3-24-05 Diagnosis and Treatment Substance Abuse
1. Personal History and Physical Findings indicative of substance abuse
Have to ASK!! Can use CAGE or other questions: Have you used ______substance? If yes, proceed with other questions: How long; How often; Why; Have you considered stopping? Do you have to increase amount of substance to get desired effect? Have you ever had emotional, psychological, physical problems related to use?
Physical findings: Pupils dilated Skin marks (scars, tracks, abscesses) Nasal septum inflamed/perforated Heart Murmur Elevated pulse or BP Alcohol Varices
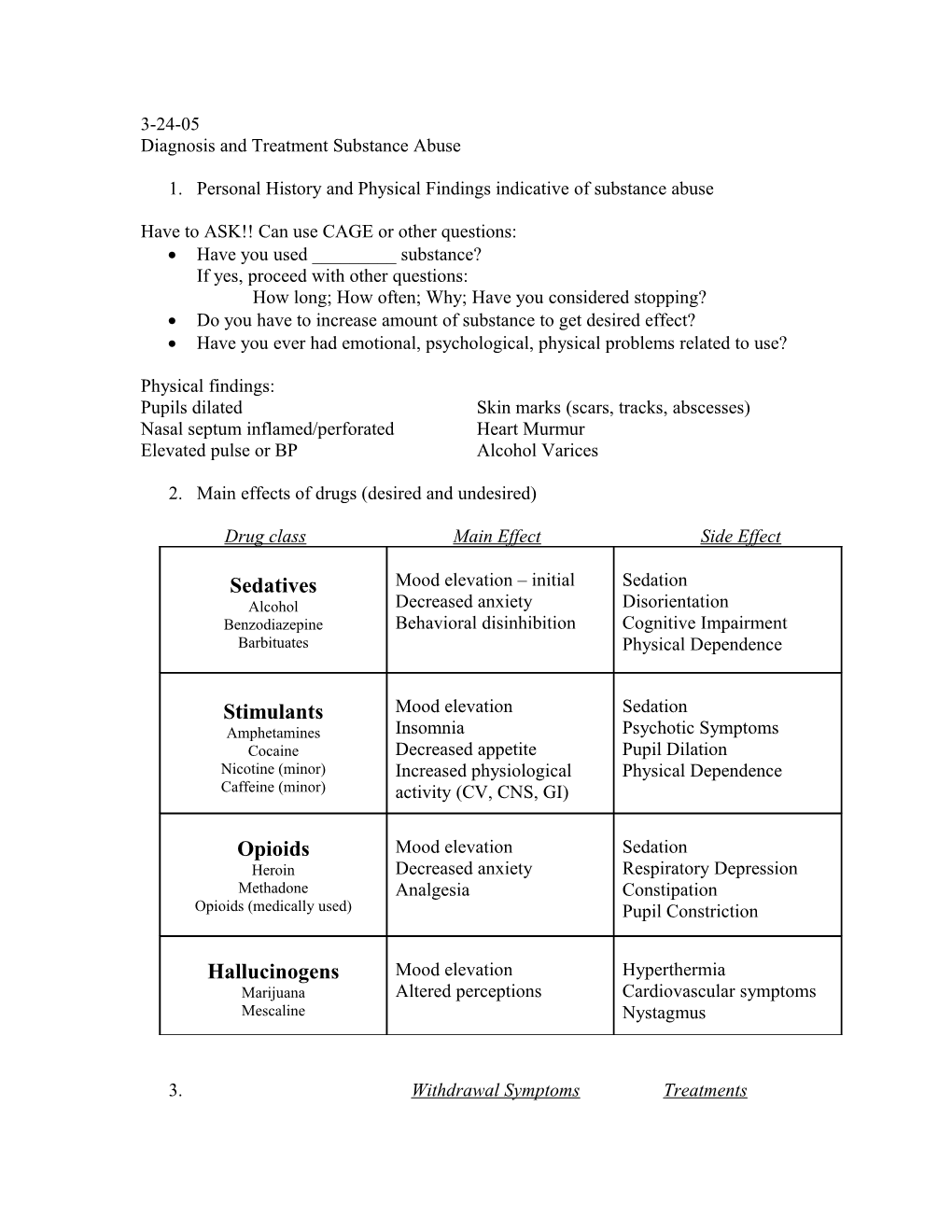
2. Main effects of drugs (desired and undesired)
Drug class Main Effect Side Effect
Sedatives Mood elevation – initial Sedation Alcohol Decreased anxiety Disorientation Benzodiazepine Behavioral disinhibition Cognitive Impairment Barbituates Physical Dependence
Stimulants Mood elevation Sedation Amphetamines Insomnia Psychotic Symptoms Cocaine Decreased appetite Pupil Dilation Nicotine (minor) Increased physiological Physical Dependence Caffeine (minor) activity (CV, CNS, GI)
Opioids Mood elevation Sedation Heroin Decreased anxiety Respiratory Depression Methadone Analgesia Constipation Opioids (medically used) Pupil Constriction
Hallucinogens Mood elevation Hyperthermia Marijuana Altered perceptions Cardiovascular symptoms Mescaline Nystagmus
3. Withdrawal Symptoms Treatments Sedatives Mood depression Hospitalization and Alcohol Increased anxiety observation (severe cases) Benzodiazepine Delirium Taper down dose of drug Barbituates Seizures Anti-seizure meds Cardiovascular crisis ETOH: vitamin supplem. Mood depression Stimulants Lethargy Benzodiazepines (to Amphetamines Increased appetite decrease agitation) Cocaine Decreased physiological Antipsychotics Nicotine (minor) activity (CV, CNS, GI) Phys/Psych Support Caffeine (minor) Headache
Opioids Mood depression Hospitalization (if O/D) Heroin Increased anxiety Clonidine (to stabilize Methadone Autonomic Instability ANS) Opioids (medically used) Piloerection Taper down drug dose Excessive Yawning Cramps/Diarrhea Hallucinogens Few Marijuana Mescaline
4. Benefits to Patients who are in pain: Relief from pain Better control over pain cycle Increased physical functions Better function as person
Potential Risks: Dependence Intoxication Impairment cognitive capacity Illegal use of drugs – selling for profit
5. Safe prescribing of narcotics should include: A full diagnostic evaluation of pain and symptoms Evaluation of degree of pain and affect on function Trial of other (less risky) meds for pain management Physical and psychological assessment of patient and their risk of abuse If doctor and patient agree to try a narcotic medicine: A discussion about goals and objectives of treatment should be had A written contract including risk awareness, dosage, and refills should be made Consequences for contract violation should be made aware Key = Good communication, documentation, and respect! Relief can be had from chronic pain if physicians and patients can talk openly and come to agreement…