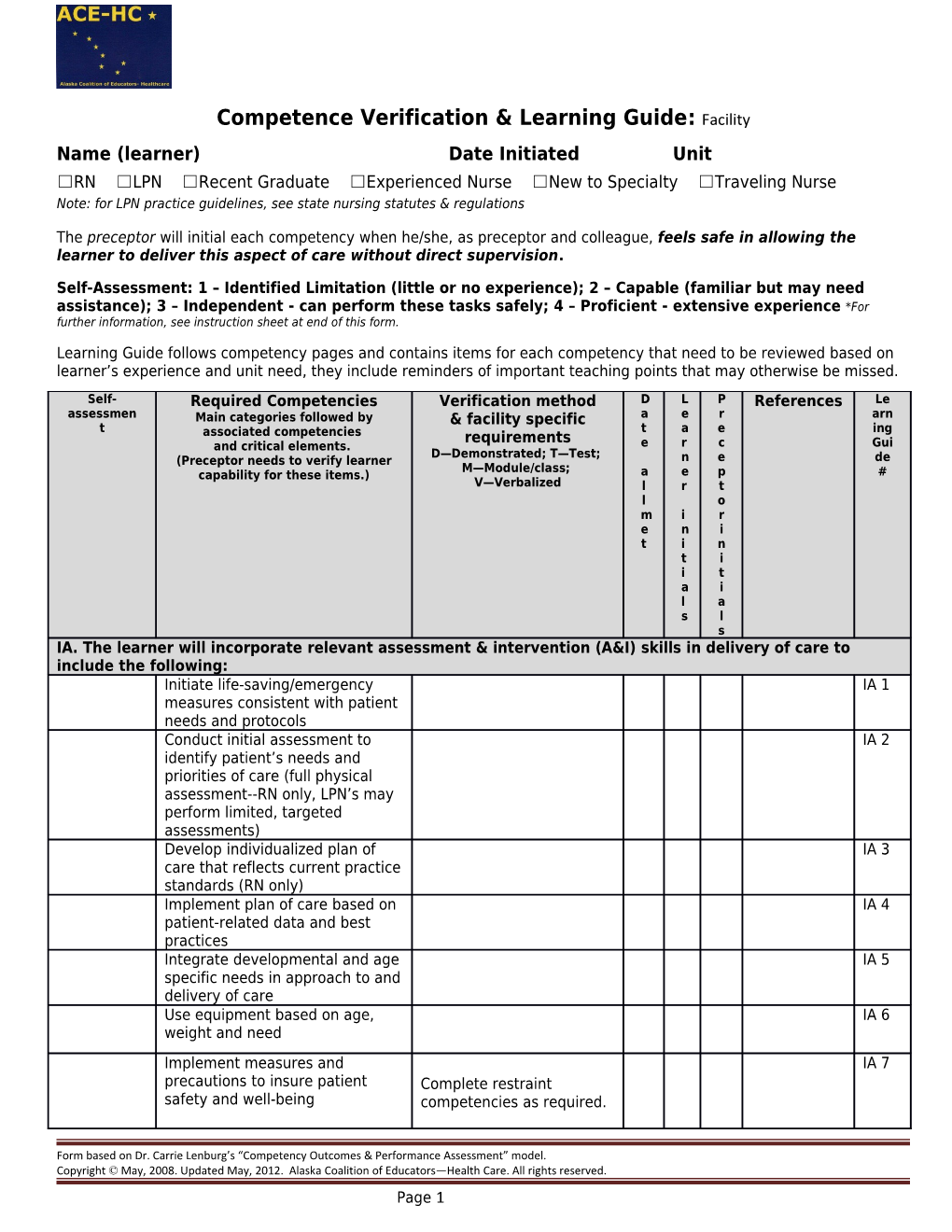
Competence Verification & Learning Guide: Facility Name (learner) Date Initiated Unit ☐RN ☐LPN ☐Recent Graduate ☐Experienced Nurse ☐New to Specialty ☐Traveling Nurse Note: for LPN practice guidelines, see state nursing statutes & regulations
The preceptor will initial each competency when he/she, as preceptor and colleague, feels safe in allowing the learner to deliver this aspect of care without direct supervision.
