ASSESSMENT OF THE NEONATE
INITIAL ASSESSMENT OF THE NEONATE- OVERVIEW
Antenatal history – Was the pregnancy free of risk factors?
Perinatal factors – Are the following satisfactory? Fetal and / or cord blood gas, CTG monitoring, presence of fetal distress?
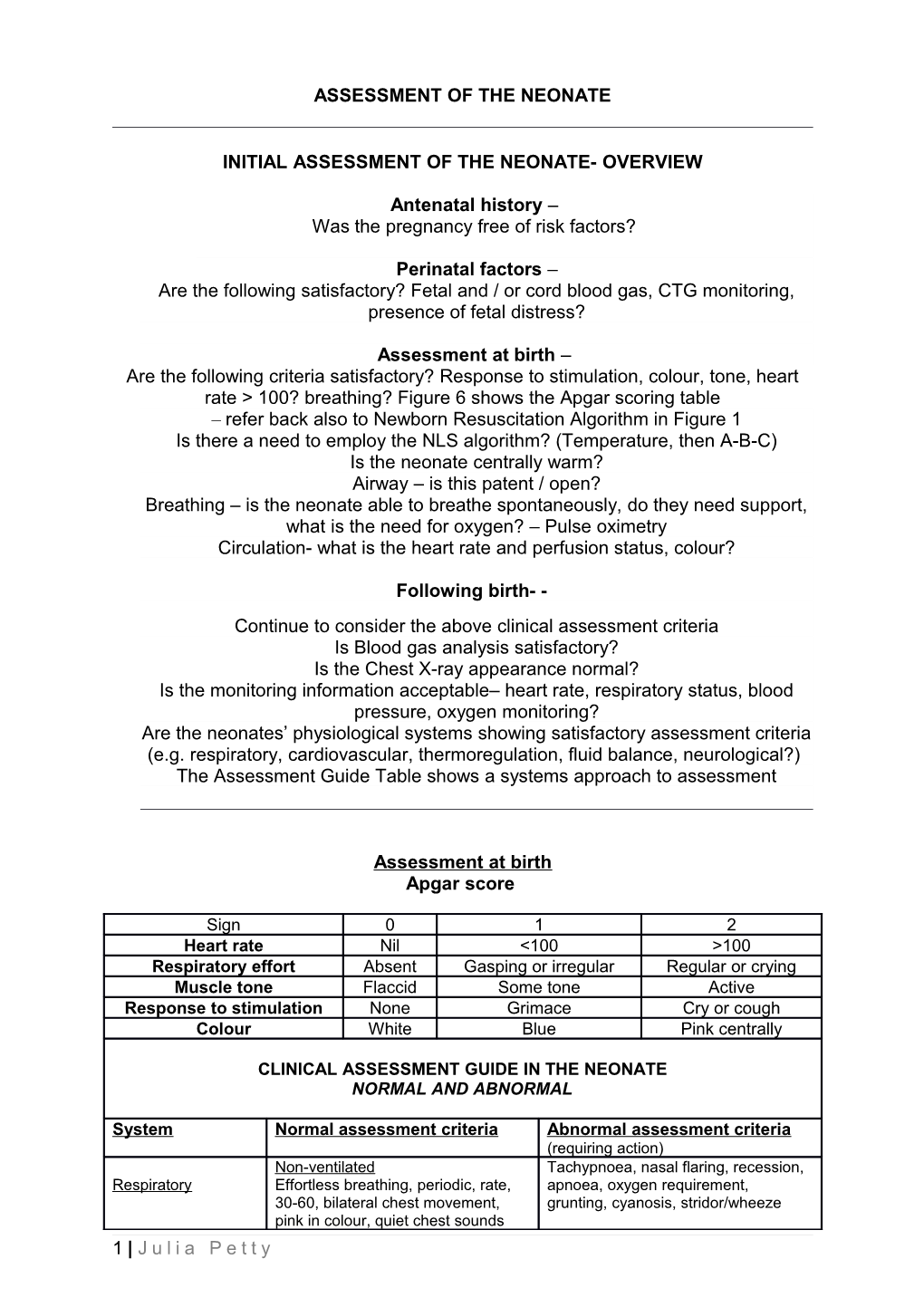
Assessment at birth – Are the following criteria satisfactory? Response to stimulation, colour, tone, heart rate > 100? breathing? Figure 6 shows the Apgar scoring table – refer back also to Newborn Resuscitation Algorithm in Figure 1 Is there a need to employ the NLS algorithm? (Temperature, then A-B-C) Is the neonate centrally warm? Airway – is this patent / open? Breathing – is the neonate able to breathe spontaneously, do they need support, what is the need for oxygen? – Pulse oximetry Circulation- what is the heart rate and perfusion status, colour?
