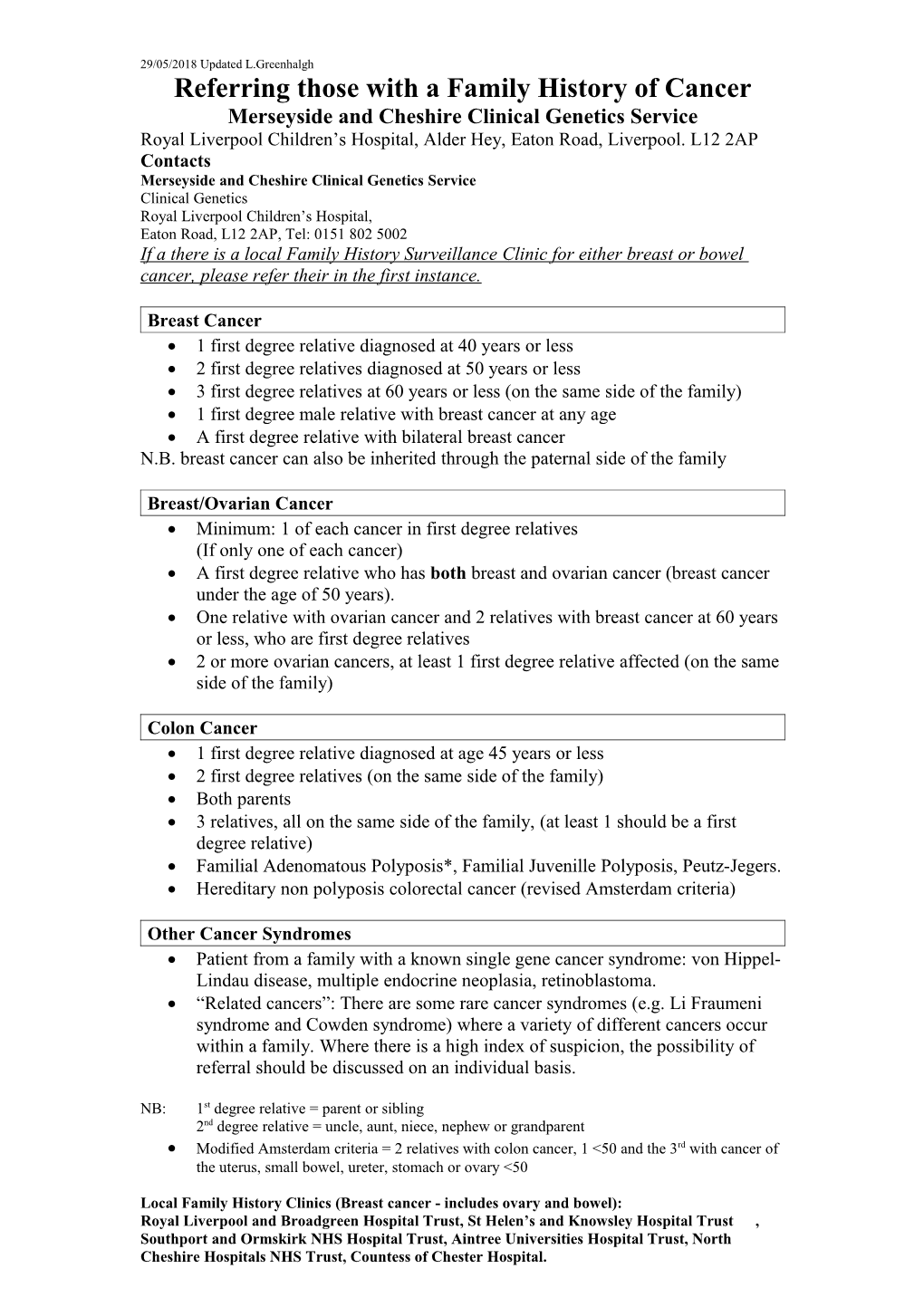
29/05/2018 Updated L.Greenhalgh Referring those with a Family History of Cancer Merseyside and Cheshire Clinical Genetics Service Royal Liverpool Children’s Hospital, Alder Hey, Eaton Road, Liverpool. L12 2AP Contacts Merseyside and Cheshire Clinical Genetics Service Clinical Genetics Royal Liverpool Children’s Hospital, Eaton Road, L12 2AP, Tel: 0151 802 5002 If a there is a local Family History Surveillance Clinic for either breast or bowel cancer, please refer their in the first instance.
