Patient Sticker
INITIAL ASSESSMENT AND DATA BASE
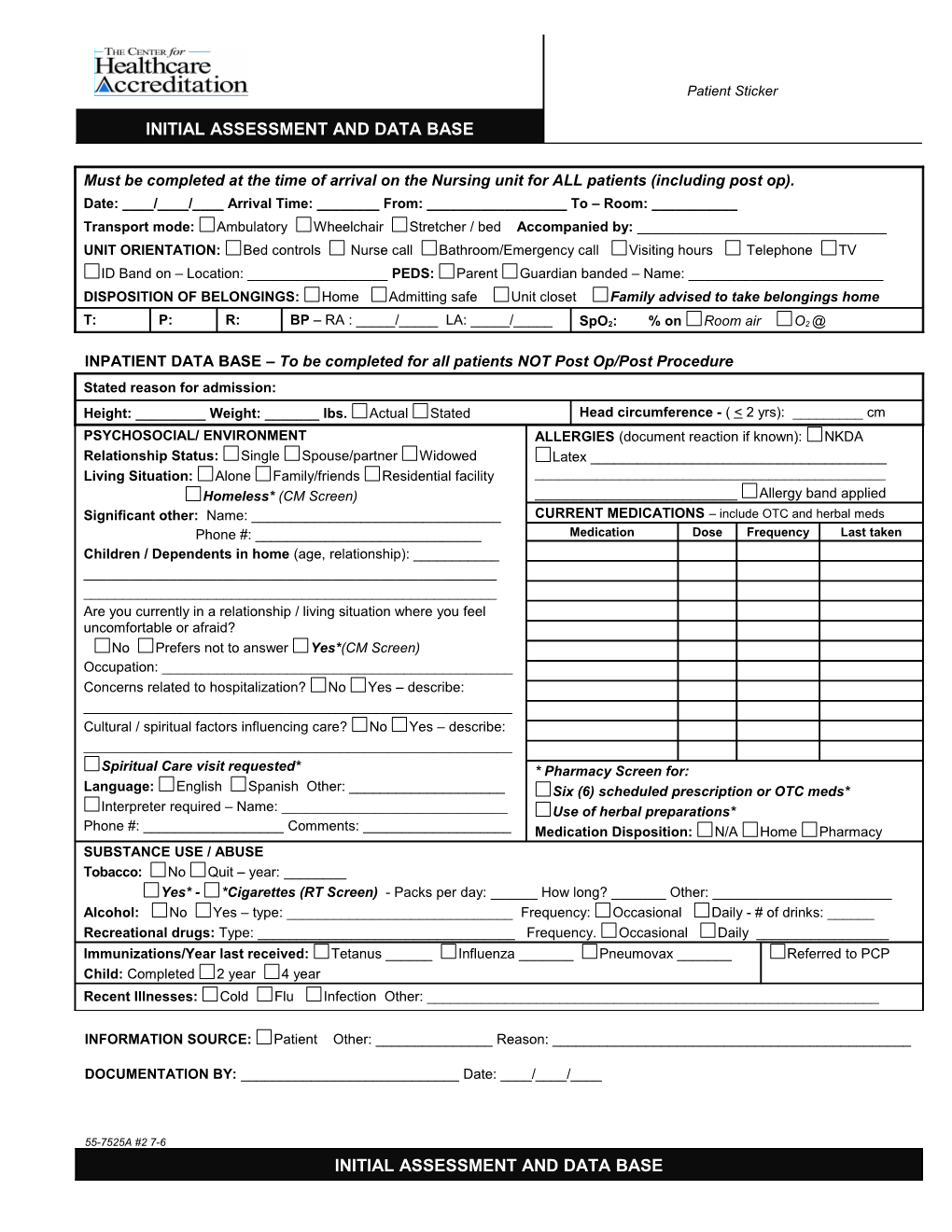
Must be completed at the time of arrival on the Nursing unit for ALL patients (including post op). Date: ____/____/____ Arrival Time: ______From: ______To – Room: ______Transport mode: Ambulatory Wheelchair Stretcher / bed Accompanied by: ______UNIT ORIENTATION: Bed controls Nurse call Bathroom/Emergency call Visiting hours Telephone TV ID Band on – Location: ______PEDS: Parent Guardian banded – Name: ______DISPOSITION OF BELONGINGS: Home Admitting safe Unit closet Family advised to take belongings home
T: P: R: BP – RA : _____/_____ LA: _____/_____ SpO2: % on Room air O2 @
INPATIENT DATA BASE – To be completed for all patients NOT Post Op/Post Procedure Stated reason for admission: Height: ______Weight: ______lbs. Actual Stated Head circumference - ( < 2 yrs): ______cm PSYCHOSOCIAL/ ENVIRONMENT ALLERGIES (document reaction if known): NKDA Relationship Status: Single Spouse/partner Widowed Latex ______Living Situation: Alone Family/friends Residential facility ______Homeless* (CM Screen) ______Allergy band applied Significant other: Name: ______CURRENT MEDICATIONS – include OTC and herbal meds Phone #: ______Medication Dose Frequency Last taken Children / Dependents in home (age, relationship): ______Are you currently in a relationship / living situation where you feel uncomfortable or afraid? No Prefers not to answer Yes*(CM Screen) Occupation: ______Concerns related to hospitalization? No Yes – describe: ______Cultural / spiritual factors influencing care? No Yes – describe: ______Spiritual Care visit requested* * Pharmacy Screen for: Language: English Spanish Other: ______Six (6) scheduled prescription or OTC meds* Interpreter required – Name: ______Use of herbal preparations* Phone #: ______Comments: ______Medication Disposition: N/A Home Pharmacy SUBSTANCE USE / ABUSE Tobacco: No Quit – year: ______Yes* - *Cigarettes (RT Screen) - Packs per day: ______How long? ______Other: ______Alcohol: No Yes – type: ______Frequency: Occasional Daily - # of drinks: ______Recreational drugs: Type: ______Frequency. Occasional Daily ______Immunizations/Year last received: Tetanus ______Influenza ______Pneumovax ______Referred to PCP Child: Completed 2 year 4 year Recent Illnesses: Cold Flu Infection Other: ______
INFORMATION SOURCE: Patient Other: ______Reason: ______
DOCUMENTATION BY: ______Date: ____/____/____
55-7525A #2 7-6 INITIAL ASSESSMENT AND DATA BASE PAST MEDICAL HISTORY Major illness, surgery / procedure Year Major illness, surgery / procedure Year
ASSESSMENT * = Screening recommended – Document on IPOC FALL RISK ASSESSMENT PSYCHOSOCIAL Fearful / anxious Agitated BASIC RISK (Caution) Appropriate to History/findings suggestive of abuse / neglect* situation and normal Age: > 80 for pt. Inadequate home support to meet needs following discharge* Dizziness New devastating, chronic diagnosis* Other: ______Generalized weakness, Comments: ______unsteady gait, use of NEURO LOC: Confused / cognitive limitations - new chronic ambulatory assistive LOC: Alert Responsive to: verbal stimuli simple commands pain device Oriented Speech: clear slurred* rambling* aphasia* Other: ______Altered elimination – Speech: Clear Tactile: Numbness Tingling incontinence, diarrhea, Tactile: No deficit Comments: ______nocturia, frequency. MUSCULOSKELETAL Assistive devices / prosthesis used: ______INCREASED RISK (Alert) States no Balance/Gait impairment* 1 or more falls in past 6 months* (other than slip/trip) Fall within past 6 problems Assistance required or dependent for*: mobility transfers bed mobility PT months eating dressing hygiene toileting OT Confusion/ Disorientation Limitations affecting function* ______RISK LEVEL Comments: ______Determination will be as GI / GU Abdomen: firm distended tender ostomy / tubes*: ______follows: Abdomen: WNL Problems with:( nausea vomiting diarrhea: > 3 days*) chewing CAUTION – Any one States no swallowing* incontinence* constipation Other: ______basic risk criteria problems Comments: ______ ALERT – Two (2) or NUTRITION more basic risk criteria Diet at home: ______Requires dietary teaching* or one (1) increased risk States no TPN/PPN* Poor intake > 3 days* Pregnant/lactating* criteria. problems Recent significant unintentional weight loss/gain (> 10 lbs.)* Comments: ______ENDOCRINE Diabetes – control with: insulin pills diet Thyroid - hypo hyper RESPIRATORY Respirations: irregular dyspneic Other: ______Resp: Regular Breath sounds: rales ronchi wheezes Other: ______ Unlabored Cough Home oxygen therapy* – type/ amount: ______Breath sounds: Comments: ______ Clear bilaterally CARDIOVASCULAR Heart rhythm: irregular pacemaker automatic implanted cardioverter/defibrillator Heart rhythm: Pulses: (0 = absent, 1 = weak, 2 = slightly decreased, 3 = strong, 4 = bounding) Regular Right: Radial: _____ DP: _____ PT: _____ Left: Radial: _____ DP: _____ PT: _____ Capillary refill (sec.): RLE: _____ LLE: ______Comments: ______PAIN Present – Location: ______Level (1-10): _____ Frequency: intermittent constant Denies Description: burning dull sharp cramping pressure Other: ______How long? ______Pain made worse by: ______Managed/made better by: ______Pain related concerns/issues: function/quality of life fear of medication addiction fear of inadequate pain relief Acceptable pain level: ______Comments: ______SKIN Skin integrity – See diagram pressure ulcers* Smooth and intact KEY: use abbreviation to indicate appropriate place on No edema or diagram swelling B = burn E = erythema S = scar/body marks Good turgor BR = bruise I = incision T = tube in place Warm and dry CS = cast / splint L = laceration U = pressure ulcer CT = contracture N = necrosis W = wound D = dressing P = petechiae X = amputation Ed = edema R = rash O = other Edema Scale: 1+ = 0 – ½” 2+ = ¼” - ½” 3+ = ½” – 1” 4+ = > 1” BRADEN SKIN ASSESSMENT – Circle appropriate score in each category. If TOTAL score < 16, document interventions on IPOC* TOTAL Score: Sensory Moisture Activity Mobility Nutrition Friction & Shear perception 1 = Constantly 1 = Bedfast 1 = Completely 1 = Very poor 1 = Problem 1 = Completely moist 2 = Chairfast immobile 2 = Probably 2 = Potential problem limited 2 = Very moist 3 = Walks 2 = Very limited inadequate 3 = No apparent 2 = Very Limited 3 = Occasionally occasionally 3 = Slightly limited 3 = Adequate problem 3 = Slightly limited moist 4 = Walks 4 = No limitation 4 = Excellent 4 = No impairment 4 = Rarely moist frequently ASSISTIVE DEVICES Location CAREGIVER ID Signature / Title Date Time Cane Walker ____/____/______/____/____ Wheelchair Documentation by: Glasses Contact lenses Completed / Reviewed by: RN ____/____/____ Hearing aid - Right Left MUST be within 24 hours of admission Dentures / partials - Upper Lower PRE OP DATA BASE /HEALTH HISTORY reviewed ______RN