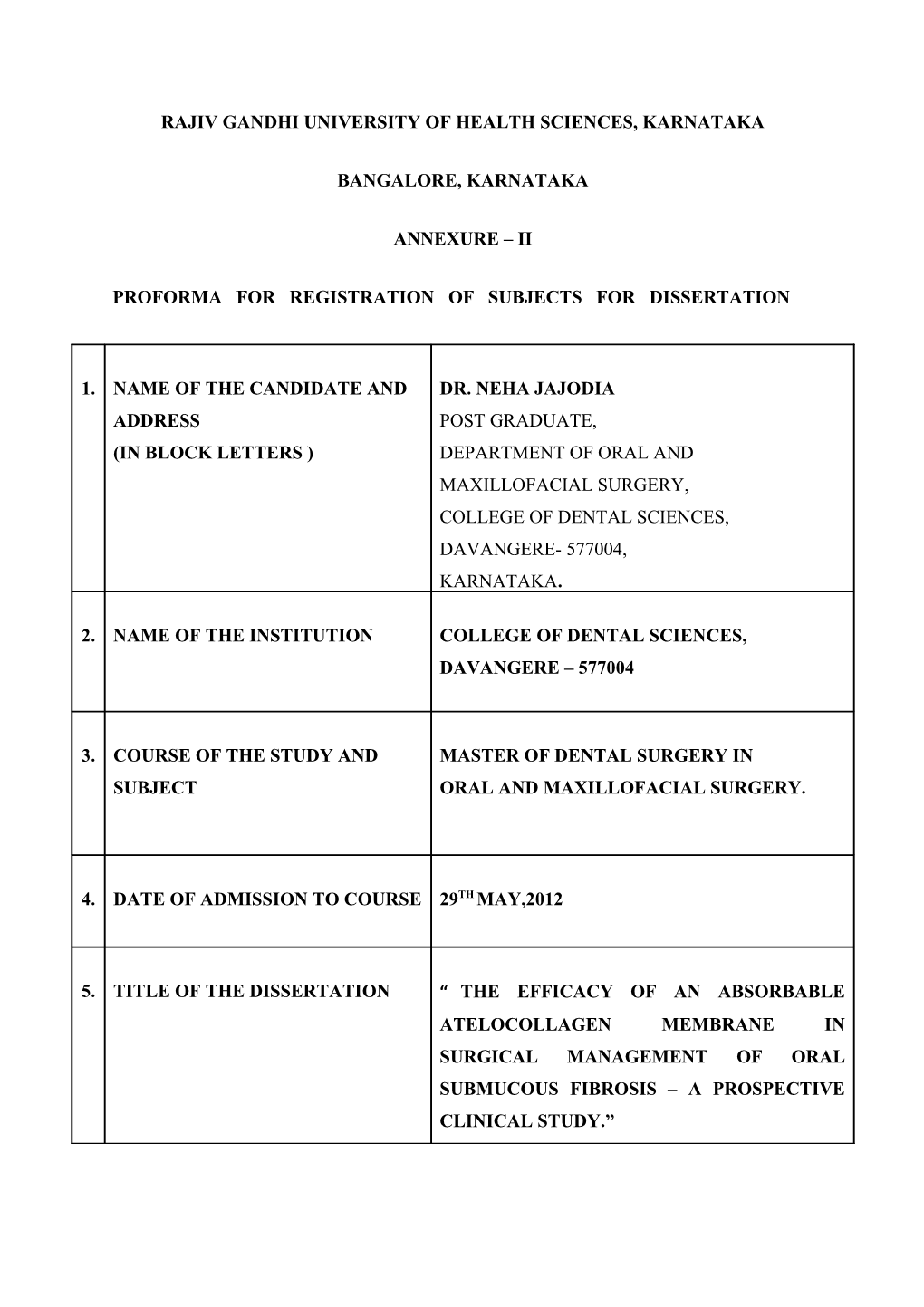
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES, KARNATAKA
BANGALORE, KARNATAKA
ANNEXURE – II
PROFORMA FOR REGISTRATION OF SUBJECTS FOR DISSERTATION
1. NAME OF THE CANDIDATE AND DR. NEHA JAJODIA ADDRESS POST GRADUATE, (IN BLOCK LETTERS ) DEPARTMENT OF ORAL AND MAXILLOFACIAL SURGERY, COLLEGE OF DENTAL SCIENCES, DAVANGERE- 577004, KARNATAKA.
