Rajiv Gandhi University of Health Sciences, Karnataka
SYNOPSIS
FOR REGISTERATION OF SUBJECT FOR DISSERTATION
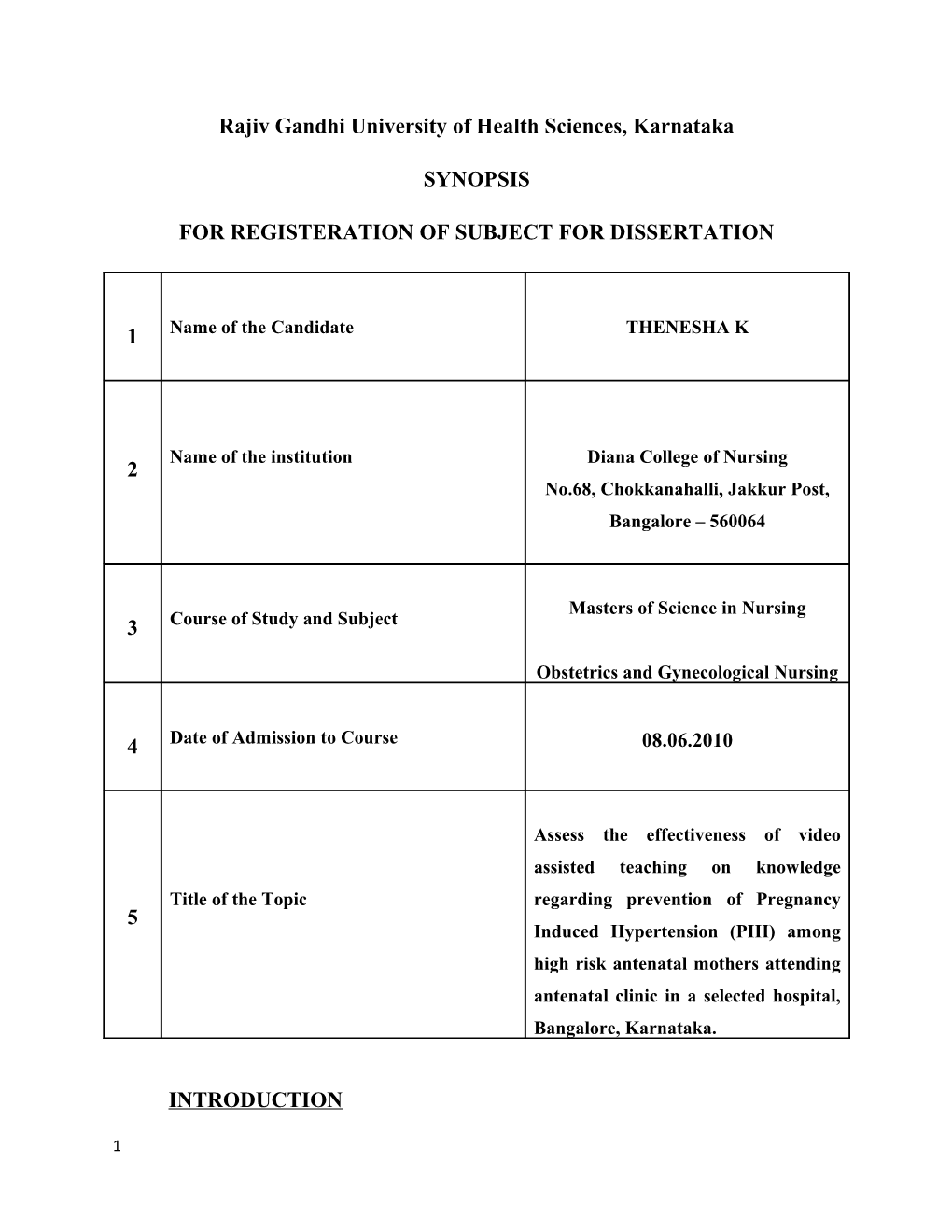
1 Name of the Candidate THENESHA K
Name of the institution Diana College of Nursing 2 No.68, Chokkanahalli, Jakkur Post, Bangalore – 560064
Masters of Science in Nursing 3 Course of Study and Subject
Obstetrics and Gynecological Nursing
4 Date of Admission to Course 08.06.2010
Assess the effectiveness of video assisted teaching on knowledge Title of the Topic regarding prevention of Pregnancy 5 Induced Hypertension (PIH) among high risk antenatal mothers attending antenatal clinic in a selected hospital, Bangalore, Karnataka.
INTRODUCTION
1 Pregnancy is a normal process but it is unique and boon to every woman. It is one of the
wonderful and noble services imposed by nature. The body undergoes enormous
functional changes during pregnancy and the functioning is altered in order to nourish the
mother, baby and to have normal delivery. Normal Pregnancy is dramatic and often
underestimated. The timing and intensity of the changes vary between systems but all are
designed to enable the women to nurture to the fetus and to prepare her body for labor
and lactation. Most of the women may not have many problems during pregnancy, but
the unlucky ones, face problems related to pregnancy and child birth. In developing
countries, pregnancy and child birth are some of the leading causes of death for women in
the reproductive age group. Yet, the fate of these women and children is too often
overlooked or ignored.1
The WHO slogan for 2005 “Make Every mother and child count”, reflects the reality
that today, Government and the International Community needs to make the health of the
women and children the top priority.2
Various Complications can develop during the course of the pregnancy and can affect the
health and well being of the mother and fetus, as well as the outcome of the pregnancy.
