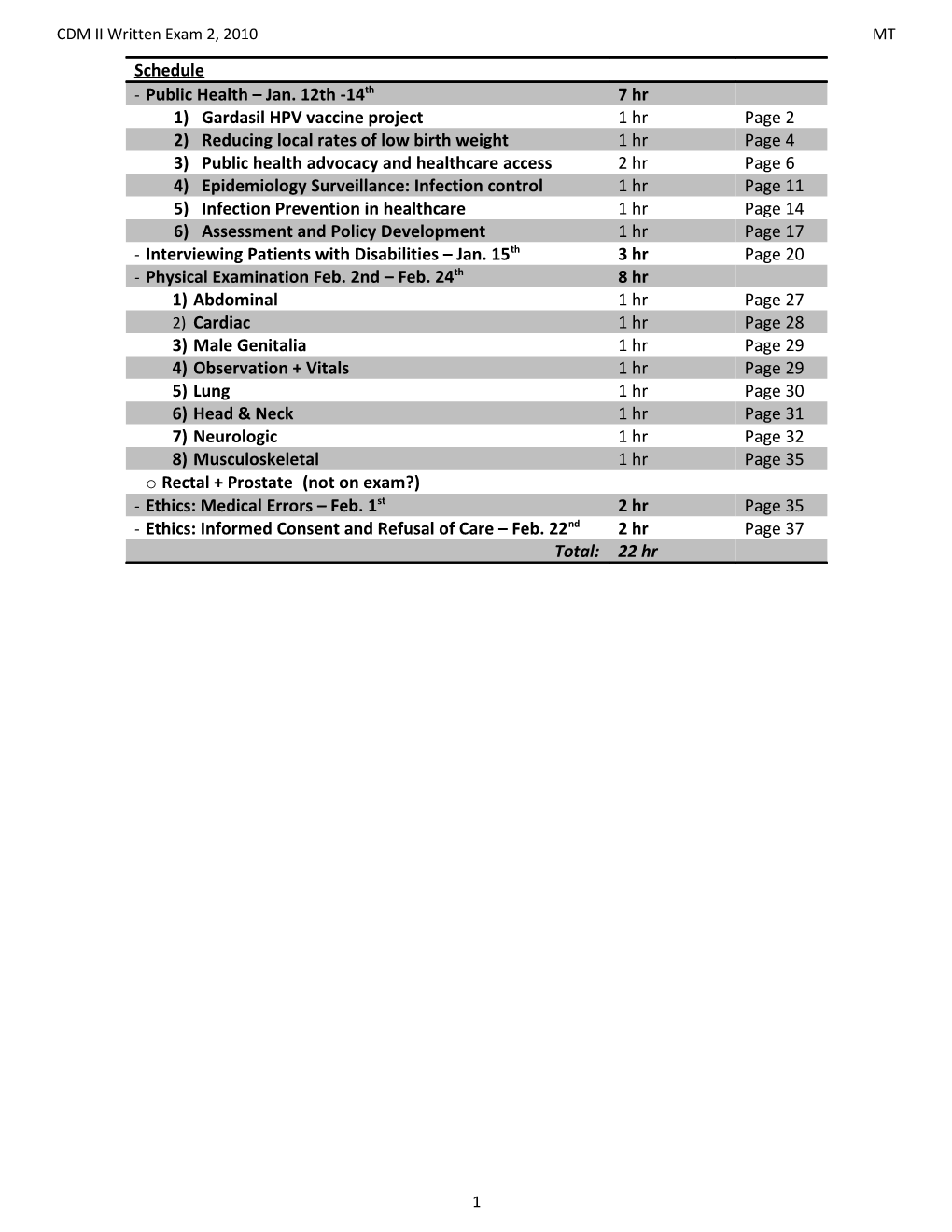
CDM II Written Exam 2, 2010 MT Schedule - Public Health – Jan. 12th -14th 7 hr 1) Gardasil HPV vaccine project 1 hr Page 2 2) Reducing local rates of low birth weight 1 hr Page 4 3) Public health advocacy and healthcare access 2 hr Page 6 4) Epidemiology Surveillance: Infection control 1 hr Page 11 5) Infection Prevention in healthcare 1 hr Page 14 6) Assessment and Policy Development 1 hr Page 17 - Interviewing Patients with Disabilities – Jan. 15th 3 hr Page 20 - Physical Examination Feb. 2nd – Feb. 24th 8 hr 1) Abdominal 1 hr Page 27 2) Cardiac 1 hr Page 28 3) Male Genitalia 1 hr Page 29 4) Observation + Vitals 1 hr Page 29 5) Lung 1 hr Page 30 6) Head & Neck 1 hr Page 31 7) Neurologic 1 hr Page 32 8) Musculoskeletal 1 hr Page 35 o Rectal + Prostate (not on exam?) - Ethics: Medical Errors – Feb. 1st 2 hr Page 35 - Ethics: Informed Consent and Refusal of Care – Feb. 22nd 2 hr Page 37 Total: 22 hr
1 CDM II Written Exam 2, 2010 MT Public Health 1: Gardasil Project 1) Understand the pathophysiology of HPV 6) Apply the principles of affordability, accessibility, 2) Recognize consequences of HPV infection and acceptability 3) Define the indications for HPV vaccination 7) Identify available resources for HPV vaccination 4) Identify the target population for HPV vaccination 8) Highlight controversial issues related to HPV 5) List barriers and facilitators to HPV vaccination vaccination - Human Papilloma Virus o Recurrence post treatment: 30-70% w/in 6 mo. o HPV is the single most common STI! - Cervical Cancer9 o By the age of 5o, it is estimated that 75-80% of o In the United States: women will have been infected with HPV. . Incidence: 11,150 new cases/year - HPV Structure: . Mortality: 3670 deaths/year o Non-enveloped . Mean age at diagnosis: 47 years o 8 kb circular DNA genome o Worldwide, cervical carcinoma is the second most o 2 structural proteins: L1, L2 common female malignancy. o Oncogenes: E6, E7 . Prevalent where screening methods are - Serotypes: >100 uncommon o Type 16: 50% of cervical CA - HPV-related Disease o Type 18: 20% of cervical CA o 10 year timeline o Types 6,11: 90% of genital warts - Progression of Cervical Changes o Type 16 + 16: 8% prevalence o Normal, low-grade CIN, high grade CIN, cancer - Life Cycle - Quadrivalent HPV Vaccine (Gardasil) o Initial infection of basal cell o Recombinant L1 Capsid Protein o Specific gene products transcribed at every level of . Empty capsids (no DNA, no oncogenicity) keratinocyte differentiation . Given in 3 IM injections at 0, 2, and 6 months . L1 protein transcribed at most superficial level . Protection Against HPV 6, 11, 16, and 18 . Upon desquamation, HPV virions infect o Remember, together these account for 90% of adjacent basal stem cells genital warts and 70% cervical cancer cases! - Natural History o Indications o 75-90% of infections clear within 1 year4 . All women ages 9-26, regardless of sexual o Desquamation of epithelial cells history o Cell-mediated immunity Recommended at age 12-13 o Low-levels of antibodies - Efficacy10 o (very limited, significant loss of Ab’s within 3 yrs) o 100% effective: CIN, CIS, invasive cancer caused by - Progression HPV 16/18 o Anogenital condyloma acuminata (genital warts) o 100% effective: genital warts due to HPV 6/11 - o Oral and laryngeal papillomas Now indicated for all males between the ages of 9-26 o Cervical, vaginal, and vulvar (and penile) dysplasia, for the prevention of genital warts.