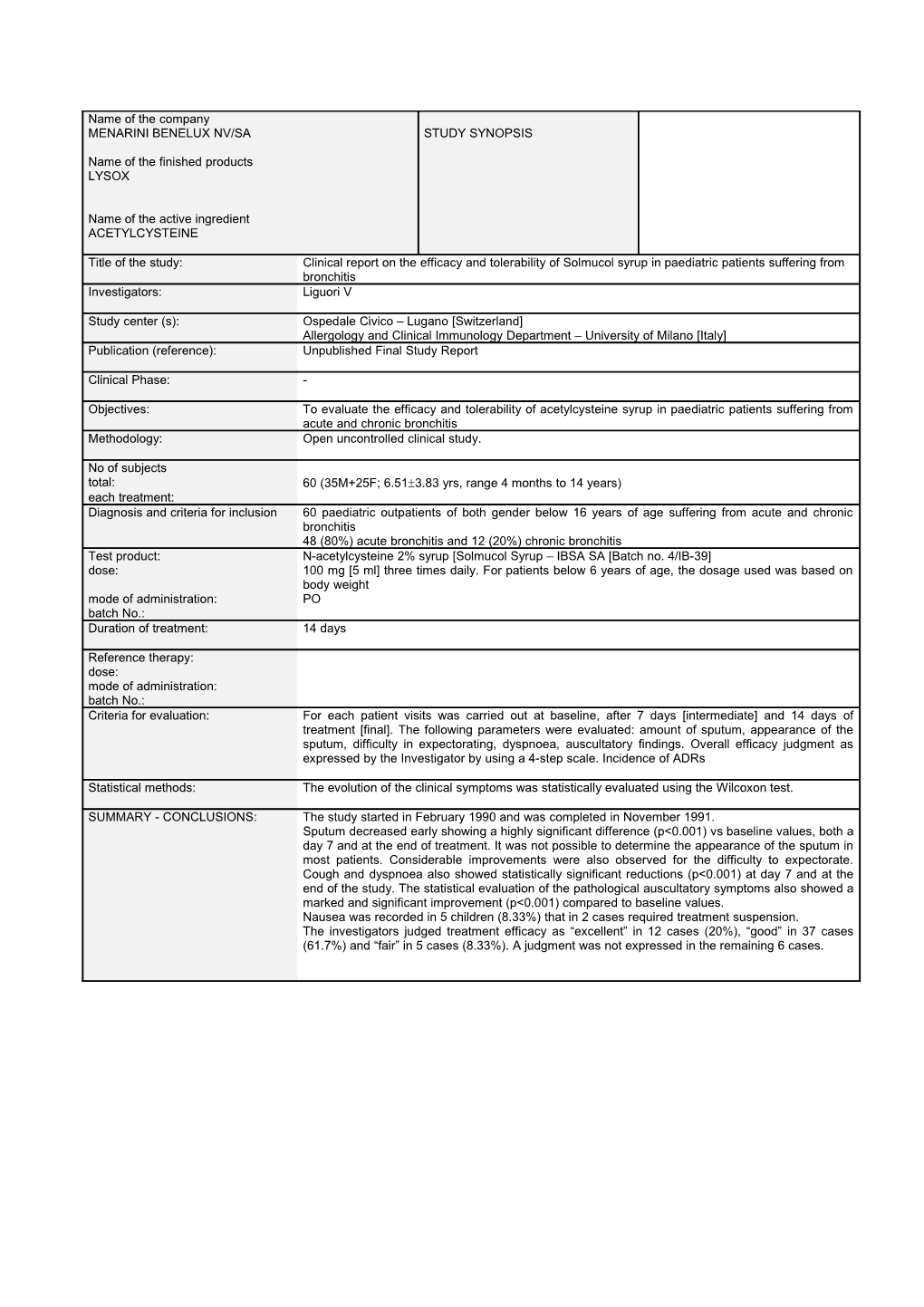
Name of the company MENARINI BENELUX NV/SA STUDY SYNOPSIS
Name of the finished products LYSOX
Name of the active ingredient ACETYLCYSTEINE
Title of the study: Clinical report on the efficacy and tolerability of Solmucol syrup in paediatric patients suffering from bronchitis Investigators: Liguori V
Study center (s): Ospedale Civico – Lugano [Switzerland] Allergology and Clinical Immunology Department – University of Milano [Italy] Publication (reference): Unpublished Final Study Report
Clinical Phase: -
Objectives: To evaluate the efficacy and tolerability of acetylcysteine syrup in paediatric patients suffering from acute and chronic bronchitis Methodology: Open uncontrolled clinical study.
No of subjects total: 60 (35M+25F; 6.513.83 yrs, range 4 months to 14 years) each treatment: Diagnosis and criteria for inclusion 60 paediatric outpatients of both gender below 16 years of age suffering from acute and chronic bronchitis 48 (80%) acute bronchitis and 12 (20%) chronic bronchitis Test product: N-acetylcysteine 2% syrup [Solmucol Syrup – IBSA SA [Batch no. 4/IB-39] dose: 100 mg [5 ml] three times daily. For patients below 6 years of age, the dosage used was based on body weight mode of administration: PO batch No.: Duration of treatment: 14 days
Reference therapy: dose: mode of administration: batch No.: Criteria for evaluation: For each patient visits was carried out at baseline, after 7 days [intermediate] and 14 days of treatment [final]. The following parameters were evaluated: amount of sputum, appearance of the sputum, difficulty in expectorating, dyspnoea, auscultatory findings. Overall efficacy judgment as expressed by the Investigator by using a 4-step scale. Incidence of ADRs
Statistical methods: The evolution of the clinical symptoms was statistically evaluated using the Wilcoxon test.
SUMMARY - CONCLUSIONS: The study started in February 1990 and was completed in November 1991. Sputum decreased early showing a highly significant difference (p<0.001) vs baseline values, both a day 7 and at the end of treatment. It was not possible to determine the appearance of the sputum in most patients. Considerable improvements were also observed for the difficulty to expectorate. Cough and dyspnoea also showed statistically significant reductions (p<0.001) at day 7 and at the end of the study. The statistical evaluation of the pathological auscultatory symptoms also showed a marked and significant improvement (p<0.001) compared to baseline values. Nausea was recorded in 5 children (8.33%) that in 2 cases required treatment suspension. The investigators judged treatment efficacy as “excellent” in 12 cases (20%), “good” in 37 cases (61.7%) and “fair” in 5 cases (8.33%). A judgment was not expressed in the remaining 6 cases.