Annual Report 2009 - National Antibiotic Committee (NAC).
The NAC officially met 5 times during 2009. Four of these meetings were minuted (see Annex 1) whilst the fifth meeting was a meeting with the European Centre for Disease Prevention and Control (ECDC) visit during the week 23rd-27th November 2009. The latter meeting was minuted by the ECDC delegation. There were also various meetings with representatives of the Malta college of General Practice whilst organizing their Autumn 2009 Continuing Medical Education (CME) credits. The CME was held during the (ECDC) week visit.
In addition the Chair and secretary attended a conference in Prague in April during the Czech EU presidency. The chair and an Infection Control Nurse (not a member of the NAC) attended the follow-up meeting in London in October during the Swedish EU presidency.
Furthermore, the 2nd European Antibiotic Awareness Day was also celebrated with a very limited budget, which was decreased from €7000 in 2008 to €3000 in 2009. The 18th November of every year will become the World Antibiotic Awareness Day (no longer just European) as of 2010.
The major issue encountered during our meetings was the lack of a representative of the Community-Pharmacists, since Ms Vanessa Bugeja the nominated representative was never present at any of the meetings. It is recommended that another representative be selected.
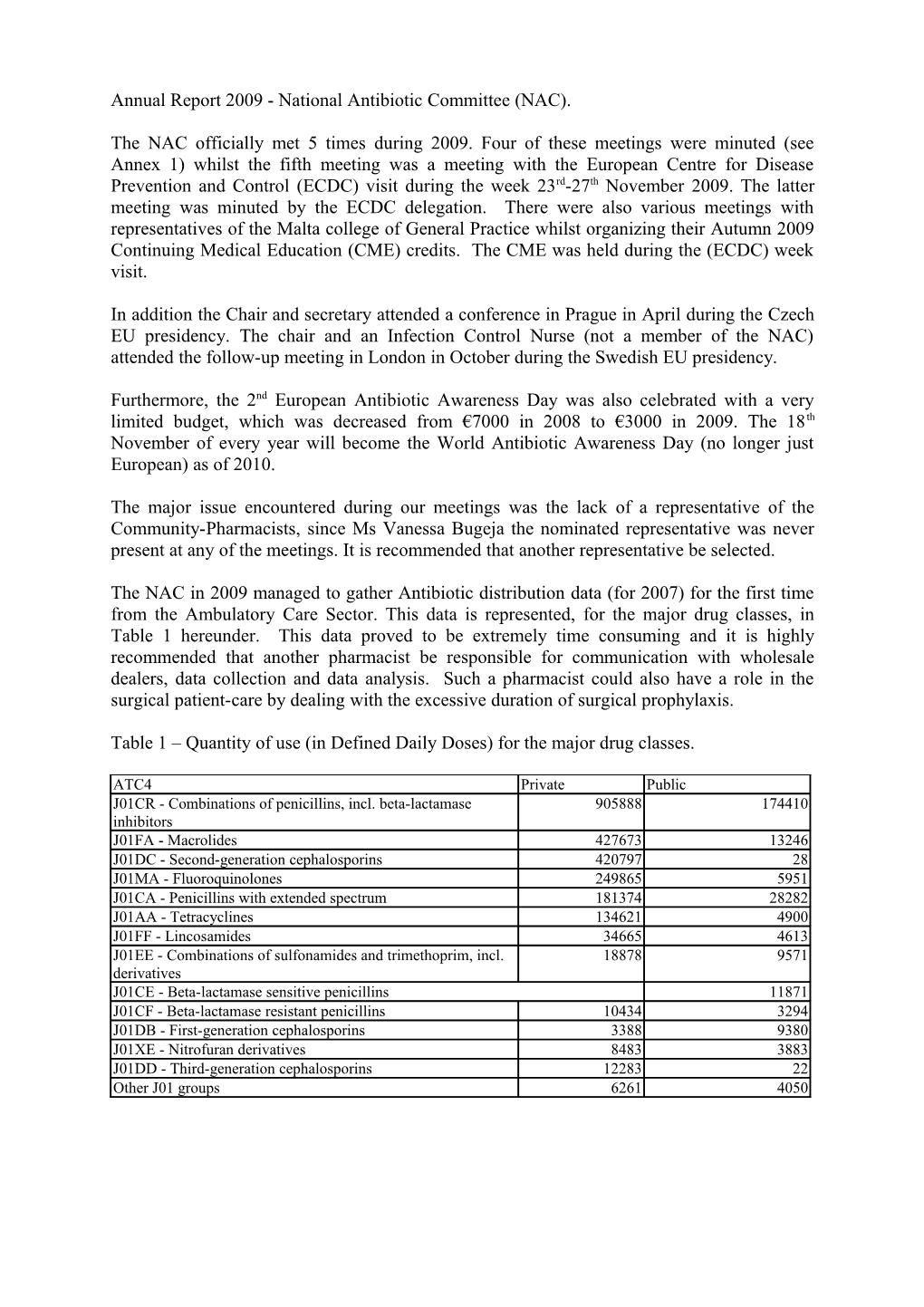
The NAC in 2009 managed to gather Antibiotic distribution data (for 2007) for the first time from the Ambulatory Care Sector. This data is represented, for the major drug classes, in Table 1 hereunder. This data proved to be extremely time consuming and it is highly recommended that another pharmacist be responsible for communication with wholesale dealers, data collection and data analysis. Such a pharmacist could also have a role in the surgical patient-care by dealing with the excessive duration of surgical prophylaxis.
Table 1 – Quantity of use (in Defined Daily Doses) for the major drug classes.
ATC4 Private Public J01CR - Combinations of penicillins, incl. beta-lactamase 905888 174410 inhibitors J01FA - Macrolides 427673 13246 J01DC - Second-generation cephalosporins 420797 28 J01MA - Fluoroquinolones 249865 5951 J01CA - Penicillins with extended spectrum 181374 28282 J01AA - Tetracyclines 134621 4900 J01FF - Lincosamides 34665 4613 J01EE - Combinations of sulfonamides and trimethoprim, incl. 18878 9571 derivatives J01CE - Beta-lactamase sensitive penicillins 11871 J01CF - Beta-lactamase resistant penicillins 10434 3294 J01DB - First-generation cephalosporins 3388 9380 J01XE - Nitrofuran derivatives 8483 3883 J01DD - Third-generation cephalosporins 12283 22 Other J01 groups 6261 4050 Annex 1 – Minutes of Meetings