*** carcinoma in situ (CIS), and invasive cancer o Since penile/anal cancer is rare, hard to do a study - Immune Evasion3 to show its preventative but it DOES prevent o Down-regulation of interferon expression transmission to female - . decreased cytotoxic T-cell activation The Problem: barriers o No cytolysis o Time… or lack thereof . no release of inflammatory cytokines o Cost o No viremia o Stigma . limited antibody response o Support - o Thus, cellular immune system is not activated and COST HPV may persist… o Without Insurance- - Genital Warts . Each Vaccine = $180 o Prevalence is 1%, but 5.6% of sexually active 18- . Total Out-of-Pocket= $540 59 year olds self-reported a history of genital o With Student Insurance Plan- warts5 . Each Vaccine = $60 o Peak incidence: 20-24 years6, women 67% . Total Out-of-Pocket = $180 -
2 CDM II Written Exam 2, 2010 MT - Support . Increasing affordability, accessibility and o Need for University support for women’s health acceptability of HPV vaccine will increase rates and preventive medicine of vaccination. o Need for advocacy from peers, faculty, staff, and o What do we want to know? institution . Vaccination rates o Need to be on the forefront of advances in . Knowledge medicine . Attitudes - Goal: Make the HPV vaccine (Gardasil)… . Barriers 1) Affordable . Facilitators 2) Accessible - Research: the process 3) Acceptable o Data collection: - Affordability . Surveys o Insurance coverage Baseline . Aetna medical student insurance: 80% of costs Post-intervention o Dr. Jeffrey Gold: $18,000 . Counting UHS consent forms . Fund remaining 20% for students with Aetna by De Schiavone . Pay all costs for students without coverage No patients identified by study personnel o Office of Student Life: $1,000 available o Data Analysis . Educational lectures, fundraising materials . Preliminary results o Fundraising event: $572 o Publication - Accessibility . Presenting credible data to potential donors o Stock HPV vaccine (Gardasil) at UHS . Providing a model for others . No appointment necessary - Preliminary Results o Eliminate unnecessary steps o Baseline: . Direct billing from UHS to insurance . 45/167 vaccinated o Reminder system through Merck . Only 4/45 at UHS - Acceptability o Post-intervention: o Two educational lunch lectures . 48* more vaccinated at UHS alone . Dr. Donna Woodson: “Women’s Health, HPV, - Barriers and HPV-related disease” o Cost: 29% . Dr. Sanford Kimmel: “Gardasil: The HPV o No benefit: 23% Vaccine” o N/A: 21% o Informational materials o No HPV: 11% . Handouts provided by Merck - Where do we go from here? . Handouts from CDC Website o Funding . Posts on social networks . Grants and Private Donors o Fundraising event: THINK TEAL! . Further Fundraising . Awareness o Expansion . Conversation . Extend funding to include other HSC students . Dispelling stigma o Collaboration - Publicity : UT News, UT matters . Providing a model for others to initiate similar - Research projects o Hypothesis: . Working with community organizations and . Significant barriers to HPV vaccination exist local schools to increase awareness and access - Unresolved Issues o Does vaccination promote promiscuity? o What about therapeutic vaccines? o Who is the target population? o Can we increase pap smear intervals? o At what age to we start/stop o Who do we vaccinate? o Bivalent vs. quadrivalent vaccine? vaccination? o What about married/monogamous o Long-term effects? o Do we need Boosters? women? o Long-term immunity? o Cost-effectiveness? o What about lesbian women? Gay men? o Herd immunity? o Cross-protection against other o Pharmaceutical financial agenda? o Male vaccination? serotypes? o Mandatory Vaccination? o Costs?