2. NAME OF THE INSTITUTION COLLEGE OF DENTAL SCIENCES, DAVANGERE – 577004
3. COURSE OF THE STUDY AND MASTER OF DENTAL SURGERY IN SUBJECT ORAL AND MAXILLOFACIAL SURGERY.
4. DATE OF ADMISSION TO COURSE 29TH MAY,2012
5. TITLE OF THE DISSERTATION “ THE EFFICACY OF AN ABSORBABLE ATELOCOLLAGEN MEMBRANE IN SURGICAL MANAGEMENT OF ORAL SUBMUCOUS FIBROSIS – A PROSPECTIVE CLINICAL STUDY.” 6. BRIEF RESUME OF INTENDED WORK:
6.1 Need for the study:
Oral Submucous fibrosis (OSMF) is a chronic, debilitating disease characterized by
juxtaepithelial fibrosis of the oral cavity. It is regarded as a precancerous and potentially
premalignant condition. Formerly confined to the Asians particularly in the Indian subcontinent
and Taiwan, it is now often seen in the Asian populations of the United Kingdom, USA, and
other developed countries and is becoming a serious problem for global health. The well-known
causative agent of the disease, areca-nut is now recognized as a group one carcinogen.1 It is
estimated that as many as five million young Indians are suffering from this as a result of the
increased popularity of the habit of chewing betel quid. Various surgical modalities have been
tried in the management of oral submucous fibrosis, each with its own limitations. Local grafts
have been used to cover the buccal mucosal defects after the fibrotic bands are released. The
Nasolabial flap, The Buccal fat pad and Collagen membrane have all been used with satisfactory
postoperative results.
The technique for solubilizing collagen with pepsin while simultaneously removing its
main antigenic structures, the telopeptides was used for the first time in tissue engineering in the
1970s. This solubilized collagen was termed as Atelocollagen. Atelocollagen is obtainable with
a high degree of purity, due to the protease treatment, which when used to extract atelocollagen
breaks down other protein contaminants too. Studies in Japan and Taiwan have used artificial
dermal substitutes made of atelocollagen membrane for reconstructing oral mucosal defects
including Oral submucous fibrosis with promising results.
This study aims to assess the efficacy and usefulness of a commercially available
absorbable Atelocollagen membrane in surgical management of Oral submucous fibrosis. 6.2 Review of Literature:
In a study conducted on 60 patients the efficacy of collagen membrane as a biodegradable wound dressing material for surgical defects of oral mucosa was evaluated. They assessed the usefulness of collagen membrane as an intraoral temporary wound dressing material to promote haemostasis, relieve pain, induce granulation, and assist in rapid epithelialization at the wound site & prevent infection, contracture, scarring, donor -site morbidity, and graft rejection. They concluded that collagen membrane is biologically acceptable to the oral mucosa and is, from the clinical point of view, an excellent wound graft material.2
A prospective study was conducted for the surgical management of oral submucous fibrosis. Buccal pad of fat and collagen membrane were compared and assessed for improving the mouth opening post operatively. The study consisted of 30 patients with bilateral clinically proven cases of oral submucous fibrosis. The results concluded that the collagen membrane group showed better mouth opening post operatively owing to their faster epithelialization rate and less wound contracture.3
This study evaluated the effect of collagen membrane to cover the buccal mucosal defects after the excision of fibrotic bands. Total of 30 cases of advanced oral submucous fibrosis having a mouth opening less than 20mm were surgically treated. The procedure involved bilateral release of fibrous bands, bilateral coronoidectomy, covering the buccal defects with collagen membrane. Regular follow up was done and results were assessed by comparing the pre operative and post operative maximum mouth opening. The collagen membrane used to cover the buccal defects after fibrotic bands release had excellent results. They concluded that the advantages of using collagen membrane to cover the defect of oral mucosa are easily availability, simplicity of procedure, good tolerance of membrane by oral tissue, no need to perform a second operation for obtaining a graft or detachment of the pedicle, no morbidities as associated with various other grafts and no problems associated with donor site healing.4
This study assessed the indications and usefulness of treating tissue defects in the oral region using artificial dermis made of fibrillar atelocollagen membrane in 13 patients with oral mucosal defects. Good tissue repair was achieved in all patients. Healing was observed to be faster than with conventional tissue covering materials. No increase in the IgA and IgG antibodies were noted. They concluded that the membrane was a useful biomaterial for a variety of applications in the oral area.5
A study was conducted in 2009, on 21 patients aiming to investigate the viability of artificial dermis as a substitute for split thickness skin graft in OSMF. Artificial dermis grafts of collagen were used to repair surgical defects after excision of fibrous bands. Patients were followed up for at least 3 months and an overall success rate of 100% was reported. Changes in interincisal distances (IDs) were analyzed in preoperative, intra-operative and postoperative periods and mean final follow up IDs of 15.5, 35, 25 mm were reported respectively. These changes revealed statistically significant differences between values at different stages.6
6.3 Objectives of the study:
The purpose of the study is to assess the effectiveness of an absorbable Atelocollagen
membrane as an alternative material to cover the buccal defects after release of fibrotic
bands in Oral Submucous Fibrosis patients. 7 MATERIALS AND METHODS:
7.1 Source of data :
The patients for this proposed study will be selected from Out-Patient Department of Oral and
Maxillofacial Department of College of Dental Sciences, Davangere. Each patient will be given
a description of the procedure to be performed and will be required to sign an informed consent.
