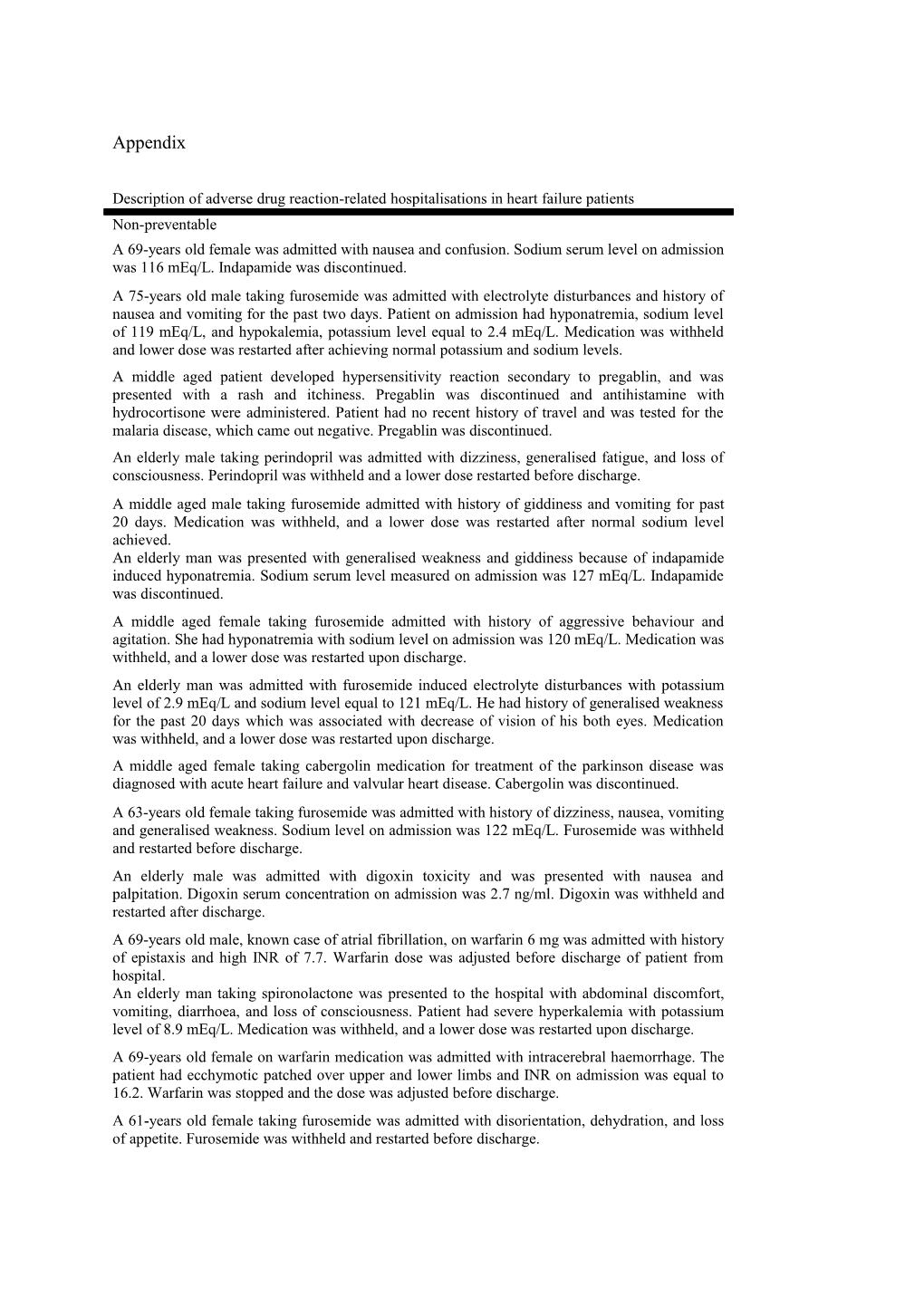
Appendix
Description of adverse drug reaction-related hospitalisations in heart failure patients Non-preventable A 69-years old female was admitted with nausea and confusion. Sodium serum level on admission was 116 mEq/L. Indapamide was discontinued. A 75-years old male taking furosemide was admitted with electrolyte disturbances and history of nausea and vomiting for the past two days. Patient on admission had hyponatremia, sodium level of 119 mEq/L, and hypokalemia, potassium level equal to 2.4 mEq/L. Medication was withheld and lower dose was restarted after achieving normal potassium and sodium levels. A middle aged patient developed hypersensitivity reaction secondary to pregablin, and was presented with a rash and itchiness. Pregablin was discontinued and antihistamine with hydrocortisone were administered. Patient had no recent history of travel and was tested for the malaria disease, which came out negative. Pregablin was discontinued. An elderly male taking perindopril was admitted with dizziness, generalised fatigue, and loss of consciousness. Perindopril was withheld and a lower dose restarted before discharge. A middle aged male taking furosemide admitted with history of giddiness and vomiting for past 20 days. Medication was withheld, and a lower dose was restarted after normal sodium level achieved. An elderly man was presented with generalised weakness and giddiness because of indapamide induced hyponatremia. Sodium serum level measured on admission was 127 mEq/L. Indapamide was discontinued. A middle aged female taking furosemide admitted with history of aggressive behaviour and agitation. She had hyponatremia with sodium level on admission was 120 mEq/L. Medication was withheld, and a lower dose was restarted upon discharge. An elderly man was admitted with furosemide induced electrolyte disturbances with potassium level of 2.9 mEq/L and sodium level equal to 121 mEq/L. He had history of generalised weakness for the past 20 days which was associated with decrease of vision of his both eyes. Medication was withheld, and a lower dose was restarted upon discharge. A middle aged female taking cabergolin medication for treatment of the parkinson disease was diagnosed with acute heart failure and valvular heart disease. Cabergolin was discontinued. A 63-years old female taking furosemide was admitted with history of dizziness, nausea, vomiting and generalised weakness. Sodium level on admission was 122 mEq/L. Furosemide was withheld and restarted before discharge. An elderly male was admitted with digoxin toxicity and was presented with nausea and palpitation. Digoxin serum concentration on admission was 2.7 ng/ml. Digoxin was withheld and restarted after discharge. A 69-years old male, known case of atrial fibrillation, on warfarin 6 mg was admitted with history of epistaxis and high INR of 7.7. Warfarin dose was adjusted before discharge of patient from hospital. An elderly man taking spironolactone was presented to the hospital with abdominal discomfort, vomiting, diarrhoea, and loss of consciousness. Patient had severe hyperkalemia with potassium level of 8.9 mEq/L. Medication was withheld, and a lower dose was restarted upon discharge. A 69-years old female on warfarin medication was admitted with intracerebral haemorrhage. The patient had ecchymotic patched over upper and lower limbs and INR on admission was equal to 16.2. Warfarin was stopped and the dose was adjusted before discharge. A 61-years old female taking furosemide was admitted with disorientation, dehydration, and loss of appetite. Furosemide was withheld and restarted before discharge. A middle aged male taking warfarin was admitted with dizziness and history of black stool. Patient had gastrointestinal bleeding which later developed hypotension, entered shock, and died. An elderly female taking