismatches from Transplant red book (in notes/blood products)
CONDITIONING REGIME: SIBLING Cyclophosphamide 60mg/kg for 2 days, days, -6,-5 Total Body Irradiation 12Gy in 6 fractions over 3 days, days -3, -2, -1
MUD Cyclophosphamide 60mg/kg for 2 days, days, -6,-5 Total Body Irradiation 13.2Gy in 6 fractions over 3 days, days -3, -2, -1
STEM CELL SOURCE: Bone Marrow/PBSC (Delete source which is not applicable) Date of Harvest: Re-infused Dose (CD34+): Ex vivo manipulation: Delete if none planned Other details:
GVHD PROPHYLAXIS Ciclosporin: 2.5mg/kg IV BD from day –1 to day +3. 1.5mg/kg IV BD from day +4 to day +8. Check levels day +4 and there after Monday and Thursday and adjust dose to maintain levels between 95-205mcg/L. Taper from day 100 by approximately 10% of initial dose per week. Aim to have stopped ciclosporin by day +180 Methrotrexate: 15mg/m2 IV bolus on day +1 10mg/m2 IV bolus on days +3, +6 +11 Folinic acid as charted.
VOD PROPHYLAXIS Ursodiol 300mg TDS day -8 to day +90
ANTIEMETICS: Ondansetron 8mg Q12H PO/IV +/- Dexamethasone 8 mg BD PO (stop prior to stem cell infusion) +/- Metoclopramide 10-20mg QID PO/IV +/- Cyclizine 50mg TDS PO/IV +/- Lorazepam 2mg PO PRN +/- Scopolamine patch changed every 3rd day
MENORRHAGIA PREVENTION: (delete if not female) Avoid Norethisterone use Leuprorelin 3.75mg s/c monthly from 1 month prior to transplant.
SPECIAL NOTES FOR THIS PATIENT:
Authorised by: Transplant consultant P Ganly BMT Coordinator A Trengrove 12 February 2008 D:\Docs\2018-05-10\08aedf546fdb49fc3b250f2f5ed05c55.doc Page 3 of 6 Canterbury DHB Stem Cell Transplant Schedule Department of Haematology Conditioning
Transplant Protocol – infection prophylaxis Protected environment: From start of conditioning until neutrophils > 0.5 X 109/L PI diet: From admission for at least 12 weeks (longer if significant GvHD) Neutropenic bacterial Ciprofloxin 500mg BD from day 0 until neutrophils >0.5 X 109/L. prophylaxis: Antifungal prophylaxis: Fluconazole 200mg PO daily from day -3 until neutrophils > 0.5 X 109/L. HSV/VZV prophylaxis: If patient HSV seropositive and/or has had significant problems (delete option(s) which do not with Herpes Simplex in the past: Give aciclovir 400mg PO BD to apply) commence at start of conditioning. Continue until discharge or 1 month post transplant (whichever is longer). If patient VZV seropositive: Aciclovir 800mg PO BD to commence at start of conditioning. Continue until 1 year post transplant. CMV prevention: If either or both patient and donor are CMV seropositive: Monitor (delete option which does not CMV DNA by quantitative PCR weekly from Day 10 until Day apply) 100, or longer if patient has had CMV reactivation or develops GVHD and remains on prednisone at more than 1mg/kg/day. If the CMV viral load is rising or becomes >1000 copies/ml, give ganciclovir 5mg/kg IV in 100mL 0.9S over 1 hour until CMV PCR is negative, discuss with ID team. If both patient and donor are CMV seronegative: Ganciclovir will not be given. Consider PCR monitoring if CMV and/or GVHD are suspected. PCP prophylaxis: Cotrimoxazole 960mg BD for 7 days, day –7 to day –1. Then cotrimoxazole 480 mg PO daily. If intolerant of cotrimoxazole, give dapsone 100 mg PO daily, or use pentamidine 300mg in 250mL 0.9S over 2 hours each month.