7.2 Method of Collection of Data
Inclusion Criteria :
Male and female subjects within the age group of 15-60yrs
ASA Grade I & II patients
Patients with Grade III and Grade IV Oral Submucous Fibrosis (Khanna and Andrade
grading) requiring surgical management and reconstruction.
Exclusion Criteria :
ASA Grade III & IV patients.
Women who are pregnant.
Patients with known history of hypersensitivity reactions.
Study Design :
This is a prospective clinical based study.
Sample size: 10
7.2 Methods of collection of data:
Procedure would include resection of fibrous bands, intra operative forced mouth opening,
followed by covering the raw mucosal defect with a commercially available absorbable
Atelocollagen membrane which would be stabilized by the use of sutures. In the post operative period the patient will be put on Ryle’s tube feeding. They will be instructed to quit the habit completely. Patients will be required to continue with postoperative physiotherapy along with nutritional supplements.
Evaluation Criteria :-
Changes in the interincisal distances will be analysed preoperative, intra-operatively and
postoperatively.
Post-operative mouth opening will be assessed for every patient at 1 week, 1 month and
3 months time interval using Inter-incisal distances.
Judgement of Atelocollagen membrane will be done based on the scoring pattern that
was used by Rastogi S, Modi M. & Sathian B.2
Following outcome variables will be evaluated -
1. Haemostatic effect
2. Pain relief
3. Granulation
4. Epithelialization
5. Contracture
6. Effectiveness
7. Reactivity
8. Usefulness 7.3 Does the study require any investigations or interventions to be conducted on patients or other humans or animals? If so, please describe briefly.
Yes
Necessary blood investigations.
Chest X – ray and ECG with medical and anesthetic fitness.
7.4 Has ethical clearance been obtained from your institution in case of 7.3?
Yes 8 LIST OF REFERENCES:
1. Arakeri G, Brennan PA. Oral submucous fibrosis: an overview of the aetiology,
pathogenesis, classification, and principles of management. Br J Oral Maxillofac Surg. 2012 Oct
26.(Article in press)
2. Rastogi S, Modi M, Sathian B. The Efficacy of Collagen Membrane as a Biodegradable
Wound Dressing Material for Surgical Defects of Oral Mucosa: A Prospective Study. J Oral
Maxillofacial Surg 2009 ;67:1600-160.
3. Nataraj S, Guruprasad Y, Shetty JN. A Comparative Clinical Evaluation Of Buccal
Fat Pad And Collagen In Surgical Management Of Oral Submucous Fibrosis. Archives of
Dental Sciences 2011; 2: 15-22.
4. Paramhans D, Mathur RK, Newaskar V, Shukla S, Sudrania MK. Role of collagen
membrane for reconstruction of buccal defects following fibrotic band excision and
coronoidectomy in Oral submucous fibrosis. World Articles in Ear Nose and Throat 2010; 3(1).
5. Yoshiga K, Ichikawa T, Kayada Y, Miyauchi S., Tsumura M, Sakurai K et al. Repair
of Mucosal Defects With Atelocollagen and Its Indications. The Journal of Hiroshima
University Dental Society 1995; 27(2): 459-468
6. Ko EC, Shen YH, Yang CF, Huang IY, Shieh TY, Chen CM. Artificial dermis as the
substitute for split-thickness skin graft in the treatment of oral submucous fibrosis. J Craniofac
Surg. 2009 Mar; 20(2): 443-5
9. SIGNATURE OF THE CANDIDATE
10. REMARKS OF THE GUIDE
11. NAME & DESIGNATION OF DR. RAJENDRA DESAI. (in block letters) PROFESSOR, 11.1 GUIDE DEPARTMENT OF ORAL AND MAXILLOFACIAL SURGERY, COLLEGE OF DENTAL SCIENCES, DAVANGERE - 577004. KARNATAKA.
11.2 SIGNATURE
11.3 CO-GUIDE (IF ANY)
11.4 SIGNATURE 11.5 HEAD OF THE DEPARTMENT DR. SIVA BHARANI K. S. N. PROFESSOR AND HEAD, DEPARTMENT OF ORAL AND MAXILLOFACIAL SURGERY, COLLEGE OF DENTAL SCIENCES, DAVANGERE - 577004. KARNATAKA.
11.6 SIGNATURE
12. 12.1 REMARKS OF THE CHAIRMAN & PRINCIPAL
12.2 SIGNATURE