Spirometry. Whole body plethysmography
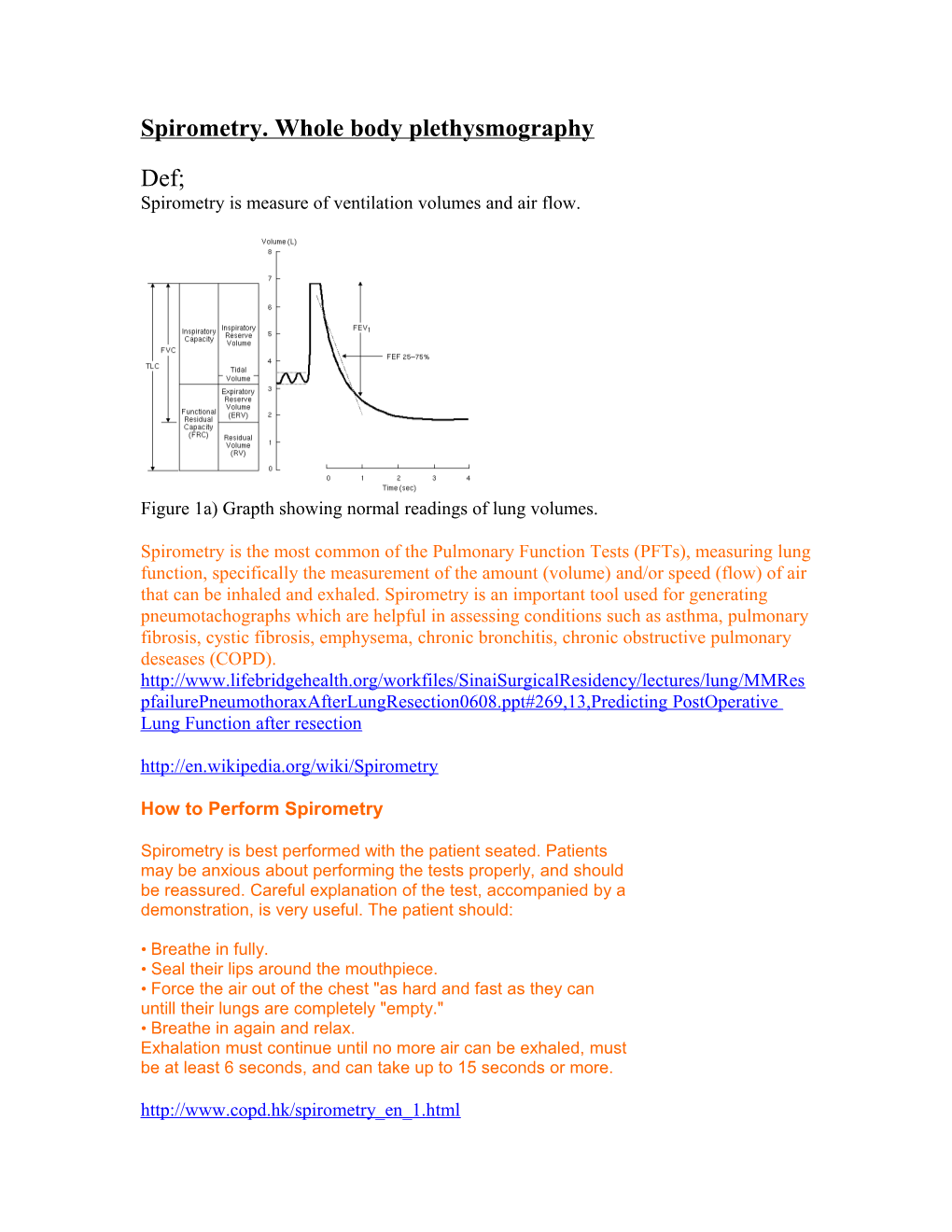
Def; Spirometry is measure of ventilation volumes and air flow.
Figure 1a) Grapth showing normal readings of lung volumes.
Spirometry is the most common of the Pulmonary Function Tests (PFTs), measuring lung function, specifically the measurement of the amount (volume) and/or speed (flow) of air that can be inhaled and exhaled. Spirometry is an important tool used for generating pneumotachographs which are helpful in assessing conditions such as asthma, pulmonary fibrosis, cystic fibrosis, emphysema, chronic bronchitis, chronic obstructive pulmonary deseases (COPD). http://www.lifebridgehealth.org/workfiles/SinaiSurgicalResidency/lectures/lung/MMRes pfailurePneumothoraxAfterLungResection0608.ppt#269,13,Predicting PostOperative Lung Function after resection http://en.wikipedia.org/wiki/Spirometry
How to Perform Spirometry
Spirometry is best performed with the patient seated. Patients may be anxious about performing the tests properly, and should be reassured. Careful explanation of the test, accompanied by a demonstration, is very useful. The patient should:
• Breathe in fully. • Seal their lips around the mouthpiece. • Force the air out of the chest "as hard and fast as they can untill their lungs are completely "empty." • Breathe in again and relax. Exhalation must continue until no more air can be exhaled, must be at least 6 seconds, and can take up to 15 seconds or more. http://www.copd.hk/spirometry_en_1.html What does sprometer measure
FEV1 - Forced Expiratory Volume in one second. This is the amount of air you can blow out within one second.