Minutes of the meeting held on Wednesday 28th January 2009.
Members - Present Dr MA Borg – Chair [MAB] Dr AP Azzopardi [APA] Prof P Cuschieri [PC] Dr Tanya Melillo [TM]
Members - Excused Dr Susan Chircop [SC] Ms Vanessa Bugeja [VB] Dr T Piscopo [TP]
Secretary Mr P Zarb [PZ]
1. Minutes of last meeting held in 2008 were agreed upon. 2. The 2008 campaign seemed to had an impact and therefore, we must repeat the campaign in 2009 with a better budget in order to be able to buy some television airtime which is the most effective form of advertising. [MAB] a. The possibility of reinforcing the campaign now was recommended by APA. b. Leaflets are to be sent to Valletta information centre. 3. The 2009 campaign on doctors should emphasise on ‘Delayed Prescriptions’. a. The NAC should issue specific prescription pads for delayed prescriptions, possibly in self carbon copied format so that the copies could be sent back in order for renewal booklets to be issued. b. Guidelines for Respiratory Tract Infections for GP’s should be issued. PZ mentioned the work done by an undergraduate Pharmacy student. c. These Guidelines are to be issued in conjunction with the MCGP. 4. The Campaign for Pharmacists should concentrate on topical treatment and something should be organised in conjunction with the MCPP. 5. The issue of sensitivity testing for community treated infections was raised by APA. It was agreed to recommend that any GP (in the private sector) should be able to communicate with a Microbiologist in the Department and get their respective endorsement for difficult cases to be tested by MDH laboratory of Microbiology. 6. The members were informed that we are currently working on obtaining a list of all anti-infective agents licensed in Malta in order to start collecting consumption data from the community. It was stressed out that wholesale dealers are to supply data divided by each product and such data should be then divided into; private sector – community; private- hospitals; Government Health Services. 7. The meeting was adjourned for the 30th April 2009. Minutes of the meeting held on Thursday 28th May 2009.
