Two Lungs (right and left) Fleming College Paramedic Program : Working with ACP’s
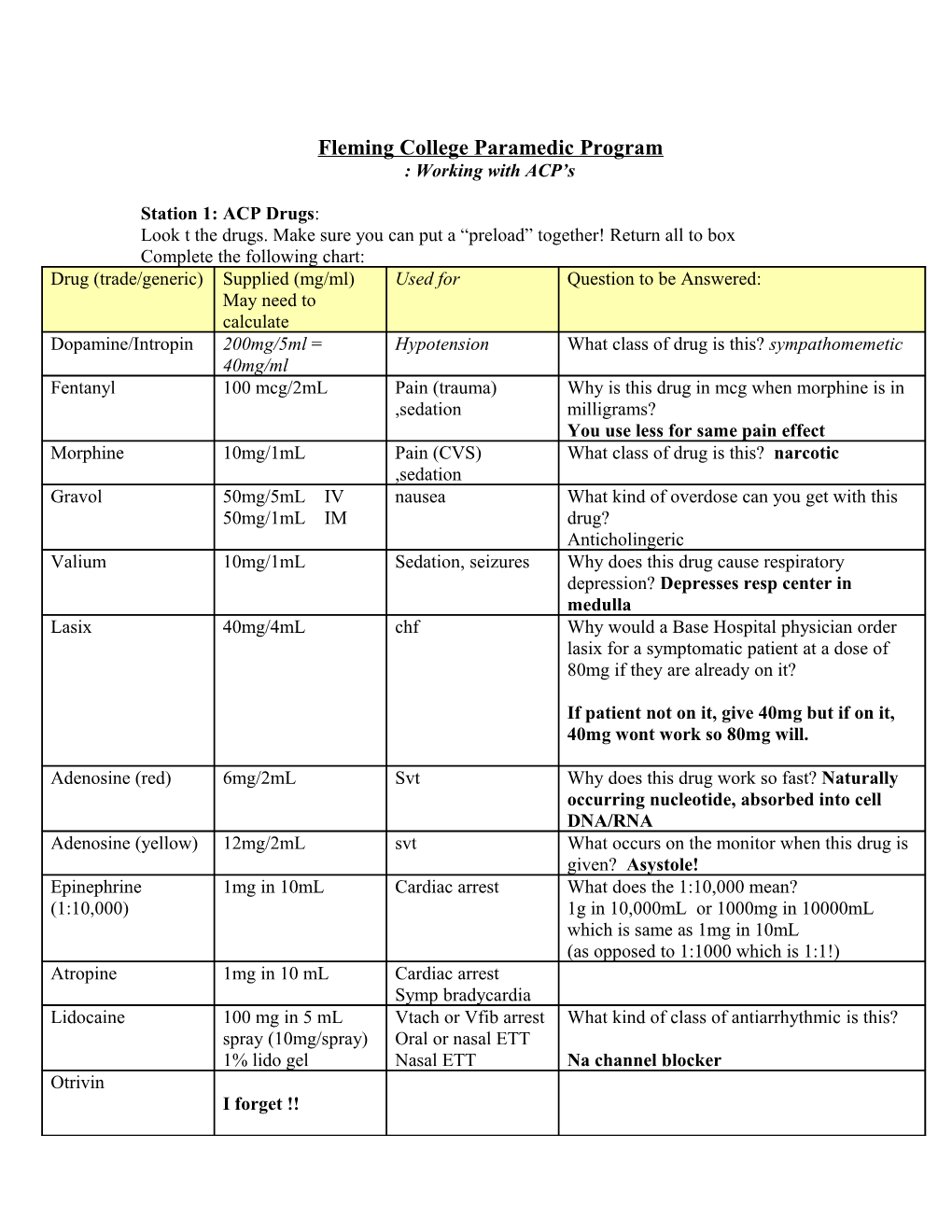
Station 1: ACP Drugs: Look t the drugs. Make sure you can put a “preload” together! Return all to box Complete the following chart: Drug (trade/generic) Supplied (mg/ml) Used for Question to be Answered: May need to calculate Dopamine/Intropin 200mg/5ml = Hypotension What class of drug is this? sympathomemetic 40mg/ml Fentanyl 100 mcg/2mL Pain (trauma) Why is this drug in mcg when morphine is in ,sedation milligrams? You use less for same pain effect Morphine 10mg/1mL Pain (CVS) What class of drug is this? narcotic ,sedation Gravol 50mg/5mL IV nausea What kind of overdose can you get with this 50mg/1mL IM drug? Anticholingeric Valium 10mg/1mL Sedation, seizures Why does this drug cause respiratory depression? Depresses resp center in medulla Lasix 40mg/4mL chf Why would a Base Hospital physician order lasix for a symptomatic patient at a dose of 80mg if they are already on it?
If patient not on it, give 40mg but if on it, 40mg wont work so 80mg will.