With early recognition and today’s advanced technology, the incidence of maternal
mortality resulting from complication is declining.3
Common Health Disorders complicating pregnancy are PIH, GDM, Cardiac disease,
renal disease and jaundice in pregnancy. A report “Global statistics – PIH” estimated
that global prevalence of PIH among pregnant women is 13%.4
2 PIH is more common in a woman's first pregnancy and in women whose mothers or
sisters had PIH. The risk of PIH is higher in women carrying multiple babies, in teenage
mothers and in women older than age 40. Other women at risk include those who had
high blood pressure or kidney disease before they became pregnant. The exact cause of
PIH isn't known.5
High blood pressure in pregnancy (hypertension) is a very serious complication. It puts
both the mother and the fetus at risk for a number of problems. Hypertension can exist in
several different forms. One of these is the preeclampsia-eclampsia continuum (also
called pregnancy-induced hypertension or PIH). In this type of hypertension, high blood
pressure is first noted sometime after week 20 of pregnancy and is accompanied by
protein in the urine and swelling. Chronic hypertension is another form of hypertension.
It usually exists before pregnancy or may develop before week 20 of pregnancy.6
Nurses have a vital role in the successful operation and ultimate outcome of antenatal
high risk mothers’ care. The ultimate goal of nurse is to prevent hypertensive disorders of
pregnancy or to assist in early diagnosis and appropriate treatment of these disorders to
maximize outcome. Preeclampsia is a much study disease of pregnancy but the triggering
factor remains unknown. This makes prevention difficult; however, because research
indicates that several factors, such as early appropriate prenatal care, adequate fluid
intake and optimal nutrition plays important roles, the nurse should include these in the
prenatal instructions. When a mother develops preeclampsia during pregnancy, the goal
becomes the prevention of eclampsia and uteroplacental insufficiency while attempting to
facilitate fetal maturity.7
NEED FOR THE STUDY
3 PIH is a multi system syndrome characterized by vasoconstriction, metabolic changes,
and endothelial dysfunction, activation of coagulation cascade and increase inflammatory
response. PIH contributes to (MMR) Maternal Mortality Rate, Prenatal mortality rate and
still birth with variations to geographical location and race.8
Hypertensive disorders of pregnancy are frequent cause of maternal and fetal morbidity
and mortality, the most common being preeclampsia and eclampsia. Pregnant mothers
should be screened routinely. Early recognition and prompt care form a multidisciplinary
service, including obstetrics, cardiology, and hypertensive disorders of pregnancy reflect
endometrial endothelial dysfunction and abnormalities and systematic endothelial
dysfunction, which might predict future cardiovascular disease in these young women,
prompting early preventive measures.9
In a study it was stated that in most of the countries, PIH is the single largest cause of
maternal mortality. WHO (2000) stated that maternal mortality is said to be an indicator
of social inequity and discrimination against women. The Goal of national health policy
was to reduce maternal mortality rate to 100 / 1, 00,000 like births by 2010.10
In Global, Pre-eclampsia or PIH is a condition that affects up to 80% of pregnancies
every year and is among the leading cause of maternal and fetal illness worldwide .The
incidence of pre-eclampsia and eclampsia was higher in the developing countries with the
highest rate reported for pre-eclampsia as 7.1% in Zimbabwe and for eclampsia as 0.81%
deliveries in Columbia. The Maternal and fetal mortality rate was 0.4% for pre-eclampsia
reported in Magpies and as 6.1% for eclampsia reported from Columbia. Hypertension
disorders of the pregnancy are the common and direct cause of maternal deaths in South
4 Africa. 19.1% of maternal deaths in a three year period (2002-2004) were associated with
hypertensive disorders of pregnancy.11
A study was conducted in US, stated that pregnancy associated hypertension is a leading
cause of maternal death. The study reported Maternal death rate in 2005 was 9.8/1,
00,000.12
In national level, the developing countries like India, the maternal and prenatal mortality
rates are still high. It is of great concern to suggest mothers to improve the health status
of the Mother and the child. It is well accepted that only a healthy mother can give birth
to a healthy baby. In 2003, Maternal mortality has declined to 301/1, 00,000 live births.13
A study was conducted on comprehensive antenatal care and prevention of pregnancy
induced hypertension. Hypertensive disorders in pregnancy are a universally common
disease. How pregnancy induces and aggravates hypertension is still not understood fully.
The incidence of pregnancy induced hypertension (PIH) in India ranges from 5-15%. In
Primi mothers 16% and Multi mothers 7%. It causes IUGR leading to low birth weights.