Members - Present Dr AP Azzopardi [APA] Dr MA Borg – Chair [MAB] Dr Susan Chircop [SC] Prof P Cuschieri [PC]
Members - Excused Dr Tanya Melillo [TM] Dr T Piscopo [TP]
Invited Dr Mario Grixti [MG] Malta College of General Practitioners (MCGP)
Absent Ms Vanessa Bugeja [VB]
Secretary Mr P Zarb [PZ]
8. Minutes of last meeting held on 28th January 2009 were agreed upon. 9. Dr Mario Grixti was specifically invited for today’s meeting in order to discuss the possibility of co-organising a CME event with the MCGP. 10. MAB and PZ gave a short summary report on the meeting for the National Focal Points (NFP) for Antimicrobial Resistance and Consumption (AMR) held in Prague in April 2009 during the Czech EU Presidency. 11. MAB informed the members that the ECDC shall be organising a ‘Country Visit’ to Malta, after invitation by the DG Public Health. They shall be auditing: the antimicrobial use and resistance; surveillance of Health Care Associated Infections (HCAIs) and also Animal Health. The visit should be around 1 working wee (5 days) a. Day 1 – Meeting with major stakeholders (including NAC) b. Day 2/3 – Technical day surveying what is being done and/or planned at laboratory level and surveillance. c. Day 4 – Animal husbandry d. Day 5 – Résumé on the visit with suggestions and recommendations for implementation until the follow up visit. 12. Following 2008’s first European Antibiotic Awareness Day (EAAD), we are still awaiting analysis from the Medical Students of the data they gathered from their survey. However, according to MAB, it transpires that the most effective medium is the audio-visual (TV), where 70% of the people who were aware of EAAD. a. This trend on effectiveness of TV adverts was also observed by ECDC and their marketing consultants. In fact the ECDC prepared two options for a TV advert, which were explained during the AMR-NFP meeting in Prague. b. These two options are quite different: i. One is based on last year’s hedgehog that comes home from work and gets better without antibiotics. This links the 2009 campaign to the 2008 campaign. ii. The other option is very abstract and metaphorical comparing a light bulb being left on during a bright day and then it does not switch on at night when needed, which is what happens when antibiotics are used unnecessarily. This option is preferred by MAB. PZ and APA showed concern about the advert being misunderstood as ‘save energy’ especially keeping in mind the issue of raised electricity costs. iii. A third option would be to come up with a Maltese advert, but this is highly unlikely since the cost of production would probably leave no budget for buying any airtime. 13. For the 2009 EAAD, it is being proposed that a CME event spread over 3 days (starting on the EAAD, i.e., Wednesday 18th November 2009) is organised by the MCGP for 3 consecutive evenings, entitled ‘Update on antimicrobial therapy in Family Practice’. The three provisional topics recommended are: a. Day 1 – A general introduction including consumption data from the community from 2007 b. Day 2 - Focus on Respiratory with an intervention from a Respiratory Physician and a Microbiologist/ID Physician. c. Day 3 – Focus on Dermatology with an intervention from a Dermatologist and a Microbiologist/ID Physician. d. It would be interesting if resistance data is collected from private laboratories (in a similar manner that antimicrobial data started being collected as of this year backdated as of 2007). Such data could be presented at the MCGP CME. 14. The MMSA students should be once again encouraged to carry out a similar event like the one of last year. 15. Furthermore, this year an EU funded British project called e-BUG is available for Schools. MAB has already communicated with Mr Philip Bonello (Education Officer Health and Safety) to this effect. 16. MAB is to contact a respiratory physician and paediatric infectious disease physician to draft ‘Treatment of Respiratory Infections’. These guidleines shall include drug classes ib the recommendations and not specific molecules. However, a drug list with comments (formulary status, cautions etc.) shall be made available as an Appendix. 17. It is also being recommended that some form of guidelines be issued for Veterinarians. This is in response to the comment raised by SC who showed documents from EU Food Safety Agency whereby they are also considering antibiotic use in pets, in addition to that in animal husbandry, as a potential threat to resistance due to the close proximity of pets with their owners. 18. The meeting was adjourned for the 2009.