Self-Assessment: 1 – Identified Limitation (little or no experience); 2 – Capable (familiar but may need assistance); 3 – Independent - can perform these tasks safely; 4 – Proficient - extensive experience *For further information, see instruction sheet at end of this form.
Learning Guide follows competency pages and contains items for each competency that need to be reviewed based on learner’s experience and unit need, they include reminders of important teaching points that may otherwise be missed. Self- Required Competencies Verification method D L P References Le assessmen Main categories followed by & facility specific a e r arn t t a e ing associated competencies requirements and critical elements. e r c Gui D—Demonstrated; T—Test; (Preceptor needs to verify learner n e de M—Module/class; capability for these items.) a e p # V—Verbalized l r t l o m i r e n i t i n t i i t a i l a s l s IA. The learner will incorporate relevant assessment & intervention (A&I) skills in delivery of care to include the following: Initiate life-saving/emergency IA 1 measures consistent with patient needs and protocols Conduct initial assessment to IA 2 identify patient’s needs and priorities of care (full physical assessment--RN only, LPN’s may perform limited, targeted assessments) Develop individualized plan of IA 3 care that reflects current practice standards (RN only) Implement plan of care based on IA 4 patient-related data and best practices Integrate developmental and age IA 5 specific needs in approach to and delivery of care Use equipment based on age, IA 6 weight and need Implement measures and IA 7 precautions to insure patient Complete restraint safety and well-being competencies as required.
Form based on Dr. Carrie Lenburg’s “Competency Outcomes & Performance Assessment” model. Copyright © May, 2008. Updated May, 2012. Alaska Coalition of Educators—Health Care. All rights reserved. Page 1 Self- Required Competencies Verification method D L P References Le assessmen Main categories followed by & facility specific a e r arn t t a e ing associated competencies requirements and critical elements. e r c Gui D—Demonstrated; T—Test; (Preceptor needs to verify learner n e de M—Module/class; capability for these items.) a e p # V—Verbalized l r t l o m i r e n i t i n t i i t a i l a s l s Promote increase in client IA 8 independence teach/assist patients with PT/OT/ST per protocols maximize client decision making Implement mental health & IA 9 alcohol/substance abuse behavior protocols Manage patient on cardiac IA 10 monitor place leads correctly
interpret rhythm correctly
intervene as needed
Manage nutritional support - IA 11 recognize need manage tube feedings per protocol administer total parenteral nutrition per protocol
IB. The learner will incorporate relevant A & I skills in delivery of medications, IV’s & blood to include the following:
Form based on Dr. Carrie Lenburg’s “Competency Outcomes & Performance Assessment” model. Copyright © May, 2008. Updated May, 2012. Alaska Coalition of Educators—Health Care. All rights reserved. Page 2 Self- Required Competencies Verification method D L P References Le assessmen Main categories followed by & facility specific a e r arn t t a e ing associated competencies requirements and critical elements. e r c Gui D—Demonstrated; T—Test; (Preceptor needs to verify learner n e de M—Module/class; capability for these items.) a e p # V—Verbalized l r t l o m i r e n i t i n t i i t a i l a s l s Administer medication to IB 1 assigned patients complete procedural implement safe practice with sedation competency if high risk medication req’d implement the “rights” of med administration state indications, contra- indications and side effects (may use reference) administer IVPB solution
administer IV push/bolus med (RN only) Manage peripheral IV care IB 2 consistent with protocols verbalize pediatric and geriatric volume and dosage precautions Manage central/PICC line IB 3 consistent with protocols complete PICC use correct flush solution and competency if required technique apply policy for clotted line
assess site for complications NOTE: LPN’s limited to specific training per state regs Administer blood/blood products IB 4 (RN only) per protocol Perform venipuncture on an adult IB 5 &/or child or infant heel stick as applicable
IC. The learner will incorporate relevant A & I skills in performing procedures & utilizing equipment to