3 CDM II Written Exam 2, 2010 MT Public Health 2: Reducing Local Low Birth Weight - Objectives oTo identify resources for local birth weight statistics oTo describe who care coordinators are and how they can help physicians oTo identify the contributing risk factors and barriers that effect low income pregnant women in Lucas County - Objective: To identify resources for local birth weight statistics oResources . Ohio Department of Health- Information Warehouse Births, Cancer incidence, Deaths, STD, Hospital Data http://dwhouse.odh.ohio.gov/ . Ohio Department of Health-Vital Statistics Birth, death data, pregnancy, abortions, fetal deaths, marriage and divorce http://www.odh.ohio.gov/healthStats/vitalstats/vitalstatsmainpage.aspx oHealthy People 2010 (didn’t meet any goals bc goals set too high) . Target Goals set nationally . http://wonder.cdc.gov/data2010/ - March of Dimes . Birth specific information . http://marchofdimes.com/PeriStats/ - Lucas County Initiative to Improve Birth Outcomes oToledo Community Foundation Call to Action-2006 oLucas County rate higher than the state & nation oDirect health care costs for premature babies during the first year of their lives average $41,610 compared to $2,830 for babies born healthy and full term (March of Dimes) oLow Birth Weight leads to infant mortality Target this as a surrogate oThe community responded by forming the Lucas County Initiative to Improve Birth Outcomes . Piloting the Pathways Outcome Model developed by Drs. Mark and Sarah Redding in Mansfield, Ohio . Community Health Access Project (CHAP) 1990 to 2004, the low birth weight rate decreased from 20 per 100 live births to 5.5. oPathways Model . Create a community HUB . Identify those at risk . Connect them to an evidenced based intervention . Contract for positive outcomes - Looking at Local Statistics (< 5.5 lbs is low birth weight) oLow Birth Weight Rates . In 2006, 9.6% of births in Lucas County were of low birth weight The primary zip codes had 13.7% low birth weight babies The secondary zip codes had 10.2% low birth weight babies (Source: ODH Vital Statistics) - Infant Mortality Rates oFor 2005-2007, the infant mortality rate is . 13.1 deaths per 1,000 live births in 43604, 43607 & 43610 . 8.7 deaths per 1,000 live births total target area rate . 8.6 deaths per 1,000 live births Lucas County rate - Objective: To describe who care coordinators are and how they can help physicians oCare Coordinator Role . Member of the community: often are the minority ethnicity like the community they serve . Find women in the target population and enroll them into program . Provide care coordination to identify and eliminate barriers of women to prenatal care Transportation, hiding pregnancy have been threw it before . Connects women to care . Educate and empower women to connect to social service agencies
4 CDM II Written Exam 2, 2010 MT
- Community Care Coordination oMercy St. Vincent Medical Center - Family Care Center oNeighborhood Health Association oToledo Hospital Help Me Grow oToledo-Lucas County Health Department - Before the Care Coordinator Intervenes - What the Care Coordinators Do Provide a centralized information source for moms - How can Care Coordinators help Physicians? oHelp “translate” physicians instructions ex diabetic misunderstood diet instructions was on 1000-calorie diet - Objective: To identify the contributing risk factors and barriers that affect low income pregnant women in Lucas County o Risk Factors o No transportation o Mental illness o African American o Unaware of the pregnancy o Homeless o Drug Use o Domestic violence o Less than 18 years old o Tobacco use o Poor living environment o Unmarried o No insurance o Poor health of the mother o Low income o Women with previous birth in last o Non-compliance with medical o Prior poor birth outcomes 18 months appointment o Residing in a zip code with a history o Late entry into prenatal care (after o Personal problems of a high percentage of low birth 13 weeks) o Unwanted pregnancy weight - Most Common Risk Factors - Most Common Barriers oOf the 508 women enrolled in the program: oOther . 429 (84%) are low income oTransportation . 403 (79%) are unmarried oNo show/no explanation given . 375 (74%) are African American oScheduling conflicts . 116 (23%) had late entry into prenatal care oBeliefs/attitudes of others influencing client . 111 (22%) had personal problems oFinancial - Literacy oHealth literacy ≠ literacy oThe problem of limited health literacy is greater among: . Older adults . Those who are poor . People with limited education . Minority populations . Persons with limited English proficiency (LEP) oPeople with limited literacy often report feeling a sense of shame and anger about their skill level. oIndividuals with poor literacy skills are often uncomfortable about being unable to read well, and they develop strategies to compensate. ohttp://www.health.gov/communication/literacy/powerpoint/healthliteracy.ppt - Literacy Resources ohttp://www.ama-assn.org/ama/no-index/about-ama/8035.shtml ohttp://www.online-utility.org/english/readability_test_and_improve.jsp ohttp://www.literacytrust.org.uk/campaign/SMOG.html ohttp://www.harrymclaughlin.com/SMOG.html ohttp://www.nlm.nih.gov/medlineplus/etr.html
5 CDM II Written Exam 2, 2010 MT Public health 3: Advocacy and healthcare access: Being a physician to your community not just your patients - Objectives 1) The learner should be able to identify aspects of public health practice that contribute to population health 2) The learner should be able to identify several aspects of effective advocacy 3) The learner should be able to identify some of the strengths and current failings of the US health system and the planned reforms being proposed by congress. 4) The learner should be able to identify some of the consequences of being uninsured in America - Pop Quiz oWhat do you believe are the top health activities that will save the most healthy years of life? - Did you mention these? o Clean water o Prenatal care o Occupational safety and health o Sanitation o Environmental protection o Control of alcohol, tobacco and o Healthy food o Prevention of war firearms o Adequate housing o Sexual and reproductive health o Mental health and substance abuse o Immunizations education services o Safe roads and cars o Preventive medical carE - Top 20 Causes of Mortality Throughout the World - All countries Rank Cause Total deaths (in thousands) % of total 1) Ischaemic heart disease 8) Malaria 14) Self-inflicted 2) Cerebrovascular disease 9) Cancer of 15) Stomach cancer 3) Lower respiratory infections trachea/bronchus/lung 16) Cirrhosis of the liver 4) HIV/AIDS 10) Road traffic accidents 17) Nephritis/nephrosis 5) COPD 11) Childhood Diseases 18) Colon/rectum cancer 6) Diarrheal diseases 12) Other unintentional injuries 19) Liver cancer 7) Tuberculosis 13) Hypertensive heart disease 20) Measles