It increases the maternal mortality by 10-15% and the prenatal mortality and morbidity
by 15 to 25%.14
PIH can be detected early during regular prenatal visits, which is one of the reasons they
are so very important. PIH can be result in preterm baby, a stillborn baby and a baby who
has growth retardation (IUGR). 15
The pregnant woman's interview at her first visit the health care provider is conducted by
the nurse, who obtains the data necessary to begin the high-risk screening. The physician
5 or midwife caring for a pregnant woman should review the prenatal assessment sheet,
order lab data, and obtain ultrasounds to determine if any risk factors are present. If it is
determined that a woman has a high-risk pregnancy, she should be referred to a
perinatologist for advanced care. This is the specialist who establishes and implements
the medical regimen needed for the particular maternal/fetal complication and the inter-
disciplinary team associated with the prenatal center works in its management. The
prenatal team usually comprises a nutritionist, social worker, nurse educators, geneticists,
ultrasonographers, and additional nursing staff who are responsible for the monitoring
and supervising of ongoing team care of the patient.16
6 A nursing care program was conducted to reduce the role of pregnancy-induced
hypertension in patients with clinical complications. The study was conducted to
investigate the predictability of complications of pregnancy induced hypertension nursing
program. Methods to confirm the diagnosis of 400 patients with PIH were randomly
divided into the nursing care intervention group and control group of 200 patients in the
control group received routine treatment and care, nursing care intervention study group
in addition to conventional treatment and care, the law of development of the disease
given under nursing care interventions. The study group maternal complications
(eclampsia, placental abruption, postpartum hemorrhage, acute renal failure, fetal death,
neonatal asphyxia, etc.) compared with the control group, the incidence of the differences
were statistically significant (P <0.01), study group was significantly lower than the
control group. It was concluded as PIH nursing intervention for patients with
predictability measures can significantly reduce the incidence of maternal
complications.17
A study was conducted to determine the health education in enhancing the self
care agency of pregnant women among 30 antenatal mothers in Turkey. The study
concluded that after health education the self care agency scores of the pregnant women
increased significantly.18
It was felt that maternal mortality rate from high risk factors during pregnancy could not
diminish until their knowledge and attitude where understood and brought more into line
with the norms of modern obstetric care. The investigator during her clinical experience
noted many high risk antenatal mothers who have inadequate knowledge. The
investigator planned to assess their knowledge regarding prevention of Pregnancy
7 Induced Hypertension and she also felt the immense need to provide video assisted
teaching programme for the high risk mothers.
REVIEW OF LITERATURE :
Review of literature is defined as a broad, comprehensive, in-depth, systematic and
critical review of scholarly publications, unpublished scholarly print materials and audio
visual materials.19
Literature review for the present study has been collected and presented under the
following headings.
1. Literature related to incidence and prevalence of PIH.
2. Literature related to the management of PIH.
3. Literature related to the complications of PIH.
4. Literature related to prevention of PIH.
5. Literature related to effectiveness of teaching program on PIH.
Literature related to incidence and prevalence of PIH:
Worldwide, it is estimated that 5, 29,000 women die yearly from complication of
pregnancy and childbirth, about one women every minute. The incidence of the pre-
eclampsia in hospital practice varies widely from 5-15%. The incidence in primigravidae
8 is about 10% and in multigravidae 5%. Imperfect documentation and lack of uniformity
in the diagnostic criteria are the responsible factors in variation of its frequency. In the
developing countries, the incidence is expected to be higher. Comparative low figures in
the hospital statistics is due to inclusion of only severe degree of the syndrome, the minor
ones being ignored.20
It was reported that the rate of PIH has risen steadily by about 30% to 40% since 1990.