Form based on Dr. Carrie Lenburg’s “Competency Outcomes & Performance Assessment” model. Copyright © May, 2008. Updated May, 2012. Alaska Coalition of Educators—Health Care. All rights reserved. Page 3 Self- Required Competencies Verification method D L P References Le assessmen Main categories followed by & facility specific a e r arn t t a e ing associated competencies requirements and critical elements. e r c Gui D—Demonstrated; T—Test; (Preceptor needs to verify learner n e de M—Module/class; capability for these items.) a e p # V—Verbalized l r t l o m i r e n i t i n t i i t a i l a s l s include: Integrate sterile technique into IC 1 practice according to agency policy Perform point of care testing per IC 2 lab and unit protocols by completing all required competencies Utilize protocols and other IC 3 references for unfamiliar or infrequently used procedures and equipment Administer oxygen safely as IC 4 ordered
Perform the following types of IC 5 suctioning as apply: trach suctioning
naso or oropharyngeal
bulb, yankaur, olive tip
Manage a nasogastric tube per IC 6 protocol
Implement pain management IC 7 protocol initiate pain pump(s) used in unit (RN only)
Manage patient pre-, during, and IC 8 post-procedure per protocol Also see separate comp for procedural sedation if applies Perform wound care consistent IC 9 with protocols Incorporate regulatory IC 10 requirements into practice
Form based on Dr. Carrie Lenburg’s “Competency Outcomes & Performance Assessment” model. Copyright © May, 2008. Updated May, 2012. Alaska Coalition of Educators—Health Care. All rights reserved. Page 4 Self- Required Competencies Verification method D L P References Le assessmen Main categories followed by & facility specific a e r arn t t a e ing associated competencies requirements and critical elements. e r c Gui D—Demonstrated; T—Test; (Preceptor needs to verify learner n e de M—Module/class; capability for these items.) a e p # V—Verbalized l r t l o m i r e n i t i n t i i t a i l a s l s
Section II. The learner will incorporate relevant communication skills in all interactions to include the following: Document care given and patient II 1 response accurately in health care record. Interact in a respectful and II 2 collaborative manner with the healthcare team. Report pertinent, concise II 3 information to team members per policy Demonstrate verbal and II 4 nonverbal therapeutic communication with patients and staff
Section III. The learner will incorporate critical thinking skills in delivery of all nursing care to include the following: Analyze patient laboratory data III 1 to use it in clinical decision making Manage unit phone calls per III 2 policy Prepare for moving a patient III 3 between levels of care within the facility or to/from another facility Use resources effectively III 4 respond to significant changes in patient status per protocols and orders notify charge nurse or manager of significant changes or needs on unit
Form based on Dr. Carrie Lenburg’s “Competency Outcomes & Performance Assessment” model. Copyright © May, 2008. Updated May, 2012. Alaska Coalition of Educators—Health Care. All rights reserved. Page 5 Self- Required Competencies Verification method D L P References Le assessmen Main categories followed by & facility specific a e r arn t t a e ing associated competencies requirements and critical elements. e r c Gui D—Demonstrated; T—Test; (Preceptor needs to verify learner n e de M—Module/class; capability for these items.) a e p # V—Verbalized l r t l o m i r e n i t i n t i i t a i l a s l s Anticipate potential unit / patient III 5 crises and act to prevent them or minimize their impact Perform nursing role within scope III 6 of practice, unit limitations and individual competency use reflective judgment in self- assessment &planning recognizes own limitations
create a plan for ongoing development of decision making ability
Section IV. The learner will incorporate human caring & relationship skills in all interactions to include the following: Advocate for patient and family IV 1 needs
Assist patient/family with ethical IV 2 and/or legal issues with sensitivity Display empathy, compassion IV 3 and respect to patients and families Maintain patient privacy and IV 4 confidentiality at all times Assist colleagues with care IV 5 delivery Incorporate cultural competence IV 6 and respect for diversity into practice Provide palliative care as part of IV 7 the continuum of care.
