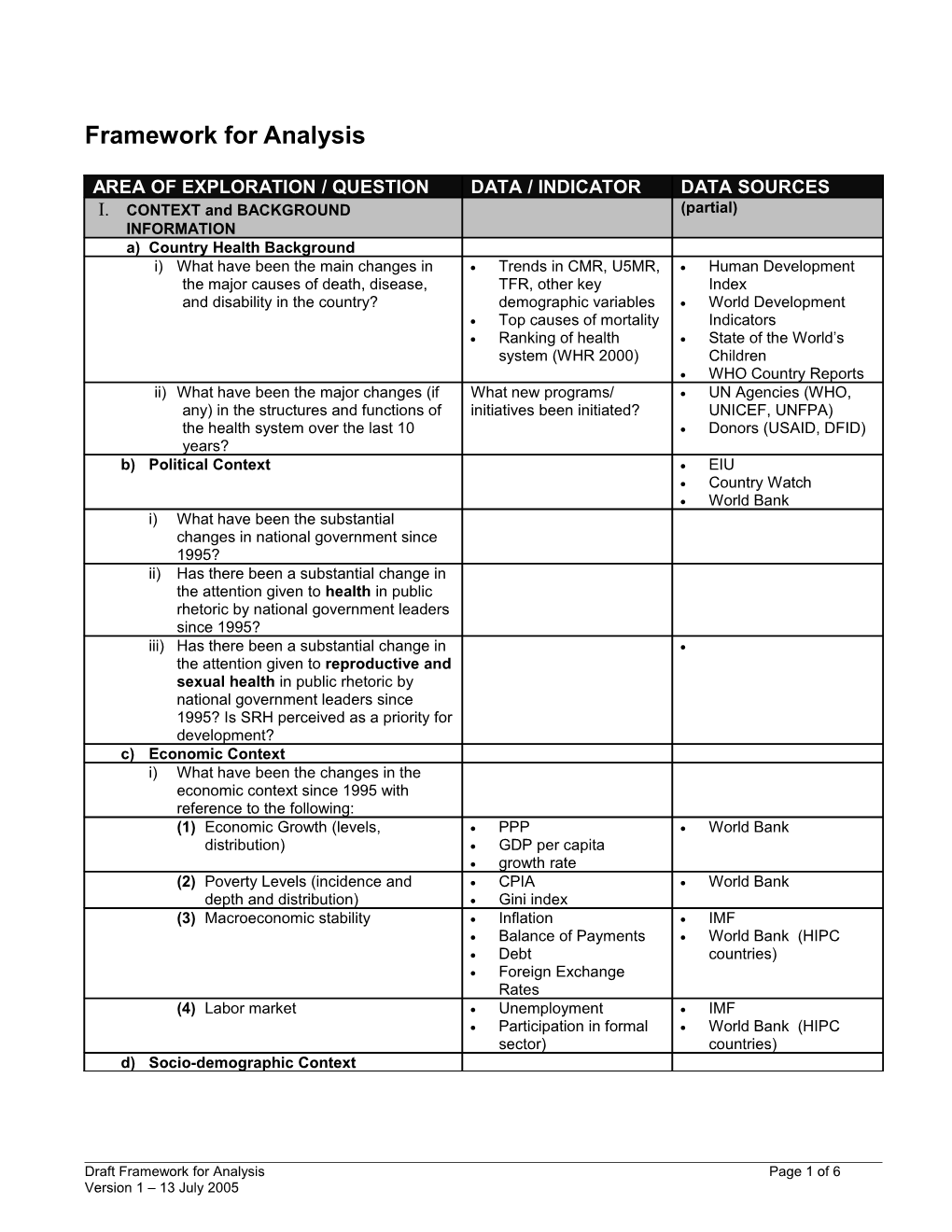
Framework for Analysis
AREA OF EXPLORATION / QUESTION DATA / INDICATOR DATA SOURCES I. CONTEXT and BACKGROUND (partial) INFORMATION a) Country Health Background i) What have been the main changes in Trends in CMR, U5MR, Human Development the major causes of death, disease, TFR, other key Index and disability in the country? demographic variables World Development Top causes of mortality Indicators Ranking of health State of the World’s system (WHR 2000) Children WHO Country Reports ii) What have been the major changes (if What new programs/ UN Agencies (WHO, any) in the structures and functions of initiatives been initiated? UNICEF, UNFPA) the health system over the last 10 Donors (USAID, DFID) years? b) Political Context EIU Country Watch World Bank i) What have been the substantial changes in national government since 1995? ii) Has there been a substantial change in the attention given to health in public rhetoric by national government leaders since 1995? iii) Has there been a substantial change in the attention given to reproductive and sexual health in public rhetoric by national government leaders since 1995? Is SRH perceived as a priority for development? c) Economic Context i) What have been the changes in the economic context since 1995 with reference to the following: (1) Economic Growth (levels, PPP World Bank distribution) GDP per capita growth rate (2) Poverty Levels (incidence and CPIA World Bank depth and distribution) Gini index (3) Macroeconomic stability Inflation IMF Balance of Payments World Bank (HIPC Debt countries) Foreign Exchange Rates (4) Labor market Unemployment IMF Participation in formal World Bank (HIPC sector) countries) d) Socio-demographic Context
Draft Framework for Analysis Page 1 of 6 Version 1 – 13 July 2005 i) What have been the substantial changes in socio-demographic context since 1995 with reference to the following: (1) Demographic transition and (By gender, minority status, Bureau of the Census urbanization religious/ethnic group, etc.) Family planning Population growth rates organizations / UNFPA Crude birth rates Crude death rates
(2) Migration (refugees, IDPs, UNHCR economic migrants) Global IDP Project IOM (3) Women's status in terms of political Percent women in UNStats power & participation, education parliamentary seats IPU and other social areas (gaps Education primary ICRW between men and women) completion rate, World’s Women Trends females & Stats (UNStats) Task Force 3 report on gender inequality (4) Education Access, availability, UN Stats quality Literacy rate
II. HEALTH OUTCOMES Country Rankings, Trends WHO a) MMR b) IMR Lancet child survival series State of the World’s Children (5 year intervals) c) Neonatal Mortality Lancet neonatal survival series d) Under 5 Mortality State of the World’s Children e) Life Expectancy UN Stats
III. HEALTH SERVICE OUTPUTS (Focus on reproductive health) a) Antenatal Coverage % of women who had DHS/MICS a live birth in the five (or WDI 3) years preceding the survey who received 2 or more antenatal care visits b) Skilled Birth Attendance % of live births DHS attended by a skilled WDI attendant (not including Other country-specific trained TBAs) in the surveys where DHS or five (or 3) years WDI data are not preceding the survey available % of live births taking place in a health facility in the five (or 3) years preceding the survey
Draft Framework for Analysis Page 2 of 6 Version 1 – 13 July 2005 c) HIV prevalence, incidence, access to ARVs WHO 3x5 website / UNAIDS Global Fund d) Health Services Utilization IV. PATTERN OF SERVICE DELIVERY AND FUNCTIONING OF HEALTH SYSTEM a) Financing i) Trends in financing since 1995 Proportion government MOH funding, external funding, Donor websites private expenditures WHO (1) Government Health Budget % of annual budget (2) Ratio of tertiary care spending to primary care spending (3) % of GDP for health (4) Total projected spending per capita (5) Total projected spending on health per capita (6) Total project spending on SRH? Is there evidence of rise/decrease over time? Can this be associated with any policy change? ii) Sources of Health Funding (1) Government (2) External (Bilateral, multilateral, NGO) (3) Private expenditures (cost recovery, user fees, out of pocket expenses) (4) How are available funds disbursed and managed? iii) Funding Restrictions (a) Donor conditionalities (any Donor sites relating to SRH) (b) Disease specific funding Global Fund RBM UNAIDS Stop TB Bilateral initiatives World Bank (c) Geographic area (urban/rural, MOH minority groups) (d) Is an increasing proportion of aid for health provided on- budget? iv) Innovative financing strategies (1) Health insurance schemes (2) Performance-based contracting (3) Franchising (4) Exemption plans (means testing) (5) Community level service provision V) HEALTHCARE INFRASTRUCTURE (1) Facilities (a) Since 1995 what have been the changes in public sector facilities providing SRH (Facilities to population ratios): (2) Human Resources WHO/HRH
Draft Framework for Analysis Page 3 of 6 Version 1 – 13 July 2005 (a) Since 1995 what have been the substantial changes (and reasons, if any) in the numbers and geographical distribution of staff providing SRH? (staff: population ration). (3) Service Delivery (1) Who is delivering reproductive health services, where and how? (2) What proportion of services is delivered by non-state actors? (3) How are communities engaged/involved in service provision? (degree of local level autonomy) ii) Ensuring access for the poor (1) How is access to public health services for the poor and vulnerable being facilitated? (2) If no public pro-poor services, are there examples of non-state actors taking on this role? If so, who and what?
Draft Framework for Analysis Page 4 of 6 Version 1 – 13 July 2005 Policy and Co-ordination i) National health policy (1) Is there a national health policy/framework, or is policy created on an ad hoc basis based on funding? How closely is the plan followed in implementation? (2) How is SRH profiled in the national health plan? (3) How are equity and poverty issues reflected in the national health plan? ii) SRH policy (1) Is there a sexual and reproductive health policy/framework, or is policy created on an ad hoc basis based on funding? How closely is the plan followed in implementation? (2) How are SRH interventions planned and managed, eg vertical programmes or an integrated approach? Is there a tension between vertical and integrated approaches? iii) Coordinating mechanisms (1) Is their a coordinating body for health and/or SRH, has is changed over time? (2) In addition to the MOH, what other ministries are involved in defining and implementing SRH policy issues? (3) How can the interaction with other ministries best be characterized? (4) What is the link between SRH and HIV/AIDS, both in terms of governance architecture and activities? iv) Relationship with national planning processes (PRSP) (3) How is the National health plan reflected in the PRSP? (4) How are SRH priorities reflected in the PRSP? (5) How has the PRSP affected sectoral planning processes? v) SRH Partners (6) Who are the major health partners working in SRH? (7) Which elements of the Global Strategy on Reproductive Health do donors emphasize? (3) What impact, if any, have Paris/Rome harmonization and alignment processes had on donor co- ordination?
Draft Framework for Analysis Page 5 of 6 Version 1 – 13 July 2005 Draft Framework for Analysis Page 6 of 6 Version 1 – 13 July 2005