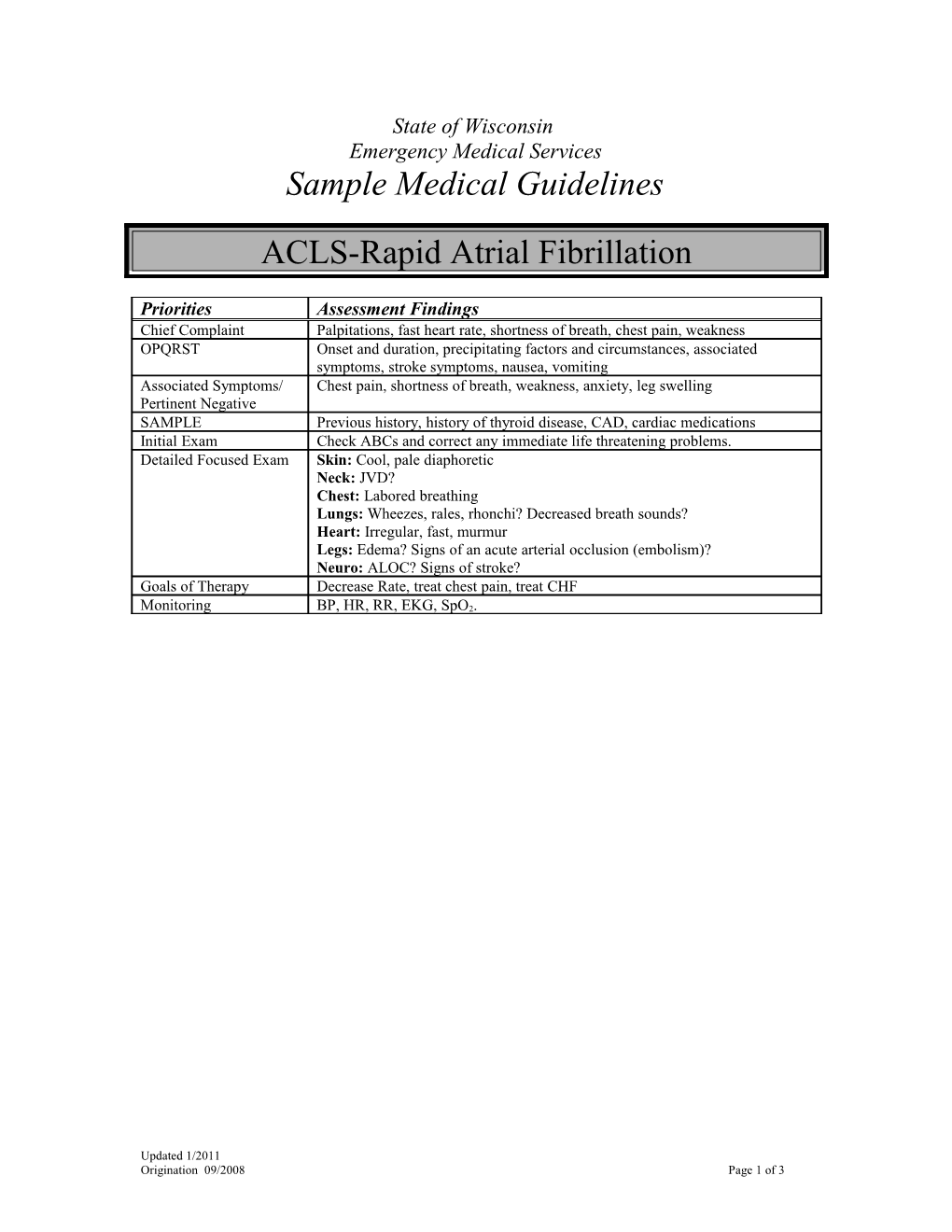
State of Wisconsin Emergency Medical Services Sample Medical Guidelines
ACLS-Rapid Atrial Fibrillation
Priorities Assessment Findings Chief Complaint Palpitations, fast heart rate, shortness of breath, chest pain, weakness OPQRST Onset and duration, precipitating factors and circumstances, associated symptoms, stroke symptoms, nausea, vomiting Associated Symptoms/ Chest pain, shortness of breath, weakness, anxiety, leg swelling Pertinent Negative SAMPLE Previous history, history of thyroid disease, CAD, cardiac medications Initial Exam Check ABCs and correct any immediate life threatening problems. Detailed Focused Exam Skin: Cool, pale diaphoretic Neck: JVD? Chest: Labored breathing Lungs: Wheezes, rales, rhonchi? Decreased breath sounds? Heart: Irregular, fast, murmur Legs: Edema? Signs of an acute arterial occlusion (embolism)? Neuro: ALOC? Signs of stroke? Goals of Therapy Decrease Rate, treat chest pain, treat CHF
Monitoring BP, HR, RR, EKG, SpO2.
Updated 1/2011 Origination 09/2008 Page 1 of 3 EMERGENCY MEDICAL RESPONDER (EMR) Routine Medical Care Titrate oxygen therapy to the lowest level required to maintain an oxygen saturation greater than 93% If the patient is having difficulty breathing allow them to sit in position of comfort
EMERGENCY MEDICAL TECHNICIAN (EMT) If the patient experiences shortness of breath, follow the Congestive Heart Failure Guidelines If the patient has suffered a stroke, follow the Stroke Guidelines. ECG monitor or 12 lead acquisition, if approved.
ADVANCED EMT (AEMT) IV/IO NS @ TKO, if approved. If SPB < 100 mmHg give 500cc fluid bolus, and then reassess o Consider Trendelenberg position, if there is no dyspnea
Contact Medical Control for the following: Additional fluid orders
INTERMEDIATE Obtain a 12-Lead EKG if not already performed If the patient does not have a history of atrial fibrillation, consider the potential causes that may have a bearing on prehospital care, including: o Acute coronary syndromes (e.g. AMI) o Pulmonary embolism o Alcohol use o Stimulant drug abuse (e.g. cocaine and amphetamines) If the patient has a history of atrial fibrillation, consider possible causes of tachycardia, including pain, dehydration, hypotension, shock, hypoglycemia, hypoxemia, anxiety, fever, sepsis, drug induced, recent heavy exertion, hyperthyroidism and anemia. If the patient is hemodynamically and clinically stable, observe and monitor.
Contact Medical Control for the following: If the patient is unstable, consider cardioversion under direction of Medical Control.
PARAMEDIC If the patient is hemodynamically and clinically stable, transport, observe and monitor. Efforts to reduce the heart rate will add little benefit in the absence of adverse effects from RAF. If the patient is hemodynamically or clinically unstable o Prepare to perform synchronized cardioversion, consider pain management or sedation o Perform first synchronized cardioversion @ 120-200 J biphasic (200 J monophasic) o If synchronization is unsuccessful, turn sync off and attempt cardioversion
Contact Medical Control for the following: Additional orders to potentially include Cardizem.
FOOTNOTES: Criteria for characterizing a patient as “unstable” Hemodynamic Criteria o SBP < 80 mmHg AND Heart Rate > 150 beats/min
Updated 1/2011 Origination 09/2008 Page 2 of 3 Clinical Criteria o Signs of shock (poor perfusion) are present, including . ALOC . Absent radial pulses . Pallor and diaphoresis o Signs of pulmonary edema are present, including . Labored breathing . Rales (wet lungs)
. Hypoxia (SpO2 <90%) o The patient complains of angina
Updated 1/2011 Origination 09/2008 Page 3 of 3