Form based on Dr. Carrie Lenburg’s “Competency Outcomes & Performance Assessment” model. Copyright © May, 2008. Updated May, 2012. Alaska Coalition of Educators—Health Care. All rights reserved. Page 6 Self- Required Competencies Verification method D L P References Le assessmen Main categories followed by & facility specific a e r arn t t a e ing associated competencies requirements and critical elements. e r c Gui D—Demonstrated; T—Test; (Preceptor needs to verify learner n e de M—Module/class; capability for these items.) a e p # V—Verbalized l r t l o m i r e n i t i n t i i t a i l a s l s Section V. The learner will incorporate management skills in all interactions to include the following: Plan shift to accomplish tasks and V1 goals organize workload effectively
prioritize and reprioritize work as needs change complete tasks or seek help Manage assignment V2 complete full patient assignment ask for advice and delegate as needed Manage self V3 manage personal professional development keep certifications, license & employee health records current, wear appropriate attire and ID maintain calm, professional behavior during stressful situations use correct body mechanics and resources to prevent injury Identify area of interest in quality improvement (committees, projects, workgroups, etc.)
Section VI. The learner will incorporate leadership skills in all interactions to include the following:
Form based on Dr. Carrie Lenburg’s “Competency Outcomes & Performance Assessment” model. Copyright © May, 2008. Updated May, 2012. Alaska Coalition of Educators—Health Care. All rights reserved. Page 7 Self- Required Competencies Verification method D L P References Le assessmen Main categories followed by & facility specific a e r arn t t a e ing associated competencies requirements and critical elements. e r c Gui D—Demonstrated; T—Test; (Preceptor needs to verify learner n e de M—Module/class; capability for these items.) a e p # V—Verbalized l r t l o m i r e n i t i n t i i t a i l a s l s Complete Clinical Nursing Complete leadership VI 1 Leadership Competence competency form if required (charge nurse, manager, house supervisor, preceptor, etc.) Supervise staff VI 2 monitor performance of supervised staff assist staff as needed
provide feedback to staff & management as needed Delegate work fairly and VI 3 according to skill level and scope of practice Coordinate care with healthcare VI 4 team Initiate chain of command VI 5
Section VII. The learner will incorporate teaching skills in delivery of all nursing care to include the following: Educate patients and families VII 1 with consideration for age, culture, educational background and home environment or setting Provide education to complete a VII 2 successful patient discharge per policy Coordinate education to ensure VII 3 the patient gets a consistent message
Section VIII. The learner will incorporate knowledge integration skills to include the following:
Form based on Dr. Carrie Lenburg’s “Competency Outcomes & Performance Assessment” model. Copyright © May, 2008. Updated May, 2012. Alaska Coalition of Educators—Health Care. All rights reserved. Page 8 Self- Required Competencies Verification method D L P References Le assessmen Main categories followed by & facility specific a e r arn t t a e ing associated competencies requirements and critical elements. e r c Gui D—Demonstrated; T—Test; (Preceptor needs to verify learner n e de M—Module/class; capability for these items.) a e p # V—Verbalized l r t l o m i r e n i t i n t i i t a i l a s l s Identify care issues within the VIII 1 rural environment Provide nursing care that is VIII 2 evidence based Use all computer systems VIII 3 successfully Accept teaching, coaching and VIII 4 mentoring to improve competence Seek continued learning VIII 5 opportunities to improve practice
Comments/alternative learning plans:
All preceptors are to sign & initial below. Ideally new graduates should have only one to two preceptors for the entire orientation. Preceptor Signature Initials Preceptor Signature Initials
Signatures at completion of preceptorship/orientation:
Preceptee/orientee Date
Primary Preceptor Date
Form based on Dr. Carrie Lenburg’s “Competency Outcomes & Performance Assessment” model. Copyright © May, 2008. Updated May, 2012. Alaska Coalition of Educators—Health Care. All rights reserved. Page 9 Manager Date
Form based on Dr. Carrie Lenburg’s “Competency Outcomes & Performance Assessment” model. Copyright © May, 2008. Updated May, 2012. Alaska Coalition of Educators—Health Care. All rights reserved. Page 10 LEARNER GUIDE: Reference content in the right-hand column that needs review. IA. The learner will incorporate relevant assessment & intervention (A&I) skills in delivery of care to include the following: IA 1 Initiate life-saving/emergency measures Review procedures for: consistent with patient needs and protocols -Correct response for all codes -Obtaining/interpreting an ECG -Emergency intubation -Allergic reaction (also latex allergy) -Seizure precautions including patient positioning/padding -Hyper and hypoglycemic episodes -Hyper and hypothermic episodes -Suicide prevention precautions -Nonviolent crisis intervention -Pediatric emergencies (including medication dosing and crash cart supplies -GI, post partum, other significant bleeds -Reporting abuse/neglect -Use of emergency equipment -Cardiac emergencies -Poison/overdose management