Minutes of the meeting held on Thursday 28th August 2009.
Members - Present Dr AP Azzopardi [APA] Dr MA Borg – Chair [MAB] Dr T Piscopo [TP] Prof P Cuschieri [PC]
Members - Excused Dr Tanya Melillo [TM] Dr Susan Chircop [SC] Absent Ms Vanessa Bugeja [VB]
Secretary Mr P Zarb [PZ]
19. Minutes of last meeting held on 28th May 2009 were agreed upon. 20. APA to contact Dr Mario Grixti re the MCGP Autumn CME which is to be held on the 25th and 27th November by the MCGP. 21. The ECDC country visit (between 23rd and 27th November, 2009) shall include a meeting with the NAC and MCGP/ APFD for a business lunch. 22. The AMR dates were already booked by two separate companies on the respective dates so there will be other activities running concurrently on both days. This will result in a slight decrease in turn-out. 23. For the second European Antibiotic Awareness Day (EAAD), the budget is only € 3000, which is less than half of last year’s allocated budget. a. The NAC shall repeat the use of 2 non-commercial posters throughout the month of November which shall take most of the limited budget. b. The remaining balance shall be used for airing a TV spot prepared by the ECDC on the EAAD before the 20.00hours news on TVM and possibly other channels but this is highly unlikely due to the low budget. i. The two options for the TV spot were discussed and it was agreed that the ‘hedgehog’ theme as opposed to the ‘light-bulb’ theme would be used both for continuity and also for message clarity. The possibility of dubbing the message in Maltese is to be explored. However, it may not worth the expense for if the advert is to be aired once only. 24. MAB and PZ met with the H&S Education Officers who agreed on utilising the E- BUG tools. 25. MAB to contact the EO again in order to reconfirm the use of E-Bug by the Education Department. 26. MAB is to issue a circular on the use of clarithromycin only when there is radiological evidence of pneumonia. 27. PZ confirmed that the great majority of WSL responded with the 2007 data and only a handful of WSL are missing their data submission. 28. The meeting was adjourned for the 22nd October 2009. Minutes of the meeting held on Thursday 22nd October 2009.
Members - Present Dr AP Azzopardi [APA] Dr MA Borg – Chair [MAB] Prof P Cuschieri [PC] Dr Tanya Melillo [TM] Dr Susan Chircop [SC]
Absent Ms Vanessa Bugeja [VB] Dr T Piscopo [TP]
Secretary Mr P Zarb [PZ]
29. Minutes of last meeting held on 28th August 2009 were postponed for the next meeting. 30. The first item on the Agenda was the 2nd European Antibiotic Awareness Day (EAAD). a. The ‘hedgehog advert’ (from now on referred to as the ‘spot’) by ECDC translated to Maltese, shall be aired on TVM on the EAAD (18th November) just before the evening news at eight. b. With the remaining budget, the spot can be aired at least twice more again during the Influenza Season (probably January-February 2010). c. TM is to check with Dr Charmaine Gauci, whether there is any ongoing agreement of ‘off-peak’ airtime with any programme/station where the EAAD spot could be aired, ideally on the Monday 16th and/or Tuesday 17th November before the actual EAAD. The possibility of airing the spot also during the off-peak on the day and the rest of the week is also to be sought. d. On the 17th November, Dr Joe Cassar (Parliamentary Secretary) will give a Press Conference about the 2nd EAAD. e. The ECDC has just launched a Primary Care toolkit for Respiratory Infections. < http://ecdc.europa.eu/en/EAAD/antibiotics/Pages/messagesForPrescribers.asp