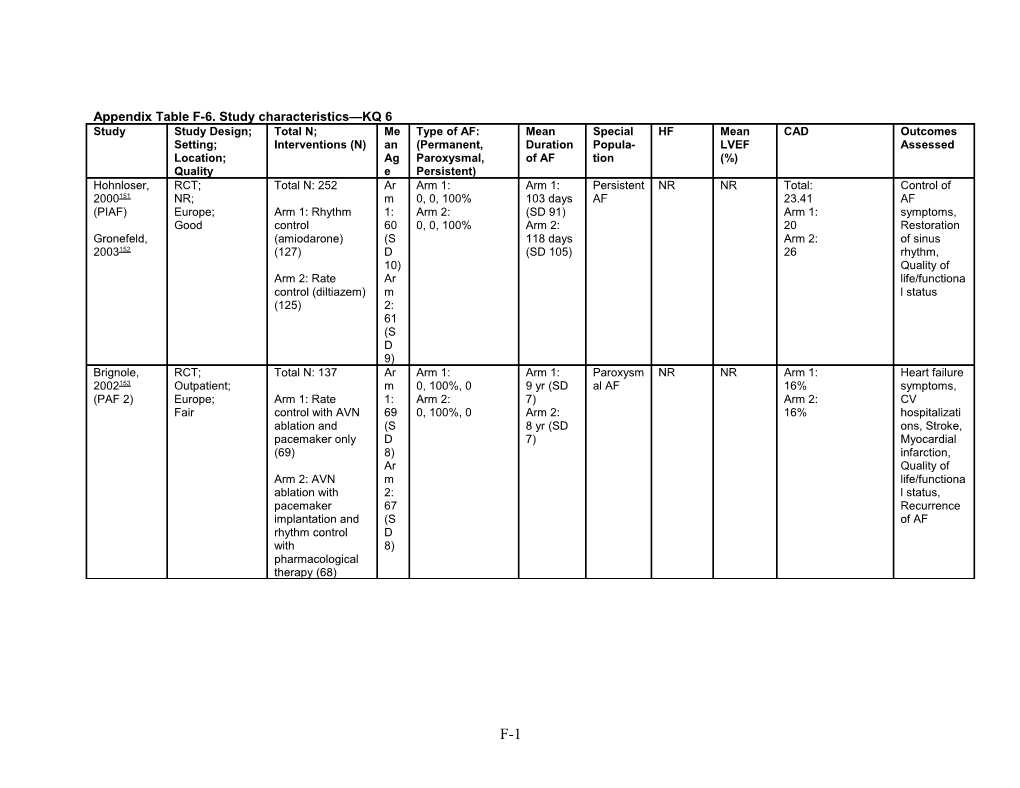
Appendix Table F-6. Study characteristics—KQ 6 Study Study Design; Total N; Me Type of AF: Mean Special HF Mean CAD Outcomes Setting; Interventions (N) an (Permanent, Duration Popula- LVEF Assessed Location; Ag Paroxysmal, of AF tion (%) Quality e Persistent) Hohnloser, RCT; Total N: 252 Ar Arm 1: Arm 1: Persistent NR NR Total: Control of 2000151 NR; m 0, 0, 100% 103 days AF 23.41 AF (PIAF) Europe; Arm 1: Rhythm 1: Arm 2: (SD 91) Arm 1: symptoms, Good control 60 0, 0, 100% Arm 2: 20 Restoration Gronefeld, (amiodarone) (S 118 days Arm 2: of sinus 2003152 (127) D (SD 105) 26 rhythm, 10) Quality of Arm 2: Rate Ar life/functiona control (diltiazem) m l status (125) 2: 61 (S D 9) Brignole, RCT; Total N: 137 Ar Arm 1: Arm 1: Paroxysm NR NR Arm 1: Heart failure 2002153 Outpatient; m 0, 100%, 0 9 yr (SD al AF 16% symptoms, (PAF 2) Europe; Arm 1: Rate 1: Arm 2: 7) Arm 2: CV Fair control with AVN 69 0, 100%, 0 Arm 2: 16% hospitalizati ablation and (S 8 yr (SD ons, Stroke, pacemaker only D 7) Myocardial (69) 8) infarction, Ar Quality of Arm 2: AVN m life/functiona ablation with 2: l status, pacemaker 67 Recurrence implantation and (S of AF rhythm control D with 8) pharmacological therapy (68)
F-1 Study Study Design; Total N; Me Type of AF: Mean Special HF Mean CAD Outcomes Setting; Interventions (N) an (Permanent, Duration Popula- LVEF Assessed Location; Ag Paroxysmal, of AF tion (%) Quality e Persistent) Van Gelder, RCT; Total N: 522 Ar Arm 1: Arm 1: Persistent Arm 1: NR Arm 1: Composite 2002154 Outpatient; m 0, 0, 100% Median AF 51% 29% outcome (RACE) Europe; Arm 1: Rate 1: Arm 2: 337 days Arm 2: Arm 2: (Cardiac Good control (256) 68 0, 0, 100% Arm 2: 49% 26% mortality, Hagens, (S Median Mixed 2004155 Arm 2: Rhythm D 309 days embolic control (266) 9) events Hagens, Ar including 2006156 m stroke, 2: Bleeding Hagens, 68 events 2005157 (S including D hemorrhagic Rienstra, 8) stroke), 2007158 Cardiac mortality, Rienstra, Mixed 2005159 embolic events including stroke, Bleeding events, Maintenance of sinus rhythm, Control of ventricular rate, Quality of life/functiona l status