Now it is 38.8/1000 live births.21
In India 10% to 30% of pregnancies belong to the high risk category. About 5,85,000
women die each year from pregnancy related census, 99% of them are from the
developing countries, out of each 80% of the deaths are due to direct obstetrics causes
(such as hemorrhage, infection, hypertension, abortion) and 20% are due to indirect
causes ( such as anemia, malaria, hepatitis, AIDS). Secure maternal mortality is 6 to 10
times more frequent than maternal mortality. WHO estimates that 95% of these deaths
are handicaps is avoidable.22
According to Indian Council of medical researchable task for a study (2002) in India
where maternal mortality rate is 582/1, 00,000 live birth and hypertensive disorders were
responsible for 24% of all maternal deaths.23
A retrospective study to determine the maternal outcome in pregnant women with
hypertensive disorder. A retrospective analysis was undertaken on 255 consecutive cases
of PIH. Of the 255 cases 11% had eclamptic convulsion, 11% of women demonstrated to
have HELLP syndrome.24
Literature related to the management of PIH:
9 Ideally all patients of pre-eclampsia are to be admitted in the hospital for effective
supervision and treatment. There is no place of domiciliary treatment in an established
case of pre-eclampsia. However, in some centers cases of preeclampsia are managed in
the day care unit (p 639). In the developing countries where the prevalence of pre-
eclampsia is more and hospital facilities are meagre, there is no alternative but to put the
uncomplicated mild pre-eclampsias in domiciliary treatment regime. Rest, high protein
diet and mild sedative at bed time are prescribed and the patient is investigated and
checked after one week or even earlier. If treatment fails, the patient is to be admitted. It
is essential that she should be warned against the ominous symptoms such as headache,
visual disturbances, vomiting, epigastric pain or scanty urine.25
A study was conducted about the short and long term strategies for the management of
hypertensive disorders of pregnancy. In this study, the main focus was given on recent
developments in the prediction and pathogenesis of these disorders, prevention of
preeclampsia and current strategies for the treatment of hypertension in pregnancy. It also
explores the evidence relating adverse pregnancy outcome to an increased future risk of
cardiovascular disease and potential strategies to minimize this risk.26
A study was conducted about “A comparison of walking versus stretching exercise to
reduce the incidence of preeclampsia: a randomized clinical trial”. Women were
randomized to either the walking group (n=41) or the stretching group (n=38). The
walkers exercised an average of 36 (SD, 6) minutes at 18 weeks gestation, 34 (SD, 7)
10 minutes at 28 week of the intervention. Equally on average, the stretching group
exercised 4 (SD, 2) times a week at 18 weeks gestation, 5 (SD, 1) times a week at 28
weeks gestation. The incidence of preeclampsia was 14.6% (95% CI, 0.07 to 13.8) among
the stretchers. The mean transferring level, an antioxidant marker, was significantly
higher in the stretching group mean (412 mg/dL, 95%CI, 389 to 435) than the walkers at
the time of labor (mean=368 g/dL, 95%CI, 346 to 391) (P=0.05). Regular stretching
exercise may promote endogenous antioxidants among women at risk for preeclampsia.27
Literature related to the complications of PIH:
Pregnancy induced hypertension may develop into eclampsia, the occurrence of seizures.
Fetal complications may occur because of prematurity at time of delivery.28
A study was conducted on supplementation of Vitamins C and E to prevent
complications of pregnancy – associated hypertension. A total of 10,154 women
underwent randomization. Two groups were similar with respective baseline
characteristics and adherence to the study drug. Outcome data were available for 9969
women. There was no significant difference between the vitamin and placebo groups in
the rates of the primary outcome (6.1% & 5.67% respectively); relative risk 1.07; 95%
CI, 0.93 to 1.24). Vitamins C and E supplementation initiated in the 9 to 16th week of
pregnancy in an unselected cohort of low risk, nulliparous women did not reduce the rate
of adverse maternal or prenatal outcomes related pregnancy associated hypertension.29
11 A study was conducted on pregnancy induced hypertension complicated acute
disseminated intravascular coagulation with the clinical analysis of 26 cases. In 26
patients with PIH complicated acute DIC, 7 cases died (26.92%), while 17 neonates died
(58.62%) in 29 neonates (3 cases were twin pregnancy). Caesarean section and
hysterectomy were performed on 7 cases respectively; including 4 cases underwent both
of them. The causative factors of PIH complicated acute DIC included placental
abruption (7 cases), amniotic fluid embolism (4 cases), eclamptic seizure (4 cases),
surgical injury (7 cases) and bleeding (4 cases). The conclusion was there are close
relationship between PIH and DIC, PIH complicated acute DIC is the major cause of
maternal and prenatal mortality, special attention should be paid on preventing DIC for
PIH.30
A study was conducted on investigating the risk of hypertension shortly after pregnancies
complicated by preeclampsia. Women with preeclampsia were significantly more likely
than controls to have hypertension (adjusted odds ratio, 13.92; 95% CI, 5.04-66.46;
P<.001) preeclampsia, may provide opportunities to identify women at risk for
cardiovascular morbidity years before the onset of disease, allowing a window for
prevention and intervention.31
A study was conducted in Ohio, to compare the frequency of the adverse fetal outcome in
women who developed PIH with or without Protienuria. The study was compared with
598 pre-eclamptic mothers and normotensive mothers. The findings revealed that in
12 women who have pre-eclampsia has increased the rate of preterm delivery (25%) and
delivery of small for gestational age (20.8%) infant.32
A study was conducted on incidence of pregnancy induced hypertension and the effects
of mother and fetus in Shangai. There were 158,790 deliveries in ten years. The total
numbers of PIH were 8,852 cases. The incidence of PIH was 5.57%. The rate of mild,
moderate and severe PIH was 55.83%, 29.39%, and 14.78% respectively. There were 114
cases (1.29%) complicated with preeclampsia. The rate if caesarean section of placenta
0.52%, heart failure 0.34%, renal failure 0.20%, DIC 0.03%, maternal death one cases.
The prenatal death 66 occurred in cases (7.18@1000) in which fetal death 48 cases, still
birth 12 and neonatal death. The incidence of PIH and the rate of prenatal infant death
can be reduced by strengthen antenatal monitoring, prevention, early diagnosis and
treatment of PIH.33
Literature related to prevention of PIH:
Although there is no known way to prevent preeclampsia, it is important for all pregnant
women to start prenatal care early and continue it through the pregnancy. This allows the
health care provider to find and treat conditions such as preeclampsia early. Proper
prenatal care is essential. At each pregnancy checkup, the health care provider will check
the weight, blood pressure, and urine (through a urine dipstick test) to screen for
preeclampsia.34
13 As with any pregnancy, a good prenatal diet full of vitamins, antioxidants, minerals, and
the basic food groups is important. Cutting back on processed foods, refined sugars, and
cutting out caffeine, alcohol, and any medication not prescribed by a doctor is essential.
