Osteoarthritis (Degenerative Joint Disease)
Definition
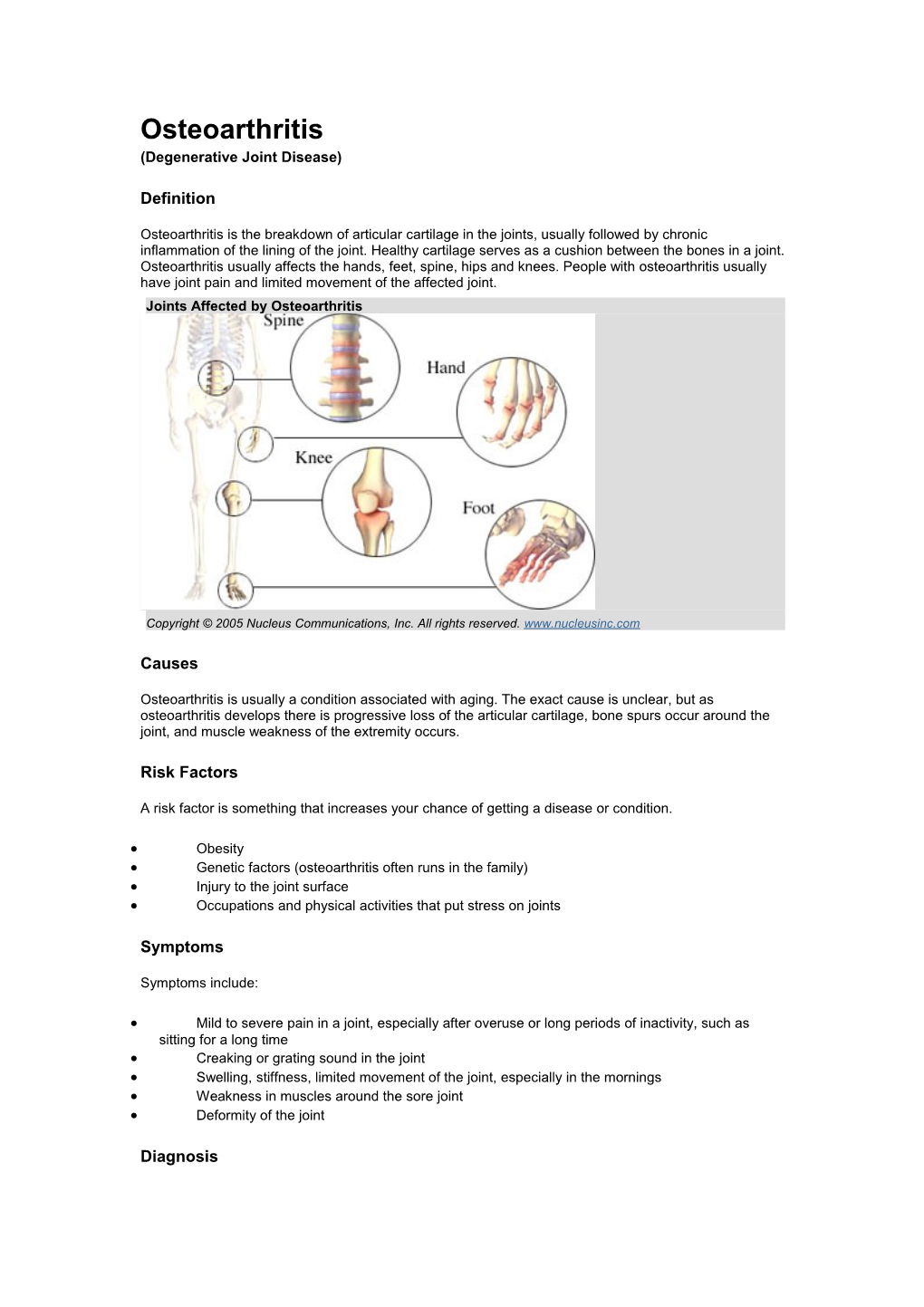
Osteoarthritis is the breakdown of articular cartilage in the joints, usually followed by chronic inflammation of the lining of the joint. Healthy cartilage serves as a cushion between the bones in a joint. Osteoarthritis usually affects the hands, feet, spine, hips and knees. People with osteoarthritis usually have joint pain and limited movement of the affected joint. Joints Affected by Osteoarthritis
Copyright © 2005 Nucleus Communications, Inc. All rights reserved. www.nucleusinc.com
Causes
Osteoarthritis is usually a condition associated with aging. The exact cause is unclear, but as osteoarthritis develops there is progressive loss of the articular cartilage, bone spurs occur around the joint, and muscle weakness of the extremity occurs.
Risk Factors
A risk factor is something that increases your chance of getting a disease or condition.