FVC - Forced Vital Capacity. The total amount of air that you blow out in one breath. (FEV1/FVC). Of the total amount of air that you can blow out in one breath, this is the proportion that you can blow out in one second.
What can measurements show
A spirometry reading usually shows one of four main patterns:
Normal An obstructive pattern A restrictive pattern A combined obstructive / restrictive pattern http://www.surgerydoor.co.uk/medcons/print.asp?Recno=23069330
Normal
Figure 1b) Graph showing normal flow-volume curve.
Recording varies according to age, size and sex. In the graph, positive values shows exhaled volumes (expiration) in litters per second and negative values shows inhaled volumes (inspiration). Y axis show floe per time and x axis show volume in litters Obstructive pattern
Figure 1c) Graph of obstructive deseases in flow-volume curve
Typical deseases that can cause narrowing of the air way include COPD (mostly emphysema and broncholitis).
If your airways are narrowed, then the amount of air that you can blow out quickly is reduced. So, your FEV1 is reduced and the ratio FEV1/FVC is lower than normal. Obstructive diseases maybe diagnosed if FEV1 is less than 80% of predicted values according to age, sex, size or FEV1\FVC ratio is 0.7 or less. Severe air flow obstruction count for FEV1 is 30% or less than predicted values.
However, with narrowed airways, the total capacity of your lungs is often normal or only mildly reduced. So, with an obstructive pattern the FVC is often normal or near normal. http://www.surgerydoor.co.uk/medcons/print.asp?Recno=23069330 http://www.patient.co.uk/showdoc/27000436/
Restrictive pattern
Figure 1d) Graph of restrictive diseases in flow-volume curve With a restrictive spirometry pattern your FVC is less than the predicted value for your age, sex and size. This is caused by various conditions that affect the lung tissue itself, or affect the capacity of the lungs to expand and hold a normal amount of air. For example, conditions that cause fibrosis or scarring of the lung such as pneumoconiosis. Or, a physical deformity that restricts the expansion of the lungs. Your FEV1 is also reduced but this is proportion to the reduced FVC. So, with a restrictive pattern the ratio of FEV1/FVC is normal. http://www.patient.co.uk/showdoc/27000436/
Restrictive patterns can be due to reduced lung compliance or reduced compliance of the alveolar. It can also be due to stiffness of the rib cage due to burns. Therefore reduced compliance lead to increased static resistance hence low static lung volumes especially low values of VC and FVC. Normal lung but lung volumes reduced.
Whole body plethysmography
Some lung volumes can not be measured by simple spirometry eg residual lung volume (RV). In order to measure it, you need to do whole body plethysmography to know total lung capacity (TLC).
It is a very sensitive lung measurement used to detect lung pathology that might be missed with conventional pulmonary functional tests.
It is done by enclosing the whole body if in a chamber often known as Body Box, a pneumotachometer is used to measure airflow while a mouth pressure transducer with a shutter measures the alveolar pressure. The most common measurements made using body plethysmographs are thoracic gas volume (VTG) and airway resistance (RAW). http://en.wikipedia.org/wiki/Body_plethysmography If the total volume of body box is 1000L, and normal breathing around 1.5L, the remaining volume in body box is 998.5L,if the person is asked to breath in, usually 6L,the remaining volume is 994L. And also the pressure is the alveolar is difficult to measure, in order to measure it, the patient is asked to expire and then the tube is blocked and the increase in lung pressure rises and become equal to the pressure in the mouth piece tube, then the alveolar pressure is measured in this way. But it should be done for short time since its not comfortable.
With this values the formula PiVi=PfVf can be used if other parameters are known.
Whole body plethysmography is also essential in detecting COPD diseases.
Reference http://patf-biokyb.lf1.cuni.cz/wiki/vyuka/stanislav_matousek http://en.wikipedia.org/wiki/Spirometry
Stephen J.M et al:Pathophysiology of disease, san Francisco, California,2002
PLAGIARISM SOURCES: 26.5%