Talk to your health care provider before taking any supplements, including herbal
preparations.35
A study was conducted on calcium supplementation during pregnancy for preventing
hypertensive disorders and related problems. In this study preeclampsia and eclampsia
are common causes of seriously morbidity and death. Calcium supplementation may
reduce the risk of preeclampsia through a number of mechanisms, and may help to
prevent preterm birth. Calcium supplementation appears to approximately halve the risk
of preeclampsia, to reduce the high risk of preterm birth and to reduce the rate of
occurrence the composite outcome ‘death or seriously morbidity’. There were no other
clear benefits, or harms.36
A study was conducted regarding regional differences in prevention of pregnancy
induced hypertension. In this review, it is found that the underlying cause of
preeclampsia and the result of clinical trials performed to prevent this disease, that the
causes and strategies to prevent preeclampsia are different in developed and developing
countries. It also suggests that establishment of an adequate prenatal care is the only
effective way to reduce the incidence of preeclampsia in population from developing
countries, especially in women at high risk of pregnancy induced hypertension.37
14 A study was conducted about low dose acetylsalicylic acid in prevention of pregnancy
induced hypertension and intrauterine growth retardation in women with bilateral uterine
artery notches. Forty three women on acetylsalicylic acid and 43 on placebo were
successfully followed up. The use of acetylsalicylic acid was associated with statistically
significant reduction in the incidence of pregnancy induced hypertension (11.6% vs.
37.2%, RR=0.31, 95% CI0.13 – 0.78) and preeclampsia (4.7% vs. 23.3%, RR=0.2, 95%
CI 0.05-0.86). Acetylsalicylic acid was not associated with excess risk of maternal or
fetal bleeding. In women rated in Doppler velocimetry waveform analysis to be at high
risk of preeclampsia, low dose acetylsalicylic acid reduces the incidence of pregnancy
induced hypertension and especially proteinuric preeclampsia.38
Literature related to effectiveness of teaching program on PIH:
A study was conducted to assess the efficacy and acceptability of a patient held pictorial
card aimed at raising awareness and appropriate health seeking behavior in response to
prodormal symptoms of imminent eclampsia. Pictorial cards were issued to antenatal
clinics and used to give instruction and advice to the women. Mothers were surveyed
before and after the introduction of the cards. The study concluded that mothers’
awareness and response to symptoms improved significantly and there was a marked
drop in eclampsia incidence.39
A descriptive exploratory study was conducted with aimed at identifying the factors that
are associated with preeclampsia and assessing the quality of midwifery care during labor
in women with preeclampsia in South Africa. The study revealed that women affected
15 with preeclampsia delayed in attending the antenatal clinic resulting in the control of the
disease being difficult. Based on the findings of the study, it is recommended that health
education on prevention of preeclampsia should be done on an ongoing process, while
carriers for mothers should be given in service education program.40
A study was conducted on Evaluation of a structured teaching program on pregnancy
induced hypertension treatment and teaching program in general practice. 10 primary
health care practices. From each practice 20 women (30 to 60 years old, mean of the last
two blood pressure measurements at or above 160 and/or 95 mmHg) were randomly
selected; in 5 practices these women were to participate in the treatment and teaching
program me; in the remaining 5 practices hypertension care was continued without the
availability of such a program me (controls). Of the 100 control women 26 and of the
100 intervention women 14 were lost to observation; 46 women had agreed to participate
in the programme. The mean number of prescribed antihypertensive agents per women
decreased in the intervention group (1.8 +/- 1.3 at baseline, vs 1.2 +/- 1.2 at follow-up)
compared to the control group (1.6 +/- 1.3 vs 1.8 +/- 1.6); difference 0.8 (95% CI 0.4 to
1.1), p < 0.0001. In the control group 9% and in the intervention group 33% of women
had documented reductions of body weight (p < 0.0001). Blood pressure decreased in the
intervention group (162 +/- 14/100 +/- 7 mmHg at baseline, vs 154 +/- 16/95 +/- 9 mmHg
at follow-up) compared to the control group (161 +/- 13/98 +/- 7 mmHg vs 158 +/- 18/96
+/- 11 mmHg); differences for systolic blood pressure 5 (95% CI 0 to 10) mmHg, p =
0.071; for diastolic blood pressure 4 (1 to 7) mmHg, p = 0.018.it was concluded that the
introduction of a structured pregnancy hypertension treatment and teaching program me
16 in general practice may lead to significant improvements of pregnancy induced
hypertension care.41
Statement of the Problem
Assess the effectiveness of video assisted teaching on knowledge regarding prevention of
Pregnancy Induced Hypertension (PIH) among high risk antenatal mothers attending
antenatal clinic in a selected hospital, Bangalore, Karnataka.