x> MAB is to contact: ‘TheSynapse’ editor Dr Wilfred Galea; Association of Private Family Doctors (APFD), College of General Practitioners (MCGP); Association of Doctors working in Health Centres and APA. 31. The 2nd item on the agenda was the ECDC AMR visit between the 23rd till the 27th November. a. On Monday 23rd between 14.00 and 16.00 the ECDC delegation shall be meeting with the members of the NAC at Mater Dei Hospital. All members are expected to be present. b. The preliminary programme as on the 15/10/2009 was discussed. Any amendements agreed upon are listed hereunder. c. Tuesday evening session with the Veterinarians is to be held at 20.00 for 20.30 hours. The venue has been agreed as the Professional Associations Centre - Gzira. MAB is to organise refreshments. SC will try and organise a small survey with colleague Veterinarians about which antibiotics are used for small animals (pets) as opposed to animal husbandry. d. Wednesday evening session with the Primary Care physicians is to be held at 20.00 for 20.30 hours. The representatives of the respective associations (see eabove) will meet the ECDC team before the event. The speakers at the event will be Michael Borg and Dominique Monnet from the ECDC. The data from antibiotic consumption surveillance will be presented as well as an overview of ECDC tools for Primary Care. Annex II – Report on NFP AMR Meeting in Prague
Report of the [6th Meeting of National AMR Focal Points & CZ PRES Ministerial Conference "The Microbial Threat to Patient Safety in Europe", 14-16 April, Prague] Purpose of the Meeting: Sharing ideas and experiences on the roles of government, public health authorities, hospital management, healthcare payers, surveillance programmes and hospital accreditation programmes in reducing antimicrobial resistance and healthcare- associated infections Participant/s: Dr Ray Busuttil; Dr Michael Borg, Mr Peter Zarb. Report drawn up by: Mr Peter Zarb Time: Meeting commenced at 1200hrs on the 14th and ended at 1300hrs on the 16th Abbreviations used: AT - Austria; BE - Belgium; CZ - Czech Republic; CY - Cyprus; DK - Denmark; EE - Estonia; FI - Finland; FR - France; DE - Germany; EL - Greece; IE - Ireland; HU - Hungary; IT - Italy; LV - Latvia; LT - Lithuania; LU - Luxembourg; MT - Malta; NL - Netherlands; PL - Poland; PT - Portugal; ES - Spain; SI - Slovenia; SK - Slovakia; SE - Sweden; UK - United Kingdom; CION - Commission. AMR –Antimicrobial Resistance, HCAI – HealthCare Associated Infections.
Introduction The meeting involved 2 round table workshops dealing with the National Systems for AMR and control of HCAIs.
1 Agenda In black: input from National AMR Focal Points
In blue: extracted from reports of Chief Medical Officers at their meeting in Prague, 16 March 2009 MALTA
• Role of Government – Major role (especially since >90% HC is publicly funded) – Sets targets and goals – Funds both AMT initiatives as well HCAI prevention programmes
• Role of Public Health Authorities – Enactment of legislation (AMR) – Legal backing to surveillance & data collection requests – Strong participation in committees & working groups – Effective collaboration
• Role of hospital management (national level) – Establishment of relevant infrastructure – Sustain infection control & antibiotic teams / committees – Support audit and accountability
• Role of healthcare payers – Minimal input of healthcare payers since private hospitals constitute <5% of hospital beds & the role of insurance companies is only related to such entities.
