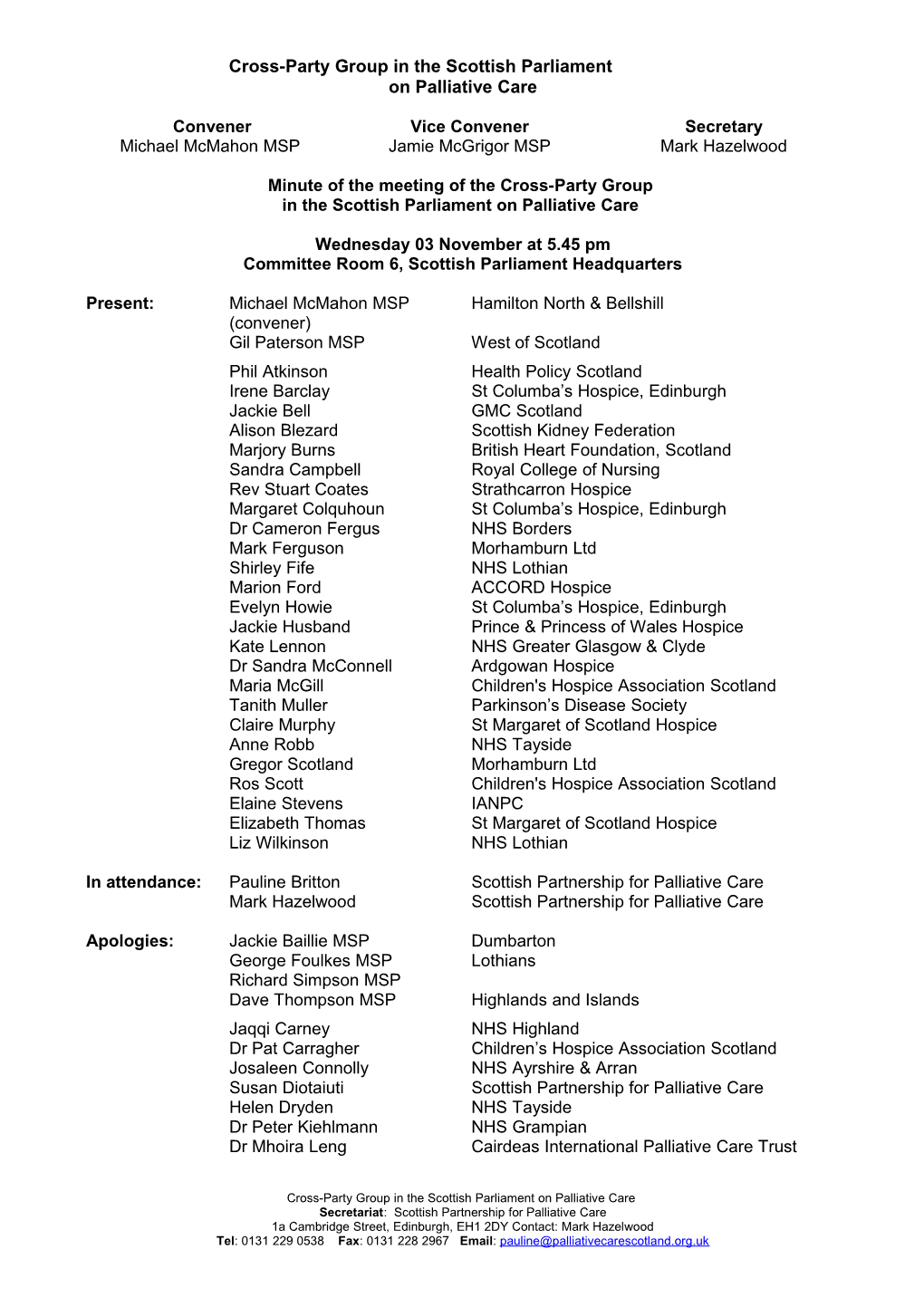
Cross-Party Group in the Scottish Parliament on Palliative Care
Convener Vice Convener Secretary Michael McMahon MSP Jamie McGrigor MSP Mark Hazelwood
Minute of the meeting of the Cross-Party Group in the Scottish Parliament on Palliative Care
Wednesday 03 November at 5.45 pm Committee Room 6, Scottish Parliament Headquarters
Present: Michael McMahon MSP Hamilton North & Bellshill (convener) Gil Paterson MSP West of Scotland Phil Atkinson Health Policy Scotland Irene Barclay St Columba’s Hospice, Edinburgh Jackie Bell GMC Scotland Alison Blezard Scottish Kidney Federation Marjory Burns British Heart Foundation, Scotland Sandra Campbell Royal College of Nursing Rev Stuart Coates Strathcarron Hospice Margaret Colquhoun St Columba’s Hospice, Edinburgh Dr Cameron Fergus NHS Borders Mark Ferguson Morhamburn Ltd Shirley Fife NHS Lothian Marion Ford ACCORD Hospice Evelyn Howie St Columba’s Hospice, Edinburgh Jackie Husband Prince & Princess of Wales Hospice Kate Lennon NHS Greater Glasgow & Clyde Dr Sandra McConnell Ardgowan Hospice Maria McGill Children's Hospice Association Scotland Tanith Muller Parkinson’s Disease Society Claire Murphy St Margaret of Scotland Hospice Anne Robb NHS Tayside Gregor Scotland Morhamburn Ltd Ros Scott Children's Hospice Association Scotland Elaine Stevens IANPC Elizabeth Thomas St Margaret of Scotland Hospice Liz Wilkinson NHS Lothian
In attendance: Pauline Britton Scottish Partnership for Palliative Care Mark Hazelwood Scottish Partnership for Palliative Care
Apologies: Jackie Baillie MSP Dumbarton George Foulkes MSP Lothians Richard Simpson MSP Dave Thompson MSP Highlands and Islands Jaqqi Carney NHS Highland Dr Pat Carragher Children’s Hospice Association Scotland Josaleen Connolly NHS Ayrshire & Arran Susan Diotaiuti Scottish Partnership for Palliative Care Helen Dryden NHS Tayside Dr Peter Kiehlmann NHS Grampian Dr Mhoira Leng Cairdeas International Palliative Care Trust
Cross-Party Group in the Scottish Parliament on Palliative Care Secretariat: Scottish Partnership for Palliative Care 1a Cambridge Street, Edinburgh, EH1 2DY Contact: Mark Hazelwood Tel: 0131 229 0538 Fax: 0131 228 2967 Email: [email protected] Apologies: Prof Dr Calum MacKellar Scottish Council on Human Bioethics (continued) Elaine MacLean Care Commission Kristine McAdam NHS Tayside Paula McCormack Highland Hospice Dorothy McElroy Ardgowan Hospice Irene McKie Strathcarron Hospice Susan Morrison NHS Highland Prof Scott Murray University of Edinburgh Helen Newport NHS Dumfries & Galloway Dr Euan Paterson RCGP Craig Stockton MND Scotland Dr Chris Sugden St Andrew’s Hospice Maggie White Marie Curie Cancer Care