Objectives
To assess the knowledge on Prevention of Pregnancy Induced Hypertension
among high risk antenatal mothers before intervention.
To assess the effectiveness of video assisted teaching module on prevention of
Pregnancy Induced Hypertension among high risk antenatal mothers.
To find the association between post-test knowledge scores on prevention of
Pregnancy Induced Hypertension among high risk antenatal mothers and their
selected demographic variables.
Operational definition
Effectiveness
17 Effectiveness refers to significant gain in the knowledge as determined by the statistical
difference in pre-test and post-test scores on prevention of pregnancy induced
hypertension among high risk antenatal mothers attending antenatal clinic in a selected
hospital, Bangalore, Karnataka.
Pregnancy Induced Hypertension (PIH)
PIH is a multi system disorder of unknown etiology characterized by development of HT
to the extent of 140/90 mmHg or more with proteinuria, induced by pregnancy after the
20th weeks in a previously normotensive and non- proteinuric women.
Video Assisting Teaching
It refers to the planned video teaching provided on prevention of PIH to high risk
antenatal mothers attending antenatal clinic. It consists of video clippings related to
introduction, meaning, signs and symptoms, and preventive measures such as regular
antenatal check up, diet, calcium supplementation, exercises, activity, relaxation
techniques, rest and sleep.
Prevention of Pregnancy Induced Hypertension
It refers to measures taken by the antenatal mothers to prevent pregnancy induced
hypertension. These measures include regular antenatal check up, diet, calcium
supplementation, exercises, activity, relaxation techniques, rest and sleep.
High Risk Mothers
High risk antenatal refers to antenatal mothers associated with certain conditions or risk
factors that predispose the mother to develop Pregnancy Induced Hypertension. The risk
18 factors associated with Pregnancy Induced Hypertension are young and elderly
primigravida, family history of hypertension, placental abnormalities, genetic disorders
and pre-existing vascular or renal disease.
Assumptions:
High risk antenatal mothers may not have adequate knowledge regarding the
prevention of Pregnancy Induced Hypertension.
Video assisted teaching module may enhance the knowledge of the high risk mothers
on prevention of Pregnancy Induced Hypertension.
Hypothesis :
H1: There will be a significant difference between pre-test and post-test knowledge
scores on prevention of Pregnancy Induced Hypertension among high risk antenatal
mothers.
H2: There will be a significant association between post-test knowledge scores on
prevention of Pregnancy Induced Hypertension among high risk antenatal mothers and
their selected demographic variables.
7. Materials and methods
19 7.1. Source of Data Data will be collected from the high risk antenatal mothers’ attending antenatal clinic, Bangalore, Karnataka. 7.2. Method of data collection Pre-experimental design with one group pre-test post- Research Design test approach to assess the effectiveness of video assisted teaching on knowledge on prevention of Pregnancy Induced Hypertension (PIH) among high risk antenatal mothers.
Setting of the Study Antenatal clinic in a selected hospital, Bangalore, Karnataka.
Population The population will be high risk antenatal mothers.
Antenatal mothers who are at high risk for PIH attending Sample antenatal clinic in a selected hospital, Bangalore, Karnataka.
Sample Size The sample size will be 30 high risk antenatal mothers.
Sampling Technique Purposive sampling technique will be used to select the high risk antenatal mothers attending antenatal clinic, Bangalore, Karnataka.
The study will include mothers: Inclusion Criteria o who are willing to participate in the study. o who are able to understand Kannada or English.
20 o who will be available at the time of data collection period.
Exclusion Criteria The study will exclude mothers: o Who were professionals of medical and nursing field. o mothers with associated complications.
Tools Tools will be divided in following sections: Section A: Inventory to screen high risk antenatal mothers. Section B: Structured questionnaire to assess the socio demographic variables. Section C: Structured knowledge interview questionnaire to assess the knowledge on prevention of PIH among the high risk antenatal mothers.
Prior to the data collection the investigator will obtain Data Collection permission from the concern authorities of the antenatal clinic, Bangalore, Karnataka. The investigator herself will collect further data collection before and after intervention.
Descriptive and inferential statistics will be used for data analysis. The collected data will be organized, tabulated Data Analysis & Data Presentation and analyzed by using descriptive statistic such as percentage, mean and standard deviation. The inferential
21 statistics such as chi-square test and paired‘t’ test will be used. The findings will be presented in the form of bar diagram, pie / sector and tables.
7.3. Does the study require any investigations or interventions to be conducted on
patients or other humans or animals?
Yes, Pre-test and post-test will be conducted among the antenatal mothers who are at
high risk of PIH before and after intervention.
7.4. Has ethical clearance been obtained?
Yes, informed consent will be obtained from concerned authority of institution and prior
to study. Privacy, confidentially and anonymity will be guarded. Scientific objectivity of
the study will be maintained with honesty and impartiality.
22 Ethical Committee
Assess the effectiveness of video assisted teaching on knowledge regarding prevention of Title of the topic Pregnancy Induced Hypertension (PIH) among high risk antenatal mothers attending antenatal clinic in a selected hospital, Bangalore, Karnataka.