• Support of surveillance programmes – Surveillance programmes (e.g., EARSS & ESAC) have sensitised both decision makers as well as public opinion on AMR issues – HCAI incidence surveillance - benchmarking – Process surveillance (esp. hand hygiene compliance)
• Role of hospital accreditation programmes – No current hospital accreditation programmes in place
Key issues for Health and Healthcare in your country over next 3-5 years Key issues for the future in relation to antimicrobial resistance and healthcare associated infections are: – Establishing the new regulatory framework – Changing the culture so that infection prevention and control is embedded in practice, education and training. – Reducing variations in performance between NHS bodies – Increasing PCT capability in commissioning and monitoring services in relation to their performance on healthcare associated infections – Ensuring that reductions in infections are sustainable, without the need for continuing intensive intervention – Improving surveillance information so that interventions can be targeted appropriately. – Influencing curricula to ensure good education of prescribers of antimicrobials
The following is a draft document which was presented by the Czech presidency. However, it needs to be resubmitted at a later stage with major amendements. Ministerial conference “The Microbial Threat to Patient Safety in Europe” Prague, Czech Republic, April 15 – 16 2009 Hospital antibiotic stewardship programme (H-ABS-Programme) Introduction Systematic prevention and control of antimicrobial resistance is necessary to maintain long- lasting effectiveness of antimicrobial agents for treatment and prophylaxis of infections. Loss of their clinical effectiveness represents a significant threat for patients affected by serious, life threatening infections in the hospital setting. Effective prevention and control of antimicrobial resistance in hospitals is based on complementarily implemented activities focused on decrease in selective pressure of antimicrobials associated with their inappropriate use as well as reduction of spread and transmission of resistant micro-organisms. These principles are generally declared in the Council Recommendation on Prudent Use of Antimicrobial Agents in Human Medicine, as well as in the recently proposed Council Recommendation on Patient Safety incl. Prevention and Control of Healthcare Associated Infections. Whereas standards and measurable elements focusing on prevention and control of infections in healthcare institutions already exist (e.g. JCI accreditation standards, IPSE standards and indicators), similar standards are not yet available for implementation of hospital antibiotic stewardship. Recent EU projects (e.g. ABS International), have defined principles of hospital antibiotic stewardship which can form the basis of discussions on appropriate standards and measurable elements to improve practices in healthcare institutions across Europe. These standards could be included as accountability criteria for hospital accreditation. Objectives • Ensuring effective, safe and cost effective antibiotic treatment and prophylaxis of infections as an integral part of care for patients in the hospital setting. • Prevention and control of antimicrobial resistance by means of prudent use of antibiotics in order to maintain their long-term effectiveness for treatment and prophylaxis. • Reduction of occurrence of difficult-to-treat infections caused by multi-drug resistant micro-organisms, threatening quality of care and the safety of hospitalised patients.
Principles • Establishing an interdisciplinary hospital antibiotic stewardship programme focused on the optimisation of quality of antibiotic usage and control of antimicrobial resistance at the hospital level. • Creating an organizational structure to lead hospital antibiotic stewardship programme, specification of its scope, functions, activities, competencies, leadership and accountability, incl. indispensable support of hospital management. • Ensuring sufficient capacity of the hospital antibiotic stewardship programme in terms of human, material and technical resources. • Creating and implementing basic tools for hospital antibiotic stewardship (e.g. an antibiotic list with specification of restricted drugs, control of antibiotic consumption, local surveillance of antimicrobial resistance, local guides for diagnostics of infections incl. clinical microbiology, local guides for initial and pathogen specific therapy, for surgical prophylaxis, consulting and supervising of antibiotic usage, etc.). • Performing epidemiological surveillance of antimicrobial resistance as required for optimisation of antibiotic treatment and prophylaxis at the local level (e.g. local rates and trends of antimicrobial resistance, outputs of local surveillance of healthcare associated infections, regional and national epidemiological patterns of community acquired infections incl. levels of antimicrobial resistance of key pathogens). • Systematic evaluation of quality of antibiotic usage in the hospital setting, based on relevant scientific knowledge, focused on identification of inappropriate practice. Continuous improvement of quality of antibiotic usage using relevant, validated, feasible and cost effective quality indicators and quality management procedures. • Effective co-ordination of the hospital Antibiotic stewardship programme with the Programme on prevention and control of infections focused on the control of spreading of resistant pathogens. • Continuous quality improvement of the hospital antibiotic stewardship programme, regarding capacity building, structure, organization, functions and effectiveness, based on implementation of action plans reflecting evaluation of adequate structure indicators and level of implementation of specific standards.