Action 1. Welcome, introductions & apologies: The Convener, Michael McMahon MSP welcomed everyone to the meeting especially guest speaker Gil Paterson MSP. Members were reminded that Gil was originally invited in June to attend the previous meeting of the Group which was scheduled for 8 September 2010. Gil made us aware at the time of our initial invitation that 8 September was a busy evening for him but indicated that he would try to accommodate us in some way on that date. Gil was true to this commitment and was available on 8 September. However, the Convenor and Secretary of the Group decided to cancel that meeting and reschedule, given the importance of, and interest in the Bill, and the fact that despite his best efforts Gil could only attend for a relatively short period. Apologies noted on previous page and above.
2. Minute of previous meeting of Wednesday 16 June 2010 The minute of the meeting of Wednesday 16 June 2010 was proposed by Maria McGill. However the minute was not seconded and did not gain approval because the majority of members who were present at the meeting of 16 June 2010 had submitted apologies for the meeting of 03 November 2010. It was agreed that the Partnership would contact those members who attended the PB meeting of 16 June 2010 to confirm their approval of the minute.
UPDATE: Dr. Belinda Hacking, Consultant Clinical Psychologist and Head of Service at the Edinburgh Cancer Centre seconded the approval of the minute of the meeting of Wednesday 16 June 2010 by email. The minute was then adopted as a true record of the meeting.
3. Matters arising from the previous meeting of Wednesday 16 June 2010: 3.1 International perspectives on palliative care from economically developing countries (item 5.1) The Convener updated the group that so far his efforts to meet with interested MSPs had been unsuccessful, although some 1:1 discussions had taken place. This matter was ongoing and he would continue to try to schedule a meeting of interested members at some point next year.
4. Discussion: Palliative Care (Scotland) Bill Please note that this is not a verbatim record but a summary of key points raised. The Convener invited Gil Paterson MSP to speak about the Bill, after which there would be an opportunity for further discussion.