- Source: The World Health Report, 2003, The World Health Organization (WHO). - Number of deaths for leading causes of death in U.S. (2006) oHeart disease: 631,636 oDiabetes: 72,449 oCancer: 559,888 oAlzheimer's disease: 72,432 oStroke (cerebrovascular diseases): 137,119 oInfluenza and Pneumonia: 56,326 oChronic lower respiratory diseases: 124,583 oNephritis, nephrotic syndrome, and nephrosis: oAccidents (unintentional injuries): 121,599 45,344 oSepticemia: 34,234 - Public Health oActions that protect all Americans and their communities from preventable, serious health threats and striving to assure community-based health promotion and disease prevention activities and preventive health services are universally accessible in the United States. oIn order to more fully and effectively achieve a healthier nation we need to ensure the underlying social and economic conditions that allow individuals and communities to be healthy. oWe must shift from a nation solely focused on treating individual illness to one that also promotes population-based health services that encourage preventive and early intervention practices. oPublic health and the prevention strategies that it promotes form the foundation for health system reform. Delivering resources to entire communities has more positive health impacts on people than individual interventions alone. Population-based programs address main causes of disease, disability and health disparities for a wide range of people and can help achieve increased value for our health dollar. These programs, in conjunction with stronger health care coverage and delivery, will lead to a true change in our nation’s health. - Public Health Priorities oRebuilding the public health infrastructure. oEnsuring access to health care. oEliminating health disparities. - Who Are The Uninsured? o46 million uninsured despite $2.2 trillion per year or 16% of GDP . Employed (50%) !!!, Children (25%), Unemployed (5%)
6 CDM II Written Exam 2, 2010 MT - Health Care costs oMedicare is not socialized medicine. It is social insurance just like Social Security. When we created Medicare in 1965, Canada created a Medicare system for Canadians of all ages. They even call it Medicare just as we do. Prior to 1965, Canada had a private insurance system just like ours. Their ability to control costs and provide care to all is proof that such a system can be changed and could work for all of us. Taiwan had a system like ours with many uninsured. Just a decade ago, after study, they rejected the private insurance model and created a single payer Medicare system for all Taiwan’s citizens. They made the transition and covered everyone with no increase in spending. The Canadians covered everyone, the Taiwanese covered everyone, and we did it for seniors with better cost control and better outcomes. We could do it for everyone but it is a tough political problem. It is up to us to develop the political will for change. - Health care spending oAt the same time that the number of uninsured is growing, the costs are soaring. Now over 2 trillion (with a T) dollars each year. We now spend twice as much as most other nations per person per year and still fail to cover more than 47 million of our friends, neighbors and family. Health care now consumes over 16% of gross domestic product. This is 50% higher than the next most expensive country Switzerland and they cover everyone. This excess cost is built into every American product and reduces our competitiveness in the global marketplace. This means lost jobs and reduced economic growth in addition to a more sickly and disabled work force due to lack of insurance to cover basic and preventive care. oPeople are becoming more and more unable to pay their medical bills - Many Americans Can't Afford the Basics oThey are more likely to have their utilities cut off, be behind on the rent or mortgage, to not have enough food in the home and, of course, they have higher unmet medical care needs. Most of the uninsured can’t afford to buy insurance especially when they can’t even afford to keep the lights on. - Number Uninsured in Poverty 1967-2001 oAs can be seen by the graph, up until about 10 years ago the uninsured and those in poverty were tracking quite closely. Now the lines have crossed. Steadily more middle class people are losing their insurance or working at jobs that don’t have insurance benefits. This is politically important because, in America, not much changes because the poor are in trouble. However, when the middle class gets in trouble things change. but middle class affected now - Unmet Health Needs of the Uninsured oA recent study documents that the uninsured are less likely to get preventive care such as mammograms, pap smears, or blood pressure checks. They are also less likely to get appropriate diabetic care such as eye exams, foot care and cholesterol checks. You can see that many insured individuals also fail to get the best care. - Chronically Ill and Uninsured oUninsured have same chronic illnesses, but don’t get the care for them - Death due to uninsurance o18,314 Adult Deaths Annually Due to Uninsurance o Spread across the country, it happens one victim at a time every day but is just as deadly and goes on day after day month after month. In fact, two more people will die from lack of insurance in America while you listen to this presentation. This is just the deaths and does not include the disability and suffering that go along with untreated illness. This data is from 2002 and the latest update by the Urban Institute now estimates that more than 21,000 die each year from lack of health insurance alone. - Illness and Medical Costs, A Major Cause of Bankruptcy oNearly half of all bankruptcies involve a medical reason or large medical debt o326,441 families identified illness/injury as the main reason for bankruptcy in 1999 oAn additional 269,757 had large medical debts at time of bankruptcy o7 per 1000 single women, and 5 per 1000 men suffered medical-related bankruptcy in 1999 o2005 study confirms the above findings and notes that 3/4 of those bankrupted had insurance at the start of their illness! oAmazingly ¾ of those who went bankrupt had insurance at the start of their illness. Insurance should protect against financial catastrophe. However our high co-pays and deductibles can bankrupt all but the wealthiest of Americans