F-2 Study Study Design; Total N; Me Type of AF: Mean Special HF Mean CAD Outcomes Setting; Interventions (N) an (Permanent, Duration Popula- LVEF Assessed Location; Ag Paroxysmal, of AF tion (%) Quality e Persistent) Wyse, RCT; Total N: 4060 Tot NR Total: None Total: Total: Total: All-cause 2002160 Outpatient; al: 2808 23.1% 54.7 26.1% mortality, (AFFIRM) US, Canada; Arm 1: Rate 69. days (SD Arm 1: (SD 13.5) Arm 1: Composite Good control (2027) 7 69.2) 23.4% Arm 1: 24.5% outcome Bush, (S Arm 1: Arm 2: 54.9 Arm 2: (All-cause 2006161 Arm 2: Rhythm D 1406 22.8% (SD 13.1) 27.6% mortality, control (2033) 9) days (SD Arm 2: Stroke, Chung, Ar 69.4) 54.6 Bleeding 2005162 m Arm 2: (SD 13.8) events 1: 1402 including Curtis, 69. days (SD hemorrhagic 2005163 8 69) stroke,Other (S adverse Guglin, D drug 2010164 8.9 reaction), ) Stroke, Jenkins, Ar Other 2005165 m embolic 2: events Sherman, 69. excluding 2005166 7 stroke, (S Bleeding Steinberg, D events, 2004167 9) Quality of lifefunctional status
F-3 Study Study Design; Total N; Me Type of AF: Mean Special HF Mean CAD Outcomes Setting; Interventions (N) an (Permanent, Duration Popula- LVEF Assessed Location; Ag Paroxysmal, of AF tion (%) Quality e Persistent) Carlsson, RCT; Total N: 200 Ar NR Arm 1: None Arm 1: NR Arm 1: Composite 2003168 Outpatient; m 6 mo 9N 34N outcome (STAF) Europe; Arm 1: Rhythm 1: (SD 2) Arm 2: Arm 2: (All-cause Good control (100) 65. Arm 2: 16N 53N mortality, Carlsson, 3 6 mo Stroke, 2003169 Arm 2: Rate (S (SD 3) Other control (100) D embolic 9.4 events, ) excluding Ar stroke), All- m cause 2: mortality, 66. Cardiac 2 mortality, (S Stroke, D Bleeding 7.6 events, CV ) hospitalizati ons, Maintenance of sinus rhythm, Quality of life/functiona l status Okcun, RCT; Total N: 154 Ar Arm 1: Arm 1: Persistent NR Arm 1: NR Mixed 2004170 Inpatient; m 0, 0, 100% 11 mo AF 31 (SD 8) embolic Europe; Arm 1: Rhythm 1: Arm 2: (SD 7) Arm 2: events Fair control 61 0, 0, 100% Arm 2: 33 including (amiodarone, (S 13 mo (SD 15) stroke, All- electrical D (SD 6) cause cardioversion) 10) mortality, (70) Ar Stroke m Arm 2: Rate 2: control (digoxin or 58 metoprolol) (84) (S D 12)
F-4 Study Study Design; Total N; Me Type of AF: Mean Special HF Mean CAD Outcomes Setting; Interventions (N) an (Permanent, Duration Popula- LVEF Assessed Location; Ag Paroxysmal, of AF tion (%) Quality e Persistent) Opolski, RCT; Total N: 205 Tot Arm 1: Total: Persistent NR NR Arm 1: Composite 2004171 Outpatient; al: 0, 0, 100% 273.7 AF 37.6% outcome (HOT CAFÉ) Europe; Arm 1: Rate 60. Arm 2: days (SD Arm 2: (All-cause Good control (101) 8 0, 0, 100% 112.4) 50% mortality, Opolski, (S Arm 1: Mixed 2003172 Arm 2: Rhythm D 243.2 embolic control (104) 11. days (SD events Pietrasik, 2) 137.3) including 2007173 Ar Arm 2: stroke, m 220.4 Bleeding Szulc, 1: days (SD events 2006174 61. 148.6) including 4 hemorrhagic (S stroke), All- D cause 17. mortality, 6) Cardiac Ar mortality, m Stroke, 2: Bleeding 60. events, 4 Maintenance (S of sinus D rhythm, 7.9 Control of ) ventricular rate, Quality of life/functiona l status