2 CPG meeting – 03 November 2010 Gil gave some background information about his involvement with the Bill in that he had attended a Parliamentary reception in November 2008 organised by St Margaret of Scotland Hospice and hosted by Roseanna Cunningham MSP to launch her draft Palliative Care (Scotland) Bill proposal. A few months later Roseanna had been appointed as Minister for the Environment and since Government Ministers were not permitted to introduce Member’s Bills, and having no baggage nor fixed ideas at that time about palliative care, Gil had agreed to take the proposal forward on her behalf, and had extended the consultation period for his own benefit. The Bill had been prepared by the non-executive Bills unit on behalf of Gil – there were two main parts for consideration, a statutory duty to provide palliative care and a system to monitor and measure the delivery of palliative care. Gil explained that a breakdown of responses to the Bill had shown that on the whole support had come from individuals, whilst institutional type bodies were against it or had requested/suggested some amendments to it. Two main concerns arising from the responses had included the litigation of the health service and the costs of monitoring and measuring palliative care delivery. Resources needed for the reporting system (based on a similar system) was £50,000 however this could cost up to £400,000 – it was a very difficult figure to predict. Not long after the launch of the Bill, Living and Dying Well (L&DW) a national action plan for palliative and end of life care in Scotland was emerging which would deliver everything the Bill was trying to achieve. In fact, the Bill sought to complement the intentions of L&DW and its lack of a reporting system. To gauge public and professional opinions around palliative care, Gil had visited hospitals, hospices and care homes, not quite throughout Scotland but certainly between Inverness and Greenock, and spoke to almost 500 people right across the board and at the coal face: doctors, nurses, managers, clinicians, volunteers, patients and their families and carers. From what he had heard and learned from his visits, including the very positive comments about L&DW and its progress, he believed even more that legislation should be introduced to effect palliative care. Both the Health and Sport Committee and the Finance Committee (financial memorandum) had already held evidence sessions and oral evidence was ongoing with a session that morning and a further session the following week. Gil reported that it was commonly said that 90% of people with cancer benefited from palliative care whilst 90% of people with other illnesses did not benefit from palliative care. Gil believed that the practice of ‘being with’ was lacking in current medical education in Scotland and specific training was required to bring about a change in this ethos. He felt that there was a need for improved education at every level (a module on palliative care was certainly not enough) and an attitudinal shift was necessary. It was a fact that some nursing staff were still frightened of confronting the needs of the dying. Palliative care had been seen as a Cinderella service outwith mainstream medicine for years, and now was the time to move forward and change this situation. The Chairman then opened up the discussion to the floor and the following points were raised:
research at Strathcarron Hospice into the experience of 'being with' as practiced by nurses in a hospice, showed that this excellent practical training was of great significance to palliative care the majority of general practitioners did deliver palliative care as it was seen as a core duty, ‘it’s what they did’ recommendations from L&DW Building on Progress were trying to address the attitudinal shift Gil had mentioned earlier L&DW was encouraging Health Boards and clinicians to take indicators on board,
CPG meeting – 03 November 2010 3 but some of the indicators identified in the Bill did not align with those suggested in the action plan if the Bill fell then some other legislation would be required to complement L&DW because on its own it was not enough best practice in palliative care was carried out in hospices palliative care provision for families and carers could also come from social care providers yet the Bill had put the onus onto Health Boards to drive things forward local authorities had a duty of care to provide services including palliative care but data for best practice in social care was not collected and reported to health boards L&DW was making an impact in some localities but where? Best practice data needed to be recorded and shared with other areas a huge amount of care was being provided by social care but this was not always officially recognised Pockets of delivery of end of life care / social care at home or in care homes could be deemed a second class service – Ministers should have a duty to ensure patients falling into this category were receiving first rate palliative care – this should also be true for patients with any conditions with complex needs. Some medical staff in hospitals found it difficult to care for such patients – it was time to look outside of the typical training model for NHS services and embrace a different type of education. Attitudinal change did take time – L&DW was already two years old and during that time a huge amount of work was already in place and ongoing for example the DNACPR policy, ePCS etc – enormous changes were already taking place but more time was needed. Five years was a more realistic length of time to demonstrate progress. the collection and publication of data on palliative and end of life care should be monitored through L&DW if after five years L&DW did not encompass the recommendations from the Audit Scotland report and produce the required evidence, then surely that was the time to progress the Bill The Bill was not meant as a criticism – it was quite clear the amount of work, energy and dedication which had already been carried out by health care staff. Two years was sufficient time to show a difference but how was this data being reported? The Scottish Government was currently not able to produce such figures. The Bill had encouraged much more discussion about indicators than had previously taken place – Gil was listening to these arguments and was seeking the best way forward to support L&DW. There might be too many suggested indicators or there might not be enough – this was open to further refinement. The bottom line was that a system of measurement needed to be in place to collect data to improve the quality, equity and delivery of palliative care provision. Data was already available from the palliative care register and more recently via the DES for palliative care. More data would be available when these were linked to the ePCS. It was unfortunate that there was not enough solid evidence to demonstrate how far L&DW had progressed but there was lots of evidence of good practice /attitudinal change/ latest tools used etc within the Health Boards’ delivery plans. A large number of nurses currently working in the health service were ‘being still’ with their patients – there were many, many examples of good practice emerging from L&DW. Gil was not disputing that L&DW was working but highlighting that there were no concrete figures to support these examples.