7 CDM II Written Exam 2, 2010 MT - Private Insurers’ High Overhead oThe insurance overhead for our single payer national health insurance program for those > 65, Medicare, is only 3 %. oPrivate insurance often consumes 15 to 25% of the premium dollar for administration and profit before a single medical bill gets paid. How can this be? Medicare does not have to sell, broker, advertise or make a profit for stock holders. Everyone is in at age 65. Medicare has no complex contracts or referral networks. Medicare is simple. They hire insurance companies to just process the bills. There is simply a lot less work to do. On the other hand, chasing money in the rest of the mixed up system of private and for profit insurance is complex work. - Growth of physicians & administrators oMore administrators than physicians and growing faster! oWe now spend over 30% of the health care dollar on administration rather than care. No other country comes close. oIf we spent the same amount as Medicare on insurance administration, we would have enough money to cover all the uninsured and improve coverage for the rest of us. - Investor-Owned Care: Summary of Evidence oHospitals: Costs 3%-11% higher, fewer nurses, higher overhead, death rates 6%-7% higher, fraud oHMOs: Higher overhead, worse quality, collaboration with tobacco industry oDialysis: Death rates 20% higher, less use of transplants & peritoneal dialysis, fraud oNursing Homes: More citations for poor quality, fraud oRehab Hospitals: Costs 19% higher oMedicare Advantage HMO’s: 11% more expensive - Non-group Plans, High Overhead o if everyone had individual insurance plan, costs double - CBO on price sensitivity oThey modeled what the uptake of insurance would be for a typical working person who did not have employer based insurance in August 2005. oA 50% subsidy ($1700 per person per year) would increase those buying insurance from about 16% to about 20%-an increase of about 4%. o Subsidies not good enough - “Mandate” Model for Reform Force you to buy private insurance oExpanded Medicaid and an Insurance Exchange oFree for poor oSubsidies for low income oBuy-in without subsidy for others with higher incomes oEmployer mandate + Individual mandate oEmployer subsidies oNo more pre-existing condition exclusions oExpanded funding for primary care and prevention - “Mandate” Model Cost savings through EHR/IT, chronic disease management, cuts to Medicare Advantage plans and pharmaceutical prices for Medicare. Increased insurance regulation. Government brokers private coverage through an insurance exchange (e.g. FEHBP) - “Mandate” Model - Problems oAbsent cost controls, expanded coverage is unaffordable. Subsidies will need to be large and costly. Who will police the mandates? oComputers, care management, prevention not shown to cut costs. oAdds administrative complexity and cost; retains wasteful private insurers. oCan’t buy into the exchange if you have bad insurance through work. oImpeccable political logic, economic nonsense - Crimes and Punishments in Massachusetts o$2000 fine for not having insurance is more than many criminal offences (ex. domestic abuse)
8 CDM II Written Exam 2, 2010 MT - Why There Will Never Be an Efficient Competitive Market for Health Care Services 1) there should be easy entry and exit from the market for both the buyer and the seller. 2) The consumer is sovereign. The buyer not the seller determines demand and the buyer wants the most for the money. 3) there must be easy access to adequate information for buyers to make a choice of products and services 4) The seller optimizes quality and meets market price to maximize profits 5) no natural or government supported monopolies exist and no significant external forces exist to distort the market oYou can’t exit the market when you are very ill-- you buy or die. The doctor not the patient orders the tests and treatments. The search for information about symptoms is why you go to the doctor. Even a good doctor is sometimes unsure of a patients diagnosis or what the long term costs will be until after some very expensive tests are done. For example if you are in agony from a ruptured appendix are you going to haggle with the surgeon over his fee on the way to the operating room? The most complex and costly services are the least negotiable. If open heart surgery was on sale would you have two? The most expensive services are necessary but not really desired like a new car or a Rolex. Most economists recognize that health care is not a normal product and not subject to the usual market forces. oThe market for health care services fails to pass the test on every element - Health Care for All Ohioans Act and HR 676, The “Improved Medicare for All” model oUniversal - covers everyone oComprehensive - all needed care, no co-pays oSingle, public payer - simplified reimbursement oImproved health planning oPublic accountability for quality and cost, but minimal bureaucracy - What Would It Look Like? oEveryone receives a health care card assuring payment for all needed care oComplete free choice of doctor & hospital oDoctors and hospitals remain independent and non-profit, negotiate fees and budgets with NHP oLocal planning boards allocate expensive technology oProgressive payroll income and sales taxes go to health care trust fund with reserves like any insurer oPublicly accountable agency processes and pays bills - How Reform Happens in the USA oCongress and regression to the mean = incremental reform only, 50 states = 50 chances oReform must be tried at the state level and be proven to be successful and that the sky will not fall oNeed to be a broad grassroots movement in support of reform and this may take years or even decades to build - Social Reforms That Were First Passed at the State - Phony vs. Real Reform Level oPhony oWomen’s suffrage . Choice of HMO/insurer oChild labor laws . Coverage = Co-pays, exclusions etc. oWorkers compensation . Security = Lose it if you can’t work or can’t pay oSocial security disability . Savings = Less care for you and more profits for o40 hour work week insurers oFamily and medical leave oReal oEnvironmental laws . Choice of doctor and hospital - . Coverage = First $, Comprehensive . Security = For everyone, forever . Savings >$300 billion on bureaucracy - What Can You Do? oYou can join SPAN Ohio or another single payer health reform group in your home state. (Spanohio.org and everybodyinnobodyout.org have links and contact persons) oYou can join Physicians for a National Health Program (pnhp.org) in support of HR676. oSpeak out. Write your politicians, friends, neighbors, and newspaper editors. Send money.