Proposal of standards and measurable elements of hospital antibiotic stewardship programme (H-ABS-Programme) 1. Establishment and objectives A healthcare institution establishes a specific, interdisciplinary programme, focused on high quality of antibiotic usage, aiming at long-lasting sustainability of effectiveness of antimicrobial agents for treatment and prophylaxis, at reduction of risk of antimicrobial resistance as well as difficult-to-treat infections due to multi-drug resistant pathogens threatening patient safety. 2. Scope and priorities The scope of H-ABS-Programme takes into account the clinical spectrum and epidemiological characteristics of community-acquired and healthcare associated infections, which occur in patients, to whom the healthcare institution provides care. Priorities of H- ABS-programme are appropriate in relation to the structure, scope and characteristics of provided healthcare (such as a spectrum of clinical disciplines, characteristics of patient populations, proportion of ICU beds, etc.). 3. Conditions for effective operation 3.1. Management of the healthcare institution is responsible for ensuring sufficient resources (in particular human, financial and technical) and support of H-ABS-Programme. 3.2. The healthcare institution supports the personal development of professionals in the interdisciplinary antibiotic management team. 3.3. The healthcare institution disposes of sufficient capacity regarding diagnostics and clinical management of infections, appropriate to the scope and characteristics of provided healthcare. 3.4. The healthcare institution has sufficient capacity of clinical microbiology services with an optimal spectrum of examinations allowing pathogen-specific therapy and providing necessary and interpretable data for optimizing initial antimicrobial therapy, prophylaxis, and also effective prevention and control of antimicrobial resistance. 3.5. The healthcare institution has access to the required data on the antimicrobial resistance for optimisation of antibiotic use and effective prevention and control of antimicrobial resistance. 3.6. Inappropriate influence of marketing and promotion of pharmaceutical industry on operation and activities of H-ABS-Programme must be avoided. Relationships between H- ABS-Programme and the pharmaceutical industry must be regulated by national legislation, ethical rules of professional societies and bodies, and local rules established by the healthcare institution.
4. Structure, organization, personnel and management 4.1. H-ABS-Programme is co-ordinated by an interdisciplinary antibiotic management team (AMT), whose composition, roles, responsibilities and leadership are defined, recognized and supported by the hospital management. 4.2. AMT is composed of experienced specialists with relevant education, training and authority, representing appropriate disciplines related to the scope of hospital antibiotic stewardship and prevention and control of antimicrobial resistance (e.g. clinical microbiology, infectious diseases, intensive care, surgery, hospital pharmacy, infection control, other clinical disciplines as appropriate, etc.). 4.3. AMT is responsible for ensuring, co-ordinating and managing of all functions and activities of H-ABS-Programme (reference to 5). 4.4. Sufficient numbers of clinical consultants with appropriate education and training are available to provide their services for clinical wards regarding support of prudent use of antimicrobial agents for individual patients (reference to 5.4). 4.5. H-ABS linked physicians effectively co-operating with AMT are established on clinical wards, to ensure all appropriate functions and activities of H-ABS-Programme at this level. 4.6. Supporting staff is available for optimal operation and ensuring functions of H-ABS- Programme as appropriate and necessary (e.g. data documentation assistants, IT specialists, epidemiologists and biostatisticians, possibly also project managers, communication and public relations specialists, etc.). 5. Functions and activities 5.1. Local surveillance of antimicrobial resistance Competent professionals regularly process, evaluate, compare and interpret local data regarding clinically and epidemiologically important patterns of antimicrobial resistance, to be adequately useful for updating local guides for initial antimicrobial therapy, for effective control of spread of resistant micro-organisms, as well as restriction of particular groups of antimicrobials with potential risk for selection of resistance. Intelligible and easy to implement outputs of this activity are routinely disseminated to all concerned personnel as appropriate. 5.2. Local surveillance of antibiotic consumption Competent professionals regularly process, evaluate, compare and interpret local data regarding consumption of antimicrobials to detect its important quantitative and qualitative changes as soon as possible, when a detailed analysis of reasons of observed trends is needed for early implementation of appropriate control measures. Intelligible and easy to implement outputs of this activity are routinely disseminated to all concerned personnel as appropriate.