furosemide was presented with drowsiness and history of poor oral intake. Serum potassium level on admission was 2.7 mEq/L, and serum sodium level was equal to 127 mEq/L. Furosemide was withheld and restarted before discharge. A middle aged male taking furosemide was admitted with dehydration and disorientation. Furosemide was withheld and restarted before discharge. An elderly male taking gliclazide was admitted with hypoglycaemia. The dose of medication was adjusted. A middle aged male taking aspirin was admitted with gastrointestinal bleeding. Blood transfusion was given, and medication was discontinued. Patient improved after stopping aspirin intake. A middle aged male on aspirin medication was admitted with gastric bleeding. Medication was discontinued, and the patient condition improved. A 62-years old female taking indapamide was admitted with nausea and vomiting. Indapamide was discontinued. Preventable An elderly female taking spironolactone was presented with confusion and decreased level of consciousness. Patient had severe hyperkalemia with potassium level of 8.9 mEq/L. Spironolactone was withheld and a lower dose was started before discharge. A 60-years old male who had taken diclofenac for knee pain, developed heart failure exacerbation, and was hospitalised with shortness of breath and peripheral oedema. N-terminal pro-brain natriuretic peptide on admission was equal to 506 pg/mL. Medication was discontinued. In a private clinic, a 40-years old male received diclofenac injection after which he developed anaphylactic reaction and exacerbation of decompensated HF. He was transferred to one of the hospitals with facial and leg swelling. N-terminal pro-brain natriuretic peptide on admission was equal to 7,484 pg/mL. A middle aged male was admitted with HF exacerbation. He was a known case of diabetes mellitus for more than 20 years and was treated with pioglitazone. This patient had a prior myocardial infarction and was a known case of HF. Pioglitazone was discontinued. A 63-years old male was developed HF exacerbation after receiving cortisone injection in a private clinic for his osteoarthritis condition. He was admitted to the cardiac unit with shortness of breath, pulmonary and peripheral oedema. An elderly man developed gastrointestinal bleeding and exacerbation of heart failure after taking the diclofenac medication orally. Medication was discontinued. An elderly man taking pioglitazone treatment for his diabetes mellitus condition was presented with exacerbation of HF. He had a history of myocardial infarction and continued taking pioglitazone which resulted in several past episodes of HF decompensation. Pioglitazone was discontinued. An elderly male developed HF exacerbation after taking diclofenac medication for his knee pain and was admitted to the cardiac unit with oedema, shortness of breath, and N-terminal pro-brain natriuretic peptide level of 3,738 pg/mL. Diclofenac was discontinued. An elderly man taking verapamil was admitted with decompensated HF. This patient was a known case of HF with systolic dysfunction. N-terminal pro-brain natriuretic peptide on admission was equal to 11,731 pg/mL. Verapamil was discontinued. A 63-years old male taking diclofenac for arthritis pain, was admitted with HF decompensation, acute pulmonary oedema, and shortness of breath. N-terminal pro-brain natriuretic peptide on admission was equal to 2, 478 pg/mL. Diclofenac was discontinued. An elderly man taking dutasteride medication was presented with exacerbation of HF. Later in hospital patient developed cardiogenic shock and died. A 63-years old male taking roziglitazone was admitted owed to decompensation of HF with shortness of breath, peripheral oedema, and NYHA functional class IV. Medication was discontinued, but patients condition deteriorated, and he was pronounced dead after three days of admission.