9 CDM II Written Exam 2, 2010 MT oThis is the civil rights struggle of the new century. You need to be with us to fight for yourself, your family and your friends. The common ground? We will all likely be patients some day - Top 10 Rules of Advocacy 1) Get to know your legislators and the legislative staff that will be working on the issue you want to affect. Work at every level (neighborhood, city, county, state, federal, world). 2) Get to know news reporters who cover your issue and become a resource to them. They are often happy to let you write the story. 3) Identify and work with partners who care about your issue. Organize! 4) Identify, meet with and listen to the opposition. They are telling you the issues you need to address. 5) In policy and politics there are no permanent friends and no permanent enemies. Look for open mindedness and be open minded yourself. 1) Top 10 Rules of Advocacy 6) Be honest, straight forward and never lie to your allies, the media or legislators. Do not make promises you can’t keep. You must be a reliable resource to them. 7) Remember names and say thank you. 8) Learn the legislative process. 9) Be brief, clear, accurate, persuasive, timely, grateful and polite. 10) Be persistent!
10 CDM II Written Exam 2, 2010 MT Public Health 4: Epidemiology &Surveillance - Surveillance Systems oEpi-Center oEpi-X oOhio Public Health Communication System (OPHCS) oOhio Disease Reporting System (ODRS) - Ohio Administrative Code oSelect diseases with Public Health implications are reportable to local Health Departments from laboratories, medical staff, or citizens. oHIPPA allows us to obtain this information. - Reportable Diseases in Ohio oClass A &B: Anthrax, meningitis, SARS, diphtheria etc - Exclusions & Isolation oExclusion: Select Enteric diseases for sensitive occupations* . Return to work or day care may require 2 or 3 negative stools . *OAC sensitive occupation = food service, direct healthcare provider, day care worker, or day care attendee . Exclusion: Vaccine preventable for school or work . Those with vaccine preventable disease may be excluded from school or work for a specified number of days . Isolation: Tuberculosis (may require isolation) . TB may require repeat sputum smears for release - Quarantine & Isolation: OAC 3701-3-01 oIsolation: “separation of an infected individual from others during the period of disease communicability in such a way that prevents as far as possible the direct or indirect conveyance of an infectious agent to those who are susceptible to infection..” oQuarantine: “restriction of the movements or activities of a well individual that has been exposed to a communicable disease during the period of communicability of that disease and in such a manner that transmission may have occurred “ - Single Disease Case - Outbreak 1) Health Department role in interviewing an oCase definition of an outbreak – The occurrence of individual with a confirmed reportable illness two or more cases of a similar illness with a 2) Others ill?→ Outbreak determination common exposure 3) Health care provider information/contact oOutbreak Notification 4) Source of exposure & or vector? oLaboratory 5) Sensitive occupation? oHealthcare provider 6) Contact/contact tracing for select vaccine oCitizen/schools preventable, tuberculosis, select STD, bacterial oState/Federal Public Health Entity (Pulsenet) meningitis 7) Exclusion necessary? 8) Travel/Pets 9) Pets 10) Vaccine Status (if applicable) 11) Notify Environmental Health - - Outbreak Reporting Examples oSalmonella oMRSA oE-Coli 0157:H7 oScabies/Head Lice oHepatitis A oNorovirus oAcinetobacter oNormal Childhood illnesses o; 5th Disease, Hand Foot & Mouth, Varicella, Strep
11 CDM II Written Exam 2, 2010 MT - Salmonella oOver 2000 serotypes oTemporal Pattern: Increase in Summer oReservoir: Poultry, rodents, reptiles, amphibians, swine, cattle, dogs, cats, humans oTransmission: Person to person fecal-oral, or . food contaminated by . contaminated water, . or meat, and peanut feces, raw vegetables, butter or . eggs or egg products, . peanut products oOnly 3% of Salmonella cases are estimated to be laboratory confirmed and reported in the US o11% of cases under age 21 and 6% of all cases are estimated to be related to reptile or amphibian contact oReported Incidence of Salmonella in Ohio and Lucas County 2003-2007 oSalmonella in Lucas County using GIS Mapping - E. Coli 0157:H7 oTemporal Pattern: Increase in summer oReservoir: Cattle, possible deer, humans oTransmission: Ingestion of undercooked raw . ground beef or . vegetables, melons, . sprouts, . person to person contaminated cider, coleslaw, alfalfa contaminated water - Lucas County Trends oSalmonella & campylobacter have shown slight ↓ trend over 06-07. Lucas follows nationwide pattern of increased cases in summer & early fall. Reptile contact reported in a number of local cases. oE. coli 0157:H7 rates remain variable, consumption of undercooked ground beef a factor in local cases and in national data. o4 cases of listeria were reported in Lucas in 2003-2007, in immune compromised individuals. o(USDA/FDA/CDC education campaign for pregnant women & changes being implemented at food processor level) - National Enteric Trends oSalmonella & Listeria decreased ~30% - Hepatitis A Clinical Features oIncubation period 28 days (range 15-50 days) oIllness not