IA 2 Conduct initial assessment to identify Review the following: patient’s needs and priorities of care (full -How to complete all intake forms & processes physical assessment--RN only, LPN’s may -How to complete assessment to identify primary needs of perform limited, targeted assessments) patient -How to distinguish abnormal from normal signs and symptoms -How to address age specific needs -Immunization policies (Review vaccination database--VAK TRAK or other) -Policy for treatment of minors and at risk adults -Skin integrity assessment and protocols -Physical, psychological, social and spiritual aspects of assessment
IA 3 Develop individualized plan of care that Review care plan process and documentation requirements reflects current practice standards (RN only) IA 4 Implement plan of care based on patient- Review priority setting practices and discharge criteria related data and best practices IA 5 Integrate developmental and age specific Review the following: needs in approach to and delivery of care -VS parameters -Communication techniques -Physical, developmental, spiritual & emotional needs
IA 6 Use equipment based on age, weight and Review the use of equipment (scales, pumps, restraints, lifts, need etc.) in regards to age and weight.
Form based on Dr. Carrie Lenburg’s “Competency Outcomes & Performance Assessment” model. Copyright © May, 2008. Updated May, 2012. Alaska Coalition of Educators—Health Care. All rights reserved. Page 11 LEARNER GUIDE: Reference content in the right-hand column that needs review. IA 7 Implement measures and precautions to Review the following: insure patient safety and well-being -Wandering & fall prevention protocols -Patient identification measures -Restraint and seclusion policy including: assessing need for continued restraint, using least restraint necessary, and monitoring for complications/patient needs -Infection control policy including hand hygiene, personal protective equipment, patient isolation (respiratory, wound, neutropenic, etc.) and contaminated waste policies -Nosocomial risks: delirium, UTI’s, central line infections, pressure ulcers, etc. -Unusual occurrence reports
IA 8 Promote increase in client independence Review physical, occupational and speech therapy procedures, introduce to PT/OT/ST team, review resources & equipment available and methods to support family involvement
IA 9 Implement mental health & alcohol/substance Review mental health policies re: suicide watch, behavioral abuse behavior protocols management, consultations Review alcohol/substance abuse protocols and pathophysiology Review process for transferring to other facilities
IA Manage patient on cardiac monitor Review procedures and monitoring equipment and policies for 10 handling abnormal rhythms Review rhythm interpretation
IA Manage nutritional support - recognize need Review protocols, available types of tube feeding, nutritional 11 supplements and diets. Introduce to dietary personnel
IB. The learner will incorporate relevant A & I skills in delivery of medications, IV’s & blood to include the following: IB 1 Administer medication to assigned patients Review medication administration policies and reference materials including med reconciliation and narcotic accounting Introduce to pharmacist and review pharmacy role and availability Must pass unit/hospital medication test if required before allowed to administer meds Review limits to medication administration (formulary, restricted meds, high alert meds)
IB 2 Manage peripheral IV care consistent with Practice with related equipment (syringe pump, IV pump and protocols corresponding supplies) Review policies re: preparing IV meds, approved IV medication list per unit Review geriatric and pediatric considerations re: volume and dosages
Form based on Dr. Carrie Lenburg’s “Competency Outcomes & Performance Assessment” model. Copyright © May, 2008. Updated May, 2012. Alaska Coalition of Educators—Health Care. All rights reserved. Page 12 LEARNER GUIDE: Reference content in the right-hand column that needs review. IB 3 Manage central/PICC line consistent with Review policies on flushing, drawing blood, declotting, dressing protocols change, removal and general care of all central catheters NOTE: LPN’s limited to specific training per used in the facility (PICC, triple lumen, groshong, portacath, state statutes etc.) Complete any specialty line competencies as required
IB 4 Administer blood/blood products (RN only) Review blood bank and nursing policies and procedure for per protocol transfusion of blood products Review actions to take if suspected reaction occurs Review massive transfusion, autologous transfusion and giving uncross-matched blood policies
IB 5 Perform venipuncture on an adult &/or child Review lab and nursing policies related to blood sampling or infant heel stick as applicable Review blood culture protocol
IC. The learner will incorporate relevant A & I skills in performing procedures & utilizing equipment to include the following: IC 1 Integrate sterile technique into practice If not demonstrated in patient care, have learner simulate a according to agency policy sterile dressing change, foley insertion or other sterile procedure.