5.3. Categorisation of antimicrobial agents and creating antibiotic lists The healthcare institution through AMT defines and regularly updates a generic list of essential antimicrobial agents according to the scope and characteristics of provided care, as well as spectrum and epidemiological characteristics of occurred infections. Categorisation of restricted drugs under supervision of AMT incl. description of specific rules for its use and prescribing is integrated. Appropriate additional information can be included, such as pricing, dosage, etc. This list (antibiotic list) is widely available for all prescribing physicians, the hospital pharmacy and other relevant healthcare workers. 5.4. Development and regular updating of local guides for diagnostics, treatment and prophylaxis of infections Interdisciplinary AMT develops and regularly updates local guides for diagnostics, treatment and prophylaxis of infections in co-operation with clinical and diagnostic hospital departments. These guides have to correspond to the scientific knowledge, relevant international and national guidelines, have to take into account adequate national, regional and local epidemiological characteristics and have to be well understandable and available. 5.5. Clinical consulting and services focusing on support of prudent use of antimicrobial agents Services on clinical consulting of individual patients for differential diagnosis, treatment and prophylaxis of infections are an integral part of H-ABS Programme. These activities also cover supervision of usage of restricted drugs and interpretation and active reporting of critical results of microbiology examinations aimed at early conversion from initial to pathogen specific therapy, where possible. Consultations must be widely available and routinely documented at patient records to ensure continuity of care. 5.6. Systematic measuring, evaluation and improving quality of antibiotic usage H-ABS-Programme implements activities focused on systematic improvement of quality of antibiotic usage in the interest of optimisation of treatment and prophylaxis of infections. Adequate procedures and measures are used, which are of scientific relevance, validated, feasible, cost effective, and ideally resulting from measurement of relevant quality indicators. 5.7. Education and training The healthcare institution ensures through AMT regular training of prescribing physicians and other relevant healthcare workers in diagnostics, treatment and prophylaxis of infections, focusing on appropriate use of antimicrobial agents as well as prevention and control of antimicrobial resistance. Training activities cover information on recent problems of antimicrobial resistance, inappropriate use of antimicrobials and adequate control measures for improvement. AMT members and clinical consultants take part in systematic continuing education and training in all areas needed for their professional skills.
6. Tools Specific tools are developed and available at all appropriate levels to ensure optimal operation of H-ABS programme. These tools are complementary to its functions (reference to 5) and cover particularly: • Antibiotic lists • Local guides for diagnostics of infections including microbiology laboratory • Local guides for initial antimicrobial therapy • Local guides for pathogen-specific antimicrobial therapy • Local guides for surgical prophylaxis • Tools for controlling of antibiotic consumption • Tools for controlling of antimicrobial resistance 7. Integration of H-ABS-Programme to the hospital programme on quality and safety, links and relationships 7.1. Continuous quality improvement of the hospital antibiotic stewardship programme is regularly evaluated using appropriate methods (measuring structure indicators, auditing implementation of H-ABS standards). Outputs of this evaluation are used for further development through realization of H-ABS action plans with appropriate timing. 7.2. H-ABS-Programme is linked to the programme on prevention and control of infections of the healthcare institution and their effective co-operation is running on daily basis. Representatives of both programmes are reciprocally involved in their organizational structures. 7.3. H-ABS-Programme activities are linked and integrated to the hospital drug policy, especially in terms of rational and cost effective use of medicines, reduction of medication errors, undesirable adverse reactions and drug interactions. Representative of H-ABS- Programme is a member of organizational structures responsible for agenda of hospital drug policy (such as hospital drug and therapeutic committee). 7.4. Relationships of H-ABS-Programme with co-operating healthcare facilities and subjects (e.g. general practitioners, ambulatory specialists, hospitals) are covered and co- ordinated. 7.5. H-ABS-Programme of healthcare institution is linked to the national inter-sectoral co- ordination mechanism as appropriate, including involvement to the international co-operation in the field of antibiotic usage and antimicrobial resistance (e.g. ECDC agenda).
Issues to be followed up by Malta Surveillance of antimicrobial consumption, outside the hospital setting, both in the private and public sector.
Date of Next Meeting London, UK, 19-21st October 2009.