Name of the candidate Miss. THENESHA K
Masters of Science in Nursing Course and the subject Obstetrics and Gynecological Nursing
Prof. Kalaivani Name of the Guide Head of the Department Obstetrics and Gynecological nursing Diana College of Nursing Bangalore – 64
Ethical Committee Approved
23 Members of Ethical Committee
1. Prof. Veda Vivek,
Principal and Head of Department,
Department of Community Health Nursing,
Diana College of Nursing, Bangalore – 64.
2. Prof. Elizabeth Dora,
Head of the Department,
Department of Child Health Nursing,
Diana College of Nursing, Bangalore – 64.
3. Prof. Kalaivani,
Head of the Department,
Department of Obstetrics and Gynecological Nursing,
Diana College of Nursing, Bangalore – 64.
4. Prof. Vasantha Chitra,
Head of the Department,
Department of Medical Surgical Nursing,
Diana College of Nursing, Bangalore – 64.
24 5. Prof. Surendra,
Biostatistician, GKVK, Jakkur, Bangalore-64.
6 Signature of the candidate
7 Remarks of the Guide The research topic selected for the candidate is suitable as it is selected for the antenatal mothers who are at high risk for PIH. There is a need to assess the knowledge and to provide adequate information regarding prevention of PIH among high risk antenatal mothers.
8 Name and Designation of Guide (In block letters) Prof. Kalaivani, Head of the Department, Obstetrics and Gynecological Nursing, Diana college of Nursing, Bangalore – 64.
25 Signature
9 Head of the Department Prof. Kalaivani, Head of the Department, Obstetrics and Gynecological Nursing, Diana college of Nursing, Bangalore – 64.
Signature
Remarks of the Chairman & The topic selected for the candidate is 10 Principal researchable and feasible and forwarded for needful action.
Signature
26 BIBILIOGRAPHY/REFERENCES
1. Dr. Satish Goel, Pregnancy & Child Care, Ist edition, Diamond Pocket Books (P) Ltd, pp 69 to
72.
2. Stokowski, Laura A. RN, and MS. Advances in Neonatal Care: June 2005 - Volume 5 - Issue
3 - p 124.
27 3. Annamma Jacob, A Comprehensive text book of midwifery. 3rd Edition. Jaypee Brothers
2009. pp 319-320.
4. SeonAe Yeo, RNC, PhD; Pamela J. Wells, MSN; Edith C. Kieffer, PhD; George H. Nolan,
MD, MP. preeclampsia among hispanic women in a detroit health system, Ethnicity &
Disease, Volume 17, Winter 2007, pp 118.
5. Norman A. Beischer, Eric V. Mackay, Paul Colditz. Obstetrics and the newborn, IIIrd
edtion, Saunders publications.pp 207-209.
6. Bennett, V.R. & Brown, C.K (1993), “Myles text book for midwifes”, (Eleventh edition), Edin burg: Churchill Livingston.
7. Elizabeth Stepp Gilbert, Manual of High risk Pregnancy and Delivery, IVth Edition, Elsevier
publications. pp 485.
8. Duckitt K, Harrington D. Risk factors for pre-eclampsia at antenatal booking:
systematic review of controlled studies. BMJ. Mar 12 2005;330(7491):565.
9. Duley L. Pre-eclampsia and the hypertensive disorders of pregnancy. Br Med
Bull. 2003;67:161-76.
10. Chang J, Elam-Evans LD, Berg CJ, Herndon J, Flowers L, Seed KA, et al. Pregnancy-
related mortality surveillance--United States, 1991--1999. MMWR Surveill Summ. Feb
21 2003;52(2):1-8
28 11. Lopa Banerjee, The Dangers of Preeclampsia and Eclampsia, Jan 22, 2010, pp 14.
12. Berg, Cynthia J. MD, MPH; Callaghan, William M. MD that pregnancy associated hypertension is a leading cause of maternal death Obstetrics & Gynecology: Dec 2010 - Volume
116 - Issue 6 - pp 1302-1309.
13. Theodore H. Tulchinsky, Elena Varavikova, The new public health, II nd edition, Elsevier
Academic Press publications, pp 224-225.
14. Laxmi Bhosale, D Padia, Harish Malhotra,Deepti Thakkar, HS Palep, KM Algotar. comprehensive antenatal care and prevention of pregnancy induced hypertension.Dept. of Obst. and Gynaecology.
15. Dutta, D.C. (2001), “Textbook of Obstetrics”, Jan.81 (1):25-30 New Central Agency (p)
Calcutta.
16. Olds, Sally B., London, Marcia L., and Ladewig, Patricia A. Maternal-Newborn Nursing: A
Family and Community-Based Approach. Upper Saddle River, NJ: Prentice Hall Health, 2000.
17. Zhao Wenjing, Zhang Yaping. Predictive nursing program nursing care of trauma patients.
Journal of Nursing, 2000, 35 (5): 16.
18. Pasinlioglo T. Health education for pregnant women. Patient educ couns. 2009; Apr; 53(1):
101-106.
