Business Case for full-time Trust Registrar in Ortho-geriatrics
Background
The initial proposal for a part-time consultant ortho-geriatrician was presented as part of a general business case to develop an improved fracture neck of femur pathway at the Executive management committee in February 2008. The consultant and additional trauma list were agreed although delayed for almost a year due to financial constraints. At this stage, it was suggested that the junior doctor support recommended (an F1 and a SHO grade) was reviewed following implementation.
The Fracture Neck of Femur Pathway project became part of the Patients first programme in December 2008. With the appointment of the sixth geriatrician, the Consultant –led ortho-geriatric service started on the 18th March 2009. All patients with fractured neck of femur are managed jointly under orthopaedic and Ortho- geriatric care and targets for improvement have been set.
Junior staffing
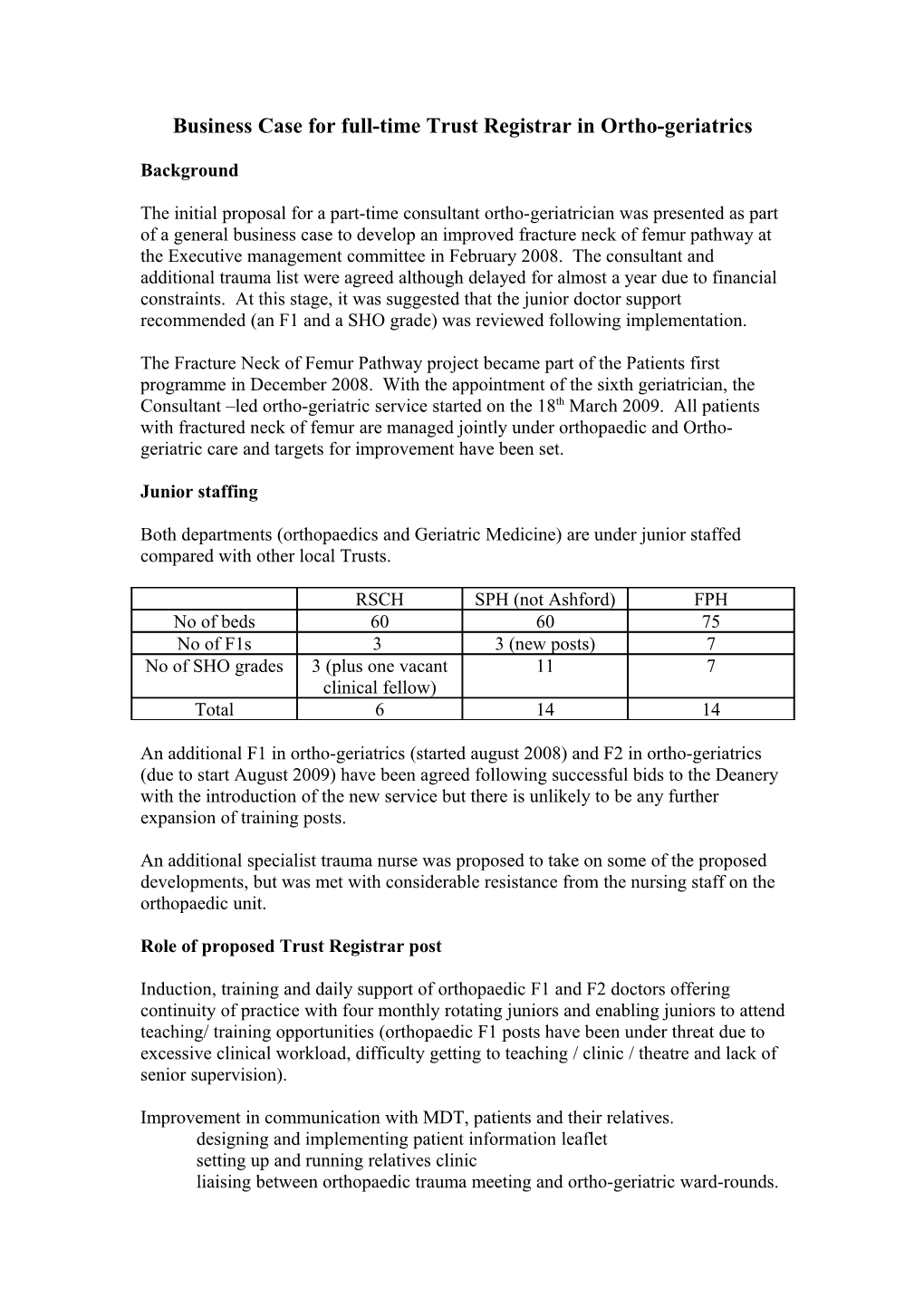
Both departments (orthopaedics and Geriatric Medicine) are under junior staffed compared with other local Trusts.
RSCH SPH (not Ashford) FPH No of beds 60 60 75 No of F1s 3 3 (new posts) 7 No of SHO grades 3 (plus one vacant 11 7 clinical fellow) Total 6 14 14
An additional F1 in ortho-geriatrics (started august 2008) and F2 in ortho-geriatrics (due to start August 2009) have been agreed following successful bids to the Deanery with the introduction of the new service but there is unlikely to be any further expansion of training posts.
An additional specialist trauma nurse was proposed to take on some of the proposed developments, but was met with considerable resistance from the nursing staff on the orthopaedic unit.
Role of proposed Trust Registrar post
Induction, training and daily support of orthopaedic F1 and F2 doctors offering continuity of practice with four monthly rotating juniors and enabling juniors to attend teaching/ training opportunities (orthopaedic F1 posts have been under threat due to excessive clinical workload, difficulty getting to teaching / clinic / theatre and lack of senior supervision).
Improvement in communication with MDT, patients and their relatives. designing and implementing patient information leaflet setting up and running relatives clinic liaising between orthopaedic trauma meeting and ortho-geriatric ward-rounds. Pre-optimisation of pre-operative patients and liaising with anaesthetists Fascio-iliaca nerve blocks (performing in new patients and teaching other staff)
Audit: Managing National fractured neck of femur audit data to feedback to Trust on patients first targets Feedback to South West Thames Ortho-geriatric Network on service developments
Develop other Research ideas: use of fascio-iliaca nerve blocks in fractured neck of femur patients (with Dr Gillian Foxall) use of USCOM monitoring in pre-optimising fractured neck of femur patients (with Dr Mike Scott)
Regular training sessions and updates for A&E staff, SNPs and the MDT in aspects of the ortho-geriatric service.
Risks of proposal
Difficulty in appointing to Trust Registrar post. However, this post offers excellent research and audit opportunities for either Geriatric medicine or Orthopaedic trainee. Would try to get it recognised for training and allow current geriatric medicine SpRs to rotate through to gain experience of ortho-geriatrics.
Risks of doing nothing
Unlikely ortho-geriatric service will meet targets set out in patients first project without additional junior staff (particularly increased length of stay as tests don’t get ordered, referrals don’t get made and difficulty getting TTOs completed).
The removal of orthopaedic F1 posts by the Deanery due to excessive clinical workload, and lack of senior supervision.
Inability to take forward anaesthetic projects which hopes to improve pre-optimisation of fracture NOF patients using non-invasive monitoring and to improve pain relief by using nerve blocks which will hopefully allow earlier mobilisation, reduce complications of opiates and shorten length of stay. Both projects require a trained individual to pilot these ideas which we hope to roll out for all patients in the future.
Alternatives
Increase more junior staff or consultant time but either unlikely to be as cost-effective. Employ additional specialist nurse – already discussed with current trauma nurse specialist and Matron who had reservations about taking on iliaca nerve blocks / pre- optimisation as Pilot. Proposed weekly timetable
Monday Tuesday Wednesday Thursday Friday
8-9am Trauma Trauma Trauma Trauma Trauma meeting meeting meeting meeting meeting Journal club 9.30- New patient New patient Geriatric x- New patient New patient 10.30am review review ray meeting review review
10.30am Ward-round Ward-round MDT Ward-round Ward-round HK HW HK HW
New patient review
Geriatric medicine Tutorial
2-4pm Ward-work Follow-up Relatives Ward-work Follow-up Audit / clinic clinic Audit / clinic Research (alt weeks) Research (alt weeks)
education / education / training training
Basic forty hours per week. (medical SBU may wish to think about banding and using this post on the on-call rota)