F-5 Study Study Design; Total N; Me Type of AF: Mean Special HF Mean CAD Outcomes Setting; Interventions (N) an (Permanent, Duration Popula- LVEF Assessed Location; Ag Paroxysmal, of AF tion (%) Quality e Persistent) Vora, RCT; Total N: 144 Tot NR Total: None Arm 1: Arm 1: NR Restoration 2004175 Outpatient; al: 6.1 yr 3N 56 of sinus (CRRAFT) Asia; Arm 1: Placebo 38. (SD 5.4) Arm 2: Arm 2: rhythm, Fair (48) 6 5N 55 Maintenance Vora, (S Arm 3: Arm 3: of sinus 2004176 Arm 2: Rhythm D 2N 56.6 rhythm, control 10. Control of (amiodarone) (48) 3) AF Ar symptoms, Arm 3: Rate m Heart failure control (diltiazem, 1: symptoms, electrical 38 Quality of cardioversion) Ar life/functiona (48) m l status, All- 2: cause 39. mortality, 5 Bleeding Ar events m 3: 38. 4 Petrac, RCT; Total N: 102 Ar Arm 1: NR Persistent Arm 1: NR Arm 1: Cardiac 200525 Outpatient; m 0, 0, 100% AF 23.1% 23.1% mortality, Europe; Arm 1: Rate 1: Arm 2: Arm 2: Arm 2: Stroke, All- Good control with AVN 62 0, 0, 100% 12% 16% cause ablation and VVI- (S mortality, CV R pacemaker (52) D hospitalizati 10) ons, Arm 2: Rate Ar Recurrence control with AVN m of AF, Heart ablation and DDD- 2: failure R pacemaker and 60 symptoms, an antiarrhythmic (S Myocardial drug (50) D infarction, 11) Composite outcome (Cardiac mortality, Stroke)
F-6 Study Study Design; Total N; Me Type of AF: Mean Special HF Mean CAD Outcomes Setting; Interventions (N) an (Permanent, Duration Popula- LVEF Assessed Location; Ag Paroxysmal, of AF tion (%) Quality e Persistent) Khan, RCT; Total N: 81 Ar Arm 1: Arm 1: Heart Total: Arm 1: Arm 1: Composite 2008177 Outpatient; m 0, 49%, 51% 4 yr failure 100% 27 (SD 8) 73% outcome (PABA-CHF) NR; Arm 1: Rhythm 1: Arm 2: (SD 2.4) Arm 1: Arm 2: Arm 2: (Quality of Good control (AF 60 0, 54%, 46% Arm 2: 100% 29 (SD 7) 68% life/functiona ablation by PVI, (S 3.9 yr Arm 2: l status), transcatheter) (41) D (SD 2.8) 100% Quality of 8) life/functiona Arm 2: Rate Ar l status, control (AVN m Maintenance ablation and PPM) 2: of sinus (40) 61 rhythm (S D 8) Yildiz, RCT; Total N: 221 Ar Total: Arm 1: Persistent NR Arm 1: NR Maintenance 2008178 NR; m 0, 0, 100% 11 mo AF 60 of sinus Europe; Arm 1: Rhythm 1: Arm 1: (SD 7) (SD 11) rhythm, Poor control (155) 61 0, 0, 100% Arm 2: Arm 2: Mixed (S Arm 2: 13 mo 63 (SD 9) embolic Arm 2: Rate D 0, 0, 100% (SD 6) events control (66) 9) including Ar stroke, m Stroke, All- 2: cause 57 mortality, (S Quality of D life/functiona 11) l status