Following birth- - Continue to consider the above clinical assessment criteria Is Blood gas analysis satisfactory? Is the Chest X-ray appearance normal? Is the monitoring information acceptable– heart rate, respiratory status, blood pressure, oxygen monitoring? Are the neonates’ physiological systems showing satisfactory assessment criteria (e.g. respiratory, cardiovascular, thermoregulation, fluid balance, neurological?) The Assessment Guide Table shows a systems approach to assessment
Assessment at birth Apgar score
Sign 0 1 2 Heart rate Nil <100 >100 Respiratory effort Absent Gasping or irregular Regular or crying Muscle tone Flaccid Some tone Active Response to stimulation None Grimace Cry or cough Colour White Blue Pink centrally
CLINICAL ASSESSMENT GUIDE IN THE NEONATE NORMAL AND ABNORMAL
System Normal assessment criteria Abnormal assessment criteria (requiring action) Non-ventilated Tachypnoea, nasal flaring, recession, Respiratory Effortless breathing, periodic, rate, apnoea, oxygen requirement, 30-60, bilateral chest movement, grunting, cyanosis, stridor/wheeze pink in colour, quiet chest sounds 1 | J u l i a P e t t y Ventilated Even, bilateral chest movement, air Chest movement ceases, entry clear and bilateral, no uneven/unilateral, excess secretions, secretions evident, ETT fixed and absent breath sounds on one or both secure sides. Think DOPPES (Displacement of tube? / Obstruction? / Pneumothorax? / Pulmonary haemorrhage / Equipment? / Stiff lungs) Adequate mean blood pressure MBP below desired limit, pale, cool Cardiovascular (MBP), capillary refill less than 2 skin, low/diminishing urine output, seconds, urine output at least capillary refill > 2 seconds, widening 1ml/kg/hour, pink in colour, warm toe-core temperature difference, skin, toe-core temperature difference weak, thready pulse, bradycardia 1-2 degrees Celsius, palpable pulses, adequate heart rate Adequate systemic perfusion and Poor systemic perfusion and low urine Fluid status and urine output (see above), normal / output (1ml/kg/hour) (see above) or balance palpable fontanelles, palpable polyuria, sunken or bulging peripheral pulses, good skin turgor, fontanelles, dry skin, fast and thready normal sodium level, specific gravity pulses, high or low specific gravity, of urine 1.010 – 1.020, weight gain large increases or decreases in appropriate for age, equal fluid weight, large positive or negative fluid balance (in and out) for 24 hr balance balance Soft, non-tender abdomen, bowel Distended, tender, hard abdomen, no Gastro-intestinal and sounds, nil/minimal aspirate from bowel sounds or bowel actions, stool nutritional status stomach which is clear and bloody/too loose / green/ large and/or mucousy, bowels open and normal increasing stomach aspirates, bile stool, no vomiting, tolerance of feeds aspirates, vomiting, failure to tolerate if applicable, blood sugar > 2.6 feeds, hypo /hyperglycaemia(<2.6 or > mmols in first week, then 4-6mmols 7) thereafter. Consider: Abnormal posture and tone, e.g. hypo Neurological & 1. tone or hypertonia, unresponsive or less sensory 2. movement responsive to stimuli, abnormal movements such as convulsions, 3. response to stimuli excessive wakefulness or lack of 4. level of consciousness consciousness. Normal flexed posture (term) or extended limbs (if preterm), normal/present reflexes according to gestation and age, reactions to stimuli as appropriate to gestation, normal tone and movements System - continued Normal assessment criteria - Abnormal assessment criteria – continued continued (requiring action) Immunological Signs of infection not evident Signs of infection may be non-specific and include respiratory distress, colour change, changes to pulse oximetry values, oxygen requirement, changes in vital signs, apnoea, abnormal values on blood gas – e.g. metabolic acidosis, white cell count and platelets and sodium drops for example. Thermoregulation Normal body temperature (36.5 Temperature < 36.5 or > 37.3 – i.e. -37.2 degrees Celsius) and thermal instability (or ‘thermal stress’) appropriate environmental is present. temperature according to age and gestation/birth weight Skin and general Normal skin for gestation, e.g.: frail Broken, excoriated skin, rashes, and appearance and red in the preterm, and well tissued I.V. sites or suspected, formed in term, pink mucous clinically jaundiced, blue mucous
2 | J u l i a P e t t y membranes, no excoriation, no signs membranes. of jaundice, umbilical area clean, I.V. sites healthy Developmental and No presence of pain or stress. Presence of pain or stress according Environmental Consider gestation. to cues- for example, tense, care (includes Neonate is positioned appropriately- continual movements, facial pain/stress) flexed, limbs in mid-line, appears expressions, excessive crying comfortable, relaxed and able to and grimace, changes to vital sleep for long periods. signs, colour change, apnoea, desaturations.
Family Family adjustment to their neonate Signs of mal-adjustment or inability to being admitted to a neonatal cope should be noted and unit must be considered. referred to appropriate multi- Parents / family members will disciplinary team member. be anxious and need Consider the adverse explanation and information – psychological effects of preterm this is to be expected and done birth and hospitalisation along in a sensitive and with chronic illness – e.g. compassionate manner. Assess depression, dysfunctional what the family needs in view behaviours & conflicts. psychological, social, practical & multi-disciplinary support.
References: Adapted from various sources; Boxwell (2010), Baston & Durward (2010), Lissauer & Faneroff (2011) and Lomax (2011) Stanford Newborn Nursery website http://newborns.stanford.edu/PhotoGallery/General.html
3 | J u l i a P e t t y