IC 2 Perform point of care testing per lab and unit Review testing and quality control for the following as apply: protocols by completing all required rapid strep, glucometer, urine chemistry strip, occult blood, competencies urine pregnancy tests, iStat, Ferning test
IC 3 Utilize protocols and other references for Review how and where to access all procedures, manuals and unfamiliar or infrequently used procedures instructions. and equipment Infrequent procedures may include post-mortem care, organ donation, and many others Equipment may include heating or cooling devices, fluid warmers, and many others
IC 4 Administer oxygen safely as ordered Review types of O2 equipment (cannula, NRB, BVM, ventimask and aerosol mask, tanks, etc.) Review O2 monitoring and signs of toxicity Set up and use pulse oximetry Review peak flow measurement
IC 5 Perform the following types of patient Review procedures for suctioning including safety suctioning as apply considerations
IC 6 Manage a nasogastric tube per protocol Review protocols including how to assess placement/proper function Practice insertion as needed
IC 7 Implement pain management protocol Review policies Assess and reassess every patient for pain For epidural, and PCA: specifically review equipment manual, pain management techniques, teaching, troubleshooting and documentation Review role of anesthesiology dept for epidurals
Form based on Dr. Carrie Lenburg’s “Competency Outcomes & Performance Assessment” model. Copyright © May, 2008. Updated May, 2012. Alaska Coalition of Educators—Health Care. All rights reserved. Page 13 LEARNER GUIDE: Reference content in the right-hand column that needs review. IC 8 Manage patient pre-, during, and post- Review pre-op preparation and paperwork including site check procedure per protocol Review protocols (including time out) for procedures performed in the unit (thoracentesis, paracentesis, spinal tap, etc.) Review protocols for post-op/unit procedure recovery & potential complications
IC 9 Perform wound care consistent with protocols Review procedures and equipment (wound vacc, drains, etc.) Introduce to any resource personnel (ostomy/wound care nurse)
IC Implement regulatory requirements into National patient safety goals, CMS guidelines, Joint 10 practice Commission, core measures, etc.
Section II. The learner will incorporate relevant communication skills in all interactions to include the following: II 1 Document care given and patient response Review charting policy, forms, and computer programs. accurately in health care record. II 2 Interact in a respectful and collaborative Meet team members and review roles and responsibilities of manner with the healthcare team. each
II 3 Report pertinent, concise information to team Review hand-off report, info to share with charge nurse, members per policy manager, MD’s, etc. Review how to reach team members (pager, phone, etc.)
II 4 Demonstrate verbal and noverbal therapeutic Review care models for the organization (rounding, family communication with patients and staff driven care, etc.) Review organizational behavior standards
Section III. The learner will incorporate critical thinking skills in delivery of all nursing care to include the following: III 1 Analyze patient laboratory data to use it in Review lab norms and reports including fluid and electrolyte clinical decision making management and critical values
III 2 Manage unit phone calls per policy Review telephone triage policy (RN only) Review Health Aide roles and capabilities Review types of calls, scope of practice and information sharing limitations
III 3 Prepare for moving a patient between levels Review ground and air transfer policies and logistics of care within the facility or to/from another Review EMTALA and medivac protocols facility III 4 Use resources effectively Review order sets and protocols and notification process Review after hour protocols, acuity process, supplies, etc.