Obesity Genetic factors (osteoarthritis often runs in the family) Injury to the joint surface Occupations and physical activities that put stress on joints
Symptoms
Symptoms include:
Mild to severe pain in a joint, especially after overuse or long periods of inactivity, such as sitting for a long time Creaking or grating sound in the joint Swelling, stiffness, limited movement of the joint, especially in the mornings Weakness in muscles around the sore joint Deformity of the joint
Diagnosis The doctor will ask about your symptoms and medical history, and perform a physical exam.
Tests may include:
X-rays of the affected joints – to look for cartilage loss, signified by narrowing of the joint, bone damage, or bone spurs Blood tests – to rule out other medical conditions Arthrocentesis – removal of fluid from the joint for testing
Treatment
There is no treatment that absolutely stops the degeneration of cartilage or repairs cartilage that is already damaged. The goal of treatment is to reduce joint pain and inflammation and to improve joint function.
Treatments may include:
Medications
Over-the-counter pain medication – acetaminophen (Tylenol) and nonsteroidal anti- inflammatory drugs (NSAIDs) such as ibuprofen and naproxen (Advil, Aleve) Prescription pain relief medications - o Cox-2 inhibitors – celecoxib (Celebrex) and rofecoxib (Vioxx) o Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)- Arthrotec is a new NSAID that may reduce the risk for gastrointestinal bleeding
***Please Note: On September 30, 2004, Merck & Co., Inc. announced a voluntary withdrawal of Vioxx(R) (rofecoxib) from the U.S. and worldwide market due to safety concerns. A recent study showed a small but significant increased risk of cardiovascular events (such as heart attack) in patients taking the prescription medication. Vioxx(R) is a so-called "selective" non-steroidal anti- inflammatory drug (NSAID) specially designed to lower the risk of stomach irritation. It is commonly used in the treatment of acute and chronic pain associated with arthritis, menstruation and other conditions. Since Merck's withdrawal of Vioxx(R), evidence has come to light regarding similar dangers posed by the other popular selective NSAID, Celebrex(R) (cefecoxib), which is produced by Pfizer. Most physicians now question the wisdom of prescribing any medications from the COX-2 class.
Viscosupplementation – injection of a substance called hyaluronan into the joint, which helps to lubricate the joint Pain relief creams – capsaicin, methyl salicylate, and menthol
Dietary Supplements
There is some evidence that glucosamine and chondroitin may relieve pain and or decrease the progression of osteoarthritis. Fish oils have also been noted to reduce inflammation, although there is no scientific evidence to support this.
Alternative Treatments
Some clinicians report that acupuncture has been successful in reducing the pain of osteoarthritis. Hydrotherapy, or spa therapy, is an ancient therapy that uses mineral baths to relieve pain.
Mechanical Aids
Shoes with shock-absorbing soles can provide some relief while you are doing daily activities or exercising. Splints or braces help to properly align joints and distribute weight. Knee and wrist joints may benefit from elastic supports. A neck brace or corset may relieve back pain, and a firm mattress may help chronic back pain. Canes, crutches, walkers, and orthopedic shoes also can be of benefit to patients with advanced osteoarthritis of the lower extremity. Weight Reduction
Losing weight can lessen the stress on joints affected by osteoarthritis. A modest loss of five pounds can eliminate at least 15 pounds of stressful impact for each step taken and thus help the affected joint. The more weight lost, the greater the benefit.
Exercise and Physical Therapy
Strengthening the muscles supporting an arthritic joint (particularly the knee, lower back and neck) may decrease pain and help to absorb energy around the joint. Swimming and water aerobics are particularly good, because they don't put stress on the joint.
Assist Devices
If you are having difficulty getting around due to arthritis pain, your doctor might recommend that you install handrails and grips throughout your home. These are especially useful in the bathroom and shower. You may need elevated seats (including the toilet seats) if you're having difficulty rising after sitting.
Heat and Ice
Applying heat (with hot water bottles, heating pads, hot paraffin) helps joints and muscles to move more easily and can decrease pain, as can using ice packs after activity.
Steroids
When less potent pain relievers are ineffective, corticosteroid injections to the inflamed joint may be given. Because repeated cortisone injections can be harmful to the tissue and bones, they are reserved for patients with more pronounced symptoms.
Surgery
Surgery can:
Reposition bones to redistribute stress on the joint Replace joints Remove loose pieces of bone or cartilage from joints
Prevention
To reduce your chance of getting osteoarthritis:
Maintain a healthy weight. Do regular, gentle exercise, including walking, stretching, swimming, and yoga. Avoid repetitive motions and risky activities that may contribute to joint injury, especially after age 40. With advancing age certain activities may have to be dropped or modified but continue to be active.
RESOURCES:
American College of Rheumatology http://www.rheumatology.org
The Arthritis Foundation www.arthritis.org
Sources: National Institute of Arthritis and Musculoskeletal and Skin Disorders
Pathophysiology of osteoarthritis. Joint Bone Spine. 2000.