specific for hepatitis A oLikelihood of symptomatic illness directly related to age oChildren generally asymptomatic, adults symptomatic - Hepatitis A Epidemiology oTransmission Fecal-oral oTemporal pattern None oCommunicability 2 weeks before to days after onset oReservoir Human oNational Hepatitis A Risk factors 1990-2000 (CDC, Epidemiology and Prevention of Vaccine Preventable Diseases, 10th Edition 2008) - Hepatitis A Cases Reported in Lucas County 2003-2008 - Countries/Areas Associated with Hepatitis A and - Brazil/Tropical South America Travel in Ohio Citizens 2003-2007 - Eastern Europe/Russia/Western Europe - Mexico/Central America/Carribean - Australia/Southwestern Pacific Islands - India/South Asia - Middle East - East Africa - Influenza Epidemiology oReservoir Human, animals oTransmission Droplet . Contaminated Surfaces oTemporal pattern Peak December – March , in temperate climate may, occur earlier or later oCommunicability 1 day before to 5 days (after onset (adults))
12 CDM II Written Exam 2, 2010 MT - Influenza Surveillance - What’s reportable? oHospitalized cases associated with influenza oPediatric influenza deaths oAny influenza A novel virus infection oSentinel Site - Influenza Activity for Lucas County 2007-2008 - Tuberculosis oTB Cases in Lucas County . 2001 – 10 cases . 2004 – 4 cases . 2007 – 4 cases . 2002 – 4 cases . 2005 – 11 cases . 2008 – 8 cases . 2003 – 7 cases . 2006 – 9 cases - Lab Communication - Treatment of Active TB Disease oNotification of all positive AFB smears oInitial Phase: - Reporting a TB Case . Isoniazid oSuspect Cases . Rifampin - Hospitalized Suspects . Ethambutol oIsolation . Pyrazinamide oPPD oContinuation Phase oHIV Testing . Rifampin oBaseline Liver Function Tests . Isoniazid o4 Drug Regimen - Role of the Health Department - oHospital Visit oContact Investigation oDOT – Directly Observed Therapy oCommunication with the state TB controller
13 CDM II Written Exam 2, 2010 MT Public Health: Infection Prevention in Healthcare - IOM - 10 Rules for Health Care - Infection Prevention in the Next Decade oCare is based on continuous healing relationships. oProtecting yourself and co-workers oCare is customized according to patient needs and oProtecting the patients values. oProtecting the UTMC work environment oThe patient is the source of control. oProtecting the bottom line oKnowledge is shared and information flows freely. oDecision making is evidence-based. oSafety is a system property. oTransparency is necessary. oNeeds are anticipated. oWaste is continuously decreased. oCooperation among clinicians is a priority. - - Objectives oDescribe methods of protection for the health care worker in the patient environment oDescribe methods of preventing health care acquired infections in patients oDescribe the fiscal outcomes of reducing infections and promoting an environment of safety for staff and patients
- Infection Prevention in the Next Decade - Prevention oProtecting yourself and co-workers oVaccinations: oProtecting the patients . Hepatitis B series oProtecting the bottom line . Varicella series - Protecting Yourself and Others . Measles, Mumps, Rubella oPrevention methods . Annual Influenza vaccination oProtection methods . H1N1 vaccine oFollow up . TB status - Prevention - Protection oOrientation oHand hygiene . Facility oIsolation bundle . Rotation specific oSafety equipment . Safety Education oSafe work practices . Blood borne Pathogen Training oQuality Measures . Annual Safety Training . Emergency Preparedness - - Hand Hygiene oExcuses we have heard: o“ Not Me” Doctors and nurses hands culture a . “ I didn’t touch anything” lot of bacteria . “ I don’t plan to touch anything” oSoap and Water . “ I just stood at the door to talk to the patient” . Indicated when hands are visibly soiled . “ I kept my hands in my pocket the whole time” . Before and after using the restroom . “ I had my hands under my arms the whole . After caring for a patient with C-Diff time” oWaterless Hand Scrub oExperiment . Alcohol Hand Sanitizer . Volunteers will plate their hands and we will Found throughout the hospital send you the results Portable, Quick oHand Hygiene Compliance oSurgical Scrub . 10 hours per week of hand hygiene . First scrub of the day is traditional observations (large “N”) . Following scrubs: alcohol scrub with CHG (adds Joint Commission due any time sustainable kill)
14 CDM II Written Exam 2, 2010 MT
Reporting compliance rates to staff, Administration provided daily feedback managers and administration
15 CDM II Written Exam 2, 2010 MT Protection . Alcohol Wipes oTools Drying to skin . Hospital grade disinfectants No sustainability on surfaces . Personal protective equipment . What’s Clean, or Dirty? . Isolation gear . Endoscopes . Signs, other communications Must be cleaned and processed between oCleaning patients . Disinfectant Sprays Requires manual cleaning Quat and Bleach cannot be mixed Following by high level disinfection Spraying can cause respiratory difficulty oSolutions are monitored for effectiveness . Disinfectant wipes Serial number and patient must be Use with caution documented. Not good on skin . avoid this: Doctor did it. . - Follow up: If all else fails, what do I do? oTransparency . If you get a needle stick, report it . If you make a mistake, correct it . If you find a mistake, report it . If you see someone about to make a mistake, speak up . Learn by yours and others mistakes