Toxoplasmosis prophylaxis: Cotrimoxazole as above (but not pentamidine) is suitable for (delete if toxoplasmosis toxoplasmosis prophylaxis. Toxoplasmosis prophylaxis should be seronegative) continued for 6 months or until off therapy for GVHD. If intolerant of cotrimoxazole, the alternative is clindamycin 300- 450mg TDS, pyrimethamine 25-75mg daily and folinic acid 10- 25mg QDS. Long term bacterial Penicillin 500mg BD on engraftment for at least 18 months post prophylaxis: transplant (until initial immunisation programme completed). If allergic to penicillin use erythromycin 250mg BD
Authorised by: Transplant consultant P Ganly BMT Coordinator A Trengrove 12 February 2008 D:\Docs\2018-05-10\08aedf546fdb49fc3b250f2f5ed05c55.doc Page 4 of 6 Canterbury DHB Stem Cell Transplant Schedule Department of Haematology Conditioning
Daily Inpatient Transplant Schedule:
DAY DATE BMT DAY PLAN Time + -7 Admit to ward, CBC + D, ONCO, Urea, Magnesium , CRP, LFT’s LDH, Immunoglobulins, retics, coag. 10ml EDTA for DNA storage to Molecular Biology (ext89878). Commence allopurinol, antiemetics Commence ursodiol 300mg TDS Commence cotrimoxazole 960mg BD for 7, days day -7 to day -1 Commence aciclovir if required, otherwise delete Dapsone 100mg PO daily or Pentamidine 300mg in 250mL 0.9S over 2 hrs if unable to take cotrimoxazole, otherwise delete 2000 1L 0.9S overnight Friday -6 0500 D4S 1L + 30mmol KCl over 4 hours 0800 Ondansetron 8mg PO/IV 0830 MESNA (20mg/kg) mg IV bolus 0900 Cyclophosphamide (60mg/kg) mg in 1L D5W over 1 hr 1000 D4S 1L + 30mmol KCl + 8mg frusemide over 4 hours 1200 MESNA (20mg/kg) mg IV bolus 1400 0.9S 1L + 30mmol KCl + 8mg frusemide over 4 hours 1500 MESNA (20mg/kg) mg IV bolus 1800 MESNA (20mg/kg) mg IV bolus D4S 1L + 30mmol KCl + 8mg frusemide over 4 hours 2000 Ondansetron 8mg IV bolus 2200 D4S 1L + 30mmol KCl + 8mg frusemide over 4 hours 2400 Stop clonazepam Saturday -5 0200 0.9S 1L + 30mmol KCl + 8mg frusemide over 4 hours 0600 D4S 1L + 30mmol KCl + 8mg frusemide over 4 hours (STOP & DISCARD REMAINDER AT 0900) 0800 Ondansetron 8mg IV bolus 0830 MESNA (20mg/kg) mg IV bolus 0900 Cyclophosphamide (60mg/kg) mg in 1L D5W over 1 hr 1000 D4S 1L + 30mmol KCl + 8mg frusemide over 4 hours 1200 MESNA (20mg/kg) mg IV bolus 1400 0.9S 1L + 30mmol KCl + 8mg frusemide over 4 hours 1500 MESNA (20mg/kg) mg IV bolus 1800 MESNA (20mg/kg) mg IV bolus D4S 1L + 30mmol KCl + 8mg frusemide over 4 hours 2000 Ondansetron 8mg IV bolus 2200 D4S 1L + 30mmol KCl + 8mg frusemide over 4 hours Sunday -4 0200 0.9S 1L + 30mmol KCl + 8mg frusemide over 4 hours 0600 D4S 1L + 30mmol KCl + 8mg frusemide over 4 hours IV MAINTAINANCE FLUIDS THEREAFTER Monday -3 0730 TBI ondansetron 8mg PO/IV and dexamethasone 8mg PO 1630 TBI ondansetron 8mg PO/IV and dexamethasone 8mg PO Tuesday -2 0730 TBI ondansetron 8mg PO/IV and dexamethasone 8mg PO 1630 TBI ondansetron 8mg PO/IV and dexamethasone 8mg PO
Authorised by: Transplant consultant P Ganly BMT Coordinator A Trengrove 12 February 2008 D:\Docs\2018-05-10\08aedf546fdb49fc3b250f2f5ed05c55.doc Page 5 of 6 Canterbury DHB Stem Cell Transplant Schedule Department of Haematology Conditioning
DAY DATE BMT DAY PLAN Time Wednesday -1 0730 TBI ondansetron 8mg PO/IV and dexamethasone 8mg PO 0800 Start Ciclosporin (2.5mg/kg) BD IV mg BD Stop allopurinol 1630 TBI ondansetron 8mg PO/IV and dexamethasone 8mg PO Thursday 0 0800 Commence ciprofloxacin 500mg BD Stop cotrimoxazole until stable engraftment Red cell X match with donor cells 1000 INFUSION OF HAEMATOPOIETIC STEM CELLS insert relevant reinfusion instruction from red book Friday +1 1300 Commence methotrexate (15mg/m2) mg IV bolus and folinic acid rescue as per protocol – ensure 24hrs post BM infusion Sunday +3 1300 2nd dose of methotrexate (10mg/m2) mg IV bolus and folinic acid rescue as per protocol Monday +4 Check ciclosporin levels, maintain levels between 95- 205mcg/L 0800 Ciclosporin dose changed to (1.5mg/kg) mg BD IV continue as charted Wednesday +6 1300 3rd dose of methotrexate (10mg/m2) mg IV bolus and folinic acid rescue as per protocol Monday +11 1300 4th dose of methotrexate (10mg/m2) mg IV bolus and folinic acid rescue as per protocol (stop 4 days post MTX) Saturday +16 Folinic Acid rescue now completed
Protocol authorised by: NAME: ______SIGN:______DATE:______NAME: ______SIGN:______DATE:______CONSULTANTS (Original signed only)
Authorised by: Transplant consultant P Ganly BMT Coordinator A Trengrove 12 February 2008 D:\Docs\2018-05-10\08aedf546fdb49fc3b250f2f5ed05c55.doc Page 6 of 6