III 5 Anticipate potential unit / patient crises and Review frequently occurring unit patient intervention needs act to prevent them or minimize their impact Review unusual occurrence reporting system Discuss failure to rescue Review rapid response team role if available
Form based on Dr. Carrie Lenburg’s “Competency Outcomes & Performance Assessment” model. Copyright © May, 2008. Updated May, 2012. Alaska Coalition of Educators—Health Care. All rights reserved. Page 14 LEARNER GUIDE: Reference content in the right-hand column that needs review. III 6 Perform nursing role within scope of practice, Review ANA and specialty standards, nurse practice act unit limitations and individual competency Review limitations of unit and competency process
Section IV. The learner will incorporate human caring & relationship skills in all interactions to include the following: IV 1 Advocate for patient and family needs Review policy for patient complaints, advocacy and ethics
IV 2 Assist patient/family with ethical and/or legal Review policy and resources for patient rights, advocacy, code issues with sensitivity status, living wills, POAs, etc.
IV 3 Display empathy, compassion and respect to Review customer service guidelines and mission statements patients and families IV 4 Maintain patient privacy and confidentiality at Review confidentiality procedures for medical records, unit all times privacy, HIPPAA, and private places to talk
IV 5 Assist colleagues with care delivery Review teamwork behaviors
IV 6 Incorporate cultural competence and respect Discuss local cultural beliefs and practices that impact for diversity into practice healthcare, interpreter procedures, pastoral care, social services, etc.
IV 7 Provide palliative care as part of the Review guidelines on pain and other symptom management continuum of care. Review education and support systems that help patients live as actively as possible until death Introduce to team and team approach to address needs of patients and families, including bereavement counseling
Section V. The learner will incorporate management skills in all interactions to include the following: V1 Plan shift to accomplish tasks and goals Review unit shift expectations and time management techniques
V2 Manage assignment Review position descriptions and capabilities of other staff on the unit
V3 Manage self Review unit and hospital requirements, lift policies, employee safety process, dress code, etc. Review quality process used in facility
Section VI. The learner will incorporate leadership skills in all interactions to include the following: VI 1 Complete Clinical Nursing Leadership Review policies along with the competence form including Competence staffing, acuities, disaster management, etc.
VI 2 Supervise staff Review position descriptions
VI 3 Delegate work fairly and according to skill Introduce to all unit staff and describe their job responsibilities level and scope of practice and limitations
VI 4 Coordinate care with healthcare team Introduce to all professional and support team members, review their roles & contact procedures
Form based on Dr. Carrie Lenburg’s “Competency Outcomes & Performance Assessment” model. Copyright © May, 2008. Updated May, 2012. Alaska Coalition of Educators—Health Care. All rights reserved. Page 15 LEARNER GUIDE: Reference content in the right-hand column that needs review. VI 5 Initiate chain of command Review organizational structure and situations requiring notification
Section VII. The learner will incorporate teaching skills in delivery of all nursing care to include the following: VII 1 Educate patients and families with Review teaching principles and local culture and resources consideration for age, culture, educational background and home environment or setting VII 2 Provide education to complete a successful Identify community resources for the patient patient discharge per policy Review discharge policy and procedures (pharmacy, standardized teaching materials, etc.)