19. Polit D E, Beck C T. Nursing Research. Principles and Methods, 7th Edition, Philadelphia. J
B Lipppincott Company 2008; pp 215-227.
29 20. Samuel C. Hughes, Gershon Levinson, Mark A. Rosen, Sol M. Shnider, Shnider and
Levinson's anesthesia for obstetrics, IVth edition, Lippincott publications, pp 297.
21. H. Seneviratne, Pregnancy Induced Hypertension, Ist edition, Orient longman publications, pp 85.
22. Sehgal A, Telang S, Passah SM, Jyothi MC. Maternal and neonatal profit and immediate outcome in extremely low weight babies in Delhi. 2003;Oct 40(10) 991-995.
23. Bedi N, Dhillon BS, Maternal deaths in India preventable tragedies. J Obstet Gynaecol
India. 2005: Oct 51:86-92.
24. Yücesoy G, Ozkan S, Bodur H, Tan T, Calişkan E, Vural B, Corakçi A. Maternal and
perinatal outcome in pregnancies complicated with hypertensive disorder of pregnancy, Arch
Gynecol Obstet. 2005 Nov; 273(1):43-9.
25. Redman CW, Sargent IL. Latest advances in understanding preeclampsia.Science. Jun
10 2005;308(5728):1592-4.
26. Huda SS, Freeman DJ, Nelson SM, The Management of hypertensive disorders of pregnancy. Expert Rev Cardiovasc Ther. 2009; Dec; 7(12): 1581-94.
27. Yeo S, Davidge S, Ronis DL, Antonakos CL, Hayashi R, O’ Leary S, A Comparison of walking exercise to reduce the incidence of Preeclampsia. Hyper tens pregnancy. 2008; 27 (2):
113-30.
30 28. Moodley J, Kalane G. A review of the management of eclampsia: practical issues. Hypertens Pregnancy. 2006;25(2):47-62.
29. Roberts JM, Myatt L, Spong CY, Vitamin C and E to prevent complications of pregnancy associated hypertension. N Engl J Med. 2010 Apr 8; 362(14): 1282-91.
30. Yang M, Shen W, Chen L. pregnancy induced hypertension complicated acute disseminated intravascular coagulation with the clinical analysis of 26 cases. Zhonghua FU
Chan Ke Za Zhi. 2003 Oct;34(10):600-602.
31. Edlow AG, Srinivas SK, Elovitz MA. Investigating the risk of hypertension shortly after
pregnancies complicated by preeclampsia. Am J Obstet Gynecol. 2009 May;200(5):e60-2.
Epub 2008 Dec 27.
32. Buchbinder A, Sibai BM, Caritis S, Macpherson C, . Adverse perinatal outcomes are significantly higher in severe gestational hypertension than in mild preeclampsia. Am J Obstet
Gynecol. 2002 Jan;186(1):66-71.
33. Huang Y, Incidence of pregnancy induced hypertension and effects on mother and fetus.
Zhonghua Fu Chan Ke Za Zhi. Journal of Obstetrics and Gynecology. 2001 Mar; 36(3): 137-9.
34. Sibai BM. Hypertension. In: Gabbe SG, Niebyl JR, Simpson JL, eds. Obstetrics - Normal and
Problem Pregnancies. 5th ed. Philadelphia, Pa: Elsevier Churchill Livingstone; 2007: pp 253-
257.
31 35. Cunnigham FG, Leveno KL, Bloom SL, et al . Hypertensive disorders in pregnancy. In:
Cunnigham FG, Leveno KL, Bloom SL, et al, eds. Williams Obstetrics. 22nd ed. New York,
NY; McGraw-Hill; 2005: pp 312-315..
36. Hofrmeyr GJ, Lawrine TA, Atallah AN, Duley L, Calcium supplementation during pregnancy for preventing hypertensive disorders and related problems. Department of
Obstetrics and Gynaecology. Cohrane database syst. Rev 2010 Aug 4; (8).
37. Jaramillo P, Garctia RG, Preventing pregnancy induced hypertension: are there regional differences for this global problem. J hypertens. 2005 Jun; 23 (6): 1121-9.
38. Vainio M, Kujansuu E. low dose acetylsalicylic acid in prevention of pregnancy induced hypertension and intrauterine growth retardation in women with bilateral uterine artery notches.
BJOG. 2002 Feb; 109(2); 161-167.
39. Ashley DE, Fedrick A, Golding J, Mac Gillivray I. Strategies to prevent preeclampsia in a developing country, Int, Gynaecol Obstet. 2004; Dec, 87(3):284-285.
40. Dalmini NJ. A descriptive exploratory study which aimed at identifying the factors that is associated with preeclampsia. Curationics. 1997; Dec 20; 20(4):16-22.
41. Mühlhauser I, Sawicki PT, Didjurgeit U, Jörgens V, Trampisch HJ, Berger M. Evaluation of a structured teaching program on pregnancy induced hypertension treatment and teaching program in general practice. Clin Exp Hypertens. 1993 Jan; 15(1):125-42.
32 33