Adenosine (red) 6mg/2mL Svt Why does this drug work so fast? Naturally occurring nucleotide, absorbed into cell DNA/RNA Adenosine (yellow) 12mg/2mL svt What occurs on the monitor when this drug is given? Asystole! Epinephrine 1mg in 10mL Cardiac arrest What does the 1:10,000 mean? (1:10,000) 1g in 10,000mL or 1000mg in 10000mL which is same as 1mg in 10mL (as opposed to 1:1000 which is 1:1!) Atropine 1mg in 10 mL Cardiac arrest Symp bradycardia Lidocaine 100 mg in 5 mL Vtach or Vfib arrest What kind of class of antiarrhythmic is this? spray (10mg/spray) Oral or nasal ETT 1% lido gel Nasal ETT Na channel blocker Otrivin I forget !! Lidocaine spray See above What would this potentially be used for? Nasal ettt Versed 5mg/1mL Why would ACP’s carried two drugs of this class? (what is the other one?) Lorazepam (Ativan-)for peds seizures Benzodiazepene
Station 2: ACP Monitor Skills
Activity 1: On the rhythm generator or the mannequin put an SVT/VTACH on the monitor.
What are the signs or symptoms that would make such a patient “unstable”? Chest pain SOB - Pulmonary edema hypotension dizziness Decreased LOC
Attach the LP 12 to the rhythm generator or mannequin: Ensure you are in manual mode (PS. How do you normally do that?______put in manual mode______)
Push the ‘sync’ button: What happens?______marks the R wave_
Why does the machine do that?______to mark the refractory period so don’t shock
Select 100 J for an energy selection: Why not 200 or 300J? ____patient alert, need less J
Charge the machine: Watch carefully after you depress the “shock” button to see if there is a lag or short delay before the machine delivers the energy: Ensuring safety: Shock the patient: This is called__Cardioversion__:
Did you notice a lag?__yes___ Why is this there?_____machine waits for refract to go!_
What could potentially happen if the machine did not mark the ‘R’ waves? Defibrillate! Give someone else in your group a chance to try this out!
Activity 2: Pacing
Q:Put the patient in a second degree or third degree block? What is considered ‘bad’ about these rhythms?______very unstable and usually slow______
Q:What would the LP 12 be designed to do in an ACP setting?__Pace only with ACP___ The pacer function has the following keys: PACER ‘on’ Rate – function key to set the rate – usually set at/above (select the correct) the patient’s normal rate. E.g. if the patient rate was 40, the pacer should be set to _60__or above MAmps – the energy setting used to introduce energy into the chest in order to capture the heart dial this up slowly until you see capture (pacer spike followed by QRS)
Q:Would this cause the patient any discomfort? What would medics do about the pain? Go over some potential paced rhythms and look at their features:
Activity 3: Intubation
In this activity you will become familiar with the steps and challenges involved in the process of intubation. This is an ACP skill currently but you should be familiar with the steps in order to facilitate things for your partner and your patient!
S - stethoscope, stylette L- laryngoscope O - oxygen P - pillow E – ETT x 2 (next size down) S - suction M- magills (forceps)
Steps in Intubation
Preoxygenate with 100% Prepare equipment (SLOPES-M) Hyperextend –Sniffing position Insert laryngoscope into R sweep tongue to left Look for view Insert ETT to 1-3 cm beyond cords Withdraw largyngoscope Remove stylet inflate cuff with 5-8 cc air Auscultate neck, chest x 4 Secure ETT Document cm marking and re-evaluate often
This is what you are looking for!
Trick is not to lever on the teeth
Watch for how much pressure you are exerting. Your aim is to bring the laryngoscope upwards and away (to where the ceiling and the wall meet!) Not as easy as it looks?
Helping in Intubation
Cricoid pressure: Landmark on each other to identify the cricoid ring: Then on the mannequin BURP – Backwards, Upwards and to the Right Pressure – press the thyroid cartilage posterior, and slightly upwards and to the patients R. Try it an see if your visualization is better
Activity 4: Needle Decompression of a Tension Pneumothorax:
In this activity, you will perform the procedure needed to alleviate a tension pneumothorax in a critical situation.
Fill out the chart below: re: Signs and Symptoms Simple Pneumothorax Tension Pneumothorax Mild to mod SOB SEVERE SOB Decreased B/S ABSENT B/S BP High or normal Hypotension or CV collapse SPO2 lower than expected VERY LOW (70’s 80s) SpO2 Mild anxiety Panicky patient N jugular veins Elevated Jug Veins
Equipment needed for Needle decompression : Label its name( look in text)
or
alcohol swabs 3way stopcock Asherman Seal Heimlich Valve
What size(ga) and length (“) would be best? _16ga 2”_
Why?__go through chest wall
Rubber hose ____tape ___16 ga needle or Thora centesis kit _
(Some providers also advocate a 10cc syringe with sterile saline) Find the 2nd intercostals space, mid-clavicular line on a partner. Then find the spot that is above the third rib. (this is THE SPOT- as it avoids the vessels and nerves that run under the 2nd rib) Procedure Now landmark it on the mannequin. Swab the site – in a circular fashion Insert the needle at 90degrees, once into the pleural space, you will hear hissing Remove needle A. If using an A -seal, put this over the catheter. The valve will flutter periodically B. If using a H- valve , attach the 3 way stop cock, then the H valve Secure the device Reassess the patient to ensure that there is resolution of the condition