4 CPG meeting – 03 November 2010 A worthwhile exercise would be to study the contents of Health Boards’ delivery plans and consider appropriate indicators to collect this data the employment of more staff would allow health care nurses to have more time to ‘be with’ their patients – across Scotland resource issues did not always enable the provision of a good, equitable palliative care service out of all of the submissions to the Bill not one had stated that the current palliative care service was adequate there were tremendous levels of commitment across Scotland but there was just not enough of them – geographically there were patchy areas with different levels and qualities of services being offered within a few miles of each other – it was not the case of rural vs urban L&DW was making a tremendous contribution to palliative care but just needed something else – a little bit extra – the Bill was about supplementing all of L&DW’s good work Within its Living and Dying Well Delivery Plan, NHS Lothian had carried out a palliative care education scoping exercise. Although the analysis was not yet complete, it demonstrated that appropriate education was being delivered throughout the region – at first glance it showed that almost all palliative care education was relevant to those with non-malignant disease as well as to those with malignant disease. This was a huge shift in focus. Over the last few years there had been a high number of generalist staff who were coming along to study palliative care. Over time things were progressing to a gradual attitudinal shift in education. an example was given about a complaint made on behalf of one individual care home patient who had had a number of referrals to a hospice because the care home could not deliver appropriate palliative care for that patient - a change of culture was needed in this particular case and others similar to it it was suggested that the Care Commission could have dealt with the complaint and it was asked if the Bill could improve the quality and delivery of care the Bill would enable L&DW via a reporting system to collect data and show where such poor levels of palliative care were being practiced – L&DW did not measure and the Bill would strengthen it. Palliative care work and good practices needed to be demonstrated in order for increased resources to be put into palliative care which was currently under-resourced and under-utilised.
Regarding timescales for the Bill, the final oral evidence session would be heard the following Wednesday, 10 November 2010. Parliament had agreed a deadline of Friday 10 December 2010 for the end of Stage 1 consideration of the Bill.
At this point in the proceedings Gil Paterson left the meeting and the Chairman offered a warm vote of thanks to him for his contribution to the debate.
5. Discussion: End of Life Assistance (Scotland) Bill
Director of the Partnership, Mark Hazelwood reported that all of the written and oral evidence had now been collected. The Clerk to the End of Life Assistance (Scotland) Bill Committee had informed the Partnership that the Committee was currently considering its draft report (ie the Committee was continuing to meet on Tuesdays and consider a new iteration of the report each week until the Committee was happy with it). To comply with the Parliament’s deadline, the Committee had until 17/18 November to publish its report.
CPG meeting – 03 November 2010 5 Whilst it was perfectly possible that the Committee would publish in advance of that date, it would not be for at least a couple of weeks yet. Members felt that because of the nature of the subject it was difficult to gauge the position of each Committee member and what recommendations they would make in the forthcoming report. It was also difficult to gauge how each MSP would vote in the Parliamentary debate. Westminster was looking closely at this Bill and awaiting the outcome of the debate. The Convenor commented that the Parliamentary process in Scotland (particularly the resources available to the Committee) was not in any way comparable to the progression in the House of Lords of the Joffe Bill which had been taken forward a couple of years ago. There was some concern that the process here in Scotland had been somewhat rushed. The End of Life Assistance (Scotland) Bill Committee had appointed a legal advisor to assist in its work. A few months ago, the Convener had discussed the Bill and the advisor’s appointment to the Committee with Baroness Illora Finlay, who advised him that Lord Joffe’s Assisted Dying for the Terminally Ill Bill had been scrutinised by a Select Committee (under the chairmanship of Lord Mackay) which had at that time appointed two specialist advisors (one with knowledge of palliative care) to assist in its work. The Convenor reminded members that on this information he had considered following this precedent and had written to the Committee with his concerns, requesting the appointment of a second advisor (with palliative care experience) to the Committee. To date he had not yet received a reply and would pursue this further.
The Stage 1 debate on the End of Life Assistance (Scotland) Bill would take place on or before 24 November 2010 - (End of Stage 1 process). It was not known at that stage when the debate would take place because Parliamentary business timetables were fitted into timeslots and announced only two weeks in advance (on Tuesdays).
6. Any other competent business: There was no other competent business on this occasion. 7. Date of next meeting: The scheduled meeting on Wednesday 8 December 2010 had been cancelled and the next meeting was planned for Wednesday 23 March 2011.
There being no further business the meeting closed at 7.15 pm.
6 CPG meeting – 03 November 2010