- Infection Prevention in the Next Decade - Progress: Ventilator-acquired pneumonias have oProtecting yourself and co-workers decreased substantially oProtecting the patients - Strategies to Prevent Central Line Related Blood oProtecting the bottom line Stream Infections - Protection oRight site oIsolation Bundle . IJ vs. Subclavian . Gown, mask gloves, respirator, HEPA Hood oRight catheter . Private room, private room with negative air oRight technique flow, HEPA filter . Maximal Sterile Barriers . Hand hygiene oRight Prep . Communication . Clorhexidine for skin - Isolation Gear oRight dressing oAirborne Isolation Protection . Gauze or clear . N-95 Respirator oRight securement . HEPA Hood . Suture-less . Do not deface your mask, your life may depend oRight Asepsis on it . Hand hygiene - Safety for the Patients . Sterile garb oStrategies to Prevent VAP - Results: Decreased substantially . VAP Bundle Head of the bed up 30-45 degrees “Sedation Vacations” Aggressive oral care and suctioning Prevent DVT’s Prevent peptic ulcer disease Exemplary Hand Hygiene - Infection Prevention in the Next Decade
16 CDM II Written Exam 2, 2010 MT oProtecting yourself and co-workers - IC Rounds SICU Room 2218, January 11, 2010 oProtecting the patients VIOLATIONS oProtecting the bottom line 1. Oral care suction left from previous patient - Effective Antibiotic Therapy 2. Aplicare packet contaminated oAnnual Antibiogram 3. Multiple lab tubes close to expiration . Rates the effectiveness of antibiotics 4. Sharps not disposed of oAntibiotic restriction 5. Open petroleum packets . Vancomycin 6. Biohazard bag in refrigerator oSCIP – pre-op antibiotic timing 7. Insulin pen left from previous patient . 60 minutes prior to incision 8. Expired culturettes oSCIP – D/C antibiotic within 24 hours post 9. Sterile urine cup seal broken - Aggregate attributable patient hospital costs by site oCart visibly dirty, petroleum in drawers and on the of infection top, collecting dirt, spilled talc, several one time oSSI $11,874 - $34,670 use, scissors, pick ups, and hemostats found in cart, obviously dirty oCLABSI $ 7,288 - $29,156
oVAP $19,633 - $28,508
oCAUTI $ 862 - $ 1,007 oCDI $ 6,408 - $ 9,124 -
17 CDM II Written Exam 2, 2010 MT Public Health 5: Assessment and Policy Development - Objectives 1) Describe OH requirements for physician reporting of cancer cases 2) Describe components of establishing causality 3) Define the purpose of H.R 1553 4) List 6 questions that outline USPSTF evidence review 5) Compare and contrast the means by which the USPSTF identifies substantial net benefit of a preventive service 6) Summarize USPSTF recommendations for screening mammography for women aged 50-74 - Assessment - Local and State Agencies oOur role in cancer reporting oSpring 2006: citizens call Sandusky County Health oRole of health departments, local and state Dept (SCHD) oEpidemiology oSCHD contacts Ohio Dept of Health (ODH) cancer - What was reported epidemiologist o35 people in eastern Sandusky county diagnosed oSCHD, ODH, and Ohio EPA collaborate on with cancer at age 19 or younger 1996-2006 (out of investigation 40 childhood cancer cases in Sandusky Co) o20 children in Clyde Oh area diagnosed with cancer since 2001 - - Epidemiology oApril 2007, SCHD and ODH completed an analysis of cancer incidence among childhood residents (ages 0-19) of the city of Clyde and Green Creek Township for the years 1996-2006 and 2002-2006 - Clyde City and Green Creek Township, Surveillance, 1996-2006 oHigher than expected numbers of childhood cancers for 11-year time period 1996-2006 (10 observed, 5.32 expected, SIR=1.88, 95% CI 0.90-3.46) oAnd for more recent 5-year period 2002-2006 (8 observed, 2.47 expected, SIR=3.24, 95% CI 1.40-6.38) oCase Counts increased from 1996-2006, no cases dx prior to 2001 and majority dx in 2005-2006. Data indicate recent temporal phenomenon in pattern of childhood cancers oBrain/CNS Cancer found to be most common among Clyde City and Green Creek Township population and significantly higher than expected based on national data for 1996-2006 oClyde City and Green Creek Township (4 observed, 0.92 expected, SIR=4.35, 95% CI=1.18-11.13) oSandusky County (8 observed, 5.85 expected, SIR=1.37, 95% CI=0.59-2.69) oEastern Sandusky Co childhood cancer cases spiked in 2005-2006, indicating exposure in 2003-2004 if cause was short-lived environmental trigger oStatistical review of “adverse reproductive outcomes” (fetal deaths, LBW, prematurity, infant death, birth defects) did not indicate increase in such adverse outcomes - Causality 1) Temporality oAssociation agrees with currently accepted 2) Strength of association understanding of pathological processes 3) Dose-response relationship oDetermine the extent to which researchers have taken 4) Consistency of evidence other possible explanations into account and have 5) Biologic plausibility effectively ruled out such alternate explanations 6) Alternate explanations oThe condition can be altered (prevented or 7) Experiment ameliorated) by an appropriate experimental regimen 8) Specificity oSingle putative cause produces a specific effect 9) Coherence (considered by some to be weakest of the criteria). oExposure always precedes the outcome When specificity of an association is found, it provides oSize of association as measