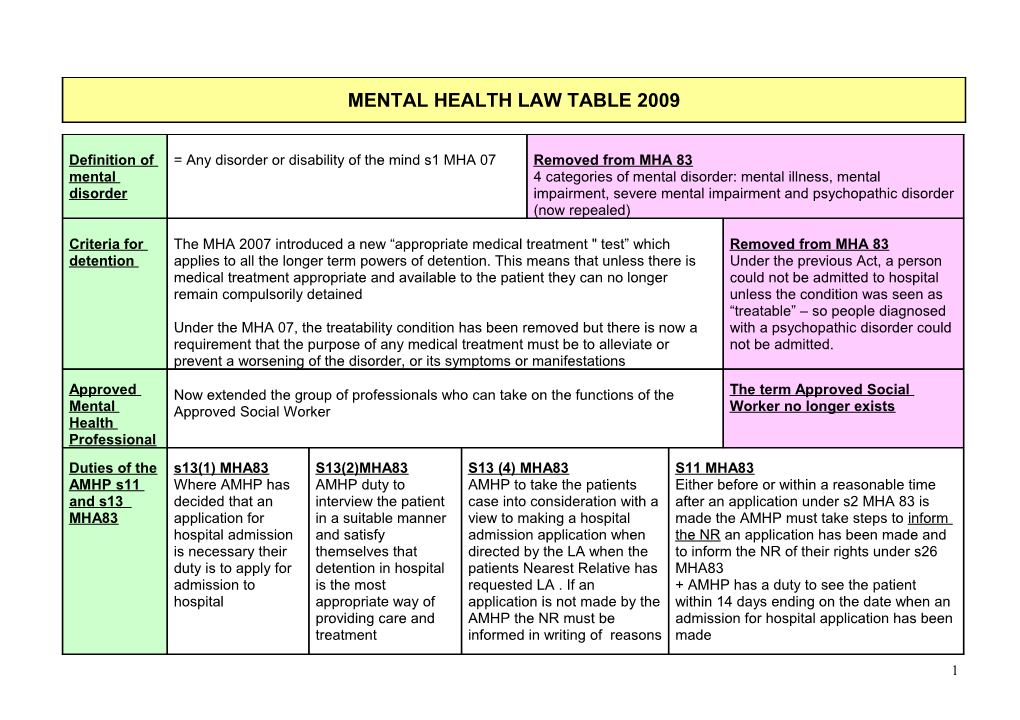
MENTAL HEALTH LAW TABLE 2009
Definition of = Any disorder or disability of the mind s1 MHA 07 Removed from MHA 83 mental 4 categories of mental disorder: mental illness, mental disorder impairment, severe mental impairment and psychopathic disorder (now repealed)
Criteria for The MHA 2007 introduced a new “appropriate medical treatment " test” which Removed from MHA 83 detention applies to all the longer term powers of detention. This means that unless there is Under the previous Act, a person medical treatment appropriate and available to the patient they can no longer could not be admitted to hospital remain compulsorily detained unless the condition was seen as “treatable” – so people diagnosed Under the MHA 07, the treatability condition has been removed but there is now a with a psychopathic disorder could requirement that the purpose of any medical treatment must be to alleviate or not be admitted. prevent a worsening of the disorder, or its symptoms or manifestations
Approved Now extended the group of professionals who can take on the functions of the The term Approved Social Mental Approved Social Worker Worker no longer exists Health Professional Duties of the s13(1) MHA83 S13(2)MHA83 S13 (4) MHA83 S11 MHA83 AMHP s11 Where AMHP has AMHP duty to AMHP to take the patients Either before or within a reasonable time and s13 decided that an interview the patient case into consideration with a after an application under s2 MHA 83 is MHA83 application for in a suitable manner view to making a hospital made the AMHP must take steps to inform hospital admission and satisfy admission application when the NR an application has been made and is necessary their themselves that directed by the LA when the to inform the NR of their rights under s26 duty is to apply for detention in hospital patients Nearest Relative has MHA83 admission to is the most requested LA . If an + AMHP has a duty to see the patient hospital appropriate way of application is not made by the within 14 days ending on the date when an providing care and AMHP the NR must be admission for hospital application has been treatment informed in writing of reasons made
1 Rights of NR under s26 MHA83 Nearest MHA 07 gives the S26 MHA 83 Relative patient the right to Defines who is *To request an assessment with a view to their NR being admitted to hospital apply to displace seen as the their NR . The Nearest Relative *The right to apply for compulsory admission under s2, 3or4 or guardianship s7 county courts can in a hierarchical do this on the list *The right to information (AMHP under s11 must advise if an application under s2 has grounds of Husband /wife or will be made *Right of NR to discharge a person from s2 and to be given a copy of information unsuitability. Civil Partner who has relating to the patient partners are also lived with patient now included as for more than 6 *Right to object to s3 admission NR months *NR Right to order the discharge of a patient under section in writing Eldest child but must be over *Right to be told when a patient is to be discharged 18yrs. *Right to delegate powers so the NR can authorise another person to perform the functions of the NR
Informal S2 MHA83 Admission for S3 MHA83 Treatment Order S4 Application admission Assessment up to 28 days Lasts up to 6 months. for Admission *Patient must be suffering from a -Patient must be suffering from a mental in Emergency Options for s131 MHA 83. No mental disorder of degree that disorder of degree that warrants detention Admission rights to appeal to warrants detention in hospital and this in hospital and this is either in relation to Lasts up to 72 Mental Health is either in relation to their own health their own health and safety or that of hrs Review Tribunal and safety or that of others others + Appropriate treatment must also -Made by AMHP be available *Application has to be made by AMHP or NR and 1 -Application has to be made by AMHP or doctor or NR and founded on 2 medical NR. If NR objects s3 order cannot opinions (one of which must be a proceed -cannot appeal doctor registered under s12 MHA83) + 2 medical opinions (one of which must to Mental health NR can apply to discharge. be a doctor registered under s12 MHA83) Review Tribunal *Can appeal to MHRT s65-66 MHA83 -Can appeal to MHRT s65-66 MHA83
2 Other orders S5 MHA83 Holding Section S135 MHA83 Warrant to Search S136 MHA 83 Power of under Mental -if a patient already in hospital tries to If the AMHP has concerns that a person with a Police to remove a Health Act leave and needs to remain for either mental disorder is being ill treated, neglected, Mentally disordered 1983 his own or others health and safety unable to care for themselves living alone the person from a public either a registered nurse can detain AMHP can apply to a magistrate for a warrant to place to a place of safety the patient for 6 hours or registered enter which the police execute and enter and can medical practitioner can detail for 72 remove the patient to a place of safety for max of 72 Max 72 hours hours hours
Mental A new power is introduced to reduce the If on s2 or s3 or guardianship or You cannot appeal against s4, s5 ,s135 Health time before a case is referred to the Supervised Community Treatment or s136 or if entering hospital voluntarily Review MHRT by hospital managers you can appeal to MHRT under s131 Tribunal s65- 66 MHA83
Options for 1. Supervised Community Treatment section 117A-G MHA 83 (as Will affect a small minority of patients Discharge amended by MHA07) This replaces the supervised discharge under who after a period of detention may be the 1995 Mental Health (Patients in the Community)Act 1995 subject to certain conditions whilst living in the community as well as recall to 2. s117 MHA83 Imposes a joint duty on Health and Social Services to hospital if not complying with medication provide after care for people previously under s3 (6 month order) necessary to ensure they continue with Services must be free medical treatment
OTHER PROVISIONS OF THE MENTAL HEALTH ACT 2007
Age Appropriate Services Advocacy ECT Any person under 18 admitted to The Act places a duty for New safeguards –except in an emergency a patient cannot be hospital must be accommodated arrangements to provide given ECT if they have the capacity to refuse it. Where someone in an environment suitable for Independent Mental Health does not have capacity ECT can only be given where it does not their needs Advocates IMHA’s conflict with an advance directive, or decision of a second opinion doctor or the decision of the Court of Protection
3 Mental Health Act Amended Code of Practice 2008
1.Purpose principle
1.2 Decisions under the Act must be taken with a view to minimising the undesirable effects of mental disorder, by maximising the safety and wellbeing (mental and physical) of patients, promoting their recovery and protecting other people from harm.
2. Least restriction principle
1.3 People taking action without a patient’s consent must attempt to keep to a minimum the restrictions they impose on the patient’s liberty, having regard to the purpose for which the restrictions are imposed.
3.Respect principle
1.4 People taking decisions under the Act must recognise and respect the diverse needs, values and circumstances of each patient, including their race, religion, culture, gender, age, sexual orientation and any disability. They must consider the patient’s views, wishes and feelings (whether expressed at the time or in advance), so far as they are reasonably ascertainable, and follow those wishes wherever practicable and consistent with the purpose of the decision. There must be no unlawful discrimination.
4. Participation principle
1.5 Patients must be given the opportunity to be involved, as far as is practicable in the circumstances, in planning, 5 Mental Health Act Code of Practice developing and reviewing their own treatment and care to help ensure that it is delivered in a way that is as appropriate and effective for them as possible. The involvement of carers, family members and other people who have an interest in the patient’s welfare should be encouraged (unless there are particular reasons to the contrary) and their views taken seriously.
4. Effectiveness, efficiency and equity principle
1.6 People taking decisions under the Act must seek to use the resources available to them and to patients in the most effective, efficient and equitable way, to meet the needs of patients and achieve the purpose for which the decision was taken.
4