Breast Cancer 1 first degree relative diagnosed at 40 years or less 2 first degree relatives diagnosed at 50 years or less 3 first degree relatives at 60 years or less (on the same side of the family) 1 first degree male relative with breast cancer at any age A first degree relative with bilateral breast cancer N.B. breast cancer can also be inherited through the paternal side of the family
Breast/Ovarian Cancer Minimum: 1 of each cancer in first degree relatives (If only one of each cancer) A first degree relative who has both breast and ovarian cancer (breast cancer under the age of 50 years). One relative with ovarian cancer and 2 relatives with breast cancer at 60 years or less, who are first degree relatives 2 or more ovarian cancers, at least 1 first degree relative affected (on the same side of the family)
Colon Cancer 1 first degree relative diagnosed at age 45 years or less 2 first degree relatives (on the same side of the family) Both parents 3 relatives, all on the same side of the family, (at least 1 should be a first degree relative) Familial Adenomatous Polyposis*, Familial Juvenille Polyposis, Peutz-Jegers. Hereditary non polyposis colorectal cancer (revised Amsterdam criteria)
Other Cancer Syndromes Patient from a family with a known single gene cancer syndrome: von Hippel- Lindau disease, multiple endocrine neoplasia, retinoblastoma. “Related cancers”: There are some rare cancer syndromes (e.g. Li Fraumeni syndrome and Cowden syndrome) where a variety of different cancers occur within a family. Where there is a high index of suspicion, the possibility of referral should be discussed on an individual basis.
NB: 1st degree relative = parent or sibling 2nd degree relative = uncle, aunt, niece, nephew or grandparent Modified Amsterdam criteria = 2 relatives with colon cancer, 1 <50 and the 3rd with cancer of the uterus, small bowel, ureter, stomach or ovary <50
Local Family History Clinics (Breast cancer - includes ovary and bowel): Royal Liverpool and Broadgreen Hospital Trust, St Helen’s and Knowsley Hospital Trust , Southport and Ormskirk NHS Hospital Trust, Aintree Universities Hospital Trust, North Cheshire Hospitals NHS Trust, Countess of Chester Hospital. 29/05/2018 Updated L.Greenhalgh
The Cancer Genetics Service
Only 5-10% of cancers of the breast, ovary and colon are due to an inherited predisposition and The Family History Breast Surveillance Clinics supported by the Merseyside and Cheshire Cancer Genetics Service assess the risk of cancer based on the reported family history and work with the relevant specialists to recommend further screening strategies where appropriate. The referral criteria suggest who may be at significantly increased risk of an inherited cancer.
Process: On receipt of appropriate referrals An appointment will be made for a Genetic Counsellor to identify family history and baseline information. Further clarification and confirmation of relevant diagnosis. This may take several weeks. Consultation with Genetic Counsellor or Genetic Consultant GP, Referring doctor and patient all receive information on risk grouping and advised screening where appropriate. We aim not to see low risk referrals as these can be managed in Primary Care
Low risk This group, should be reassured, that on the information given, their risk is not raised to a significant degree above that of the general population. Extra surveillance is not suggested. It should be clearly stated that individuals in this group still have the same risk (or perhaps slightly higher) of cancer as any other individual of the same age in the general population. They should continue the standard health awareness and screening as the general population. This information can be given in a Primary Care setting.
Moderate risk Ongoing management between primary care and appropriate specialist (for example the local Family history Screening Clinic) is recommended. The pathway will indicate the appropriate referral route for the GP and patient to consider.
High risk In addition to suggesting the involvement of other specialist surveillance, this group will be offered a genetic clinic appointment, and if requested, genetic testing can be pursued in some families.
Genetic Clinics offer Time to discuss issues at length Where appropriate: Follow up of other family members at high risk Storage of DNA from affected individuals, and organisation of molecular genetic testing. Discussion of the advantages and disadvantages of gene testing options
All Queries: Merseyside and Cheshire Clinical Genetics Service. Tel: 0151 802 5002.