VII 3 Coordinate education to ensure the patient Review standards for patient education gets a consistent message Section VIII. The learner will incorporate knowledge integration skills to include the following: VIII Identify care issues within the rural Discuss general rural care issues & those specific to each rural 1 environment site Problems common in frontier areas: older population, socioeconomic status, access, transportation and financial issues, employee benefits, fewer practitioners Rural nurse generalist concepts: isolation and distance, lack of anonymity, old timer/newcomer and insider/outsider, informal networks, rural concepts of health, definition of health, possibly delayed treatment seeking, self reliance, cultural issues, boundary expansion and pinch hitting, “practicing medicine” without a license, family centered care, career development and education, accessing patient care information on the fly
VIII Provide nursing care that is evidence based Review computer/library resources, local experts and classes 2 VIII Use all computer systems successfully Obtain computer systems training 3 VIII Accept teaching, coaching and mentoring to 4 improve competence VIII Seek continued learning opportunities to Review resources available for learning 5 improve practice Other facility specific items to cover:
Form based on Dr. Carrie Lenburg’s “Competency Outcomes & Performance Assessment” model. Copyright © May, 2008. Updated May, 2012. Alaska Coalition of Educators—Health Care. All rights reserved. Page 16 REQUIREMENTS: All nurses will complete these competencies upon hire. Some competencies may be reviewed annually. This form follows the Competency Outcomes and Performance Assessment (COPA) model.
PRECEPTEE/LEARNER INSTRUCTIONS: Complete self-assessment: Rate your skill in each area to identify the areas where you need additional experience, access to teaching resources, and/or lab practice. Discuss your results with your preceptor to help establish a plan and goals for your learning experience and to aid in choosing patient assignments. Scoring per instructions at the top of page 1.
PRECEPTOR INSTRUCTIONS: A. Review self-assessment with preceptee/learner to establish plan. B. Required Competencies: The specialty area competency forms are required for independent practice on this unit. This column represents the Alaska Statewide required competencies per ACE-HC and should not be altered. The preceptor will sign each one off when he/she, as preceptor and colleague, feels safe in allowing the preceptee/learner to deliver this aspect of care without direct supervision. C. Verification Method & Agency Specific. Document comments/check marks for the competency and any agency specific requirements. Verification methods include: 1. Demonstration – Preceptor watches learner perform task/procedure in safe, capable manner in a simulated lab or computer setting or as part of direct care performance. The expectation for new graduates is that they demonstrate as many of the competencies as possible. 2. Test – Learner passes a test provided by the facility to measure competence for this skill. (Minimum passing grade indicated. Initial only after test passed.) 3. Module –Learner has completed a training tool (computerized or written module, class, video, etc.) provided by the facility to measure competence for this skill. 4. Verbalization - Learner explains to the preceptor the process and/or planning that evidences safe, reliable knowledge base. This may include case scenarios, discussion, and/or description of plan. NOTE: some competencies may have the verification method specified per facility guidelines (e.g. “test only”) Record N/A and initials only for items that never apply to this learner’s role or performance. D. Sign-off: Sign and date when all elements of the competency are met. If unable to sign off an area due to patient population issues or learner needs more time, document a plan in the comments section at the end of the form. Discuss alternative ways of meeting the requirement(s) as well as any additional time needed with the nurse manager and/or nurse educator. All preceptors assisting in orientation of a new staff member/intern must sign and initial in the signature chart at the end of this document. E. References: Competencies should be met in accordance with these. Add your facility approved references here. F. Learning Guide: These are memory ticklers. The amount of time spent on each of them depends on the learner’s experience. New graduates will likely need time on almost all of the areas listed.
REFERENCES COLUMN: List foundational documents to support the learning experience and to use as the official measure by which the competencies are assessed. The ACE-HC group recognizes the following as sources for evidence based practice that can be included in the reference list along with local policies, procedures and forms: Perry & Potter, Elsevier/Mosby, Lippincott, Kozier & Erb, ANA, nationally recognized hospital related regulatory organizations (CLIA, CDC, CMS, JC, etc.), and specialty nursing organizations’ scope, standards and core curricula. This column’s content may be changed to be facility specific.
NOTE: ACE-HC competency forms are intended to be used between facilities within Alaska.
Form based on Dr. Carrie Lenburg’s “Competency Outcomes & Performance Assessment” model. Copyright © May, 2008. Updated May, 2012. Alaska Coalition of Educators—Health Care. All rights reserved. Page 17 Form based on Dr. Carrie Lenburg’s “Competency Outcomes & Performance Assessment” model. Copyright © May, 2008. Updated May, 2012. Alaska Coalition of Educators—Health Care. All rights reserved. Page 18