F-7 Study Study Design; Total N; Me Type of AF: Mean Special HF Mean CAD Outcomes Setting; Interventions (N) an (Permanent, Duration Popula- LVEF Assessed Location; Ag Paroxysmal, of AF tion (%) Quality e Persistent) Shelton, RCT; Total N: 61 Tot Total: Total: Heart Total: NR Total: Quality of 2009179 Outpatient; al: 0, 0, 100% Median failure, 100% 50% life/ (CAFÉ-II) UK; Arm 1: Rate 72. Arm 1: 14 mo Persistent Arm 1: Arm 1: Functional Good control (digoxin or 4 0, 0, 100% (IQR, 6 to AF 100% 55% status beta blockers) (S Arm 2: 32) Arm 2: Arm 2: (31) D 0, 0, 100% Arm 1: 100% 44% 7.1 Median Arm 2: Rhythm ) 15 mo control Ar (IQR, 8 to (amiodarone, m 34) electrical 1: Arm 2: cardioversion) 72. Median (30) 7 14 mo (S (IQR, 5 to D 31) 8.3 ) Ar m 2: 72 (S D 5.4 ) Talajic, RCT; Total N: 1376 Ar Arm 1: NR Heart Arm 1: Arm 1: Arm 1: Cardiac 2010180 (AF- Outpatient; m 0, 33%, 67% failure 100% 27 (SD 6) 48% mortality, CHF) US, Canada, S. Arm 1: Rhythm 1: Arm 2: Arm 2: Arm 2: Arm 2: All-cause America, Israel; control (electrical 66 0, 30%, 70% 100% 27 (SD 6) 48% mortality, Roy, 2008181 Good cardioversion, (S Heart failure AAD) (682) D symptoms, 11) Stroke, Arm 2: Rate Ar Composite control (beta m outcome blockers, digoxin) 2: (All-cause (694) 67 mortality, (S Heart failure D symptoms, 11) Stroke), AF hospital- izations
F-8 Study Study Design; Total N; Me Type of AF: Mean Special HF Mean CAD Outcomes Setting; Interventions (N) an (Permanent, Duration Popula- LVEF Assessed Location; Ag Paroxysmal, of AF tion (%) Quality e Persistent) MacDonald, RCT; Total N: 41 Ar Total: Arm 1: Heart Arm 1: Arm 1: Arm 1: Maintenance 2011182 Outpatient; m 0, 0, 100% 64 mo failure, 100% 19.6 10N of sinus UK; Arm 1: Rate 1: Arm 1: (SD 47.6) Persistent Arm 2: (SD 5.5) Arm 2: rhythm, Poor control (19) 64. 0, 0, 100% Arm 2: AF 100% Arm 2: 11N Quality of 4 Arm 2: 44 mo 16.1 life/ Arm 2: Rhythm (S 0, 0, 100% (SD 36.5) (SD 7.1) Functional control (AF D status ablation by PVI, 8.3 transcatheter) (22) ) Ar m 2: 62. 3 (S D 6.7 ) Abbreviations: AAD9(s)=antiarrhythmic drug(s); AF=atrial fibrillation; CAD=coronary artery disease; CV=cardiovascular; IQR=interquartile range; KQ=Key Question; LVEF=left ventricular ejection fraction; MI=myocardial infarction; mo=month(s); N=number of patients; NR=not reported; PVI=pulmonary vein isolation; RCT=randomized controlled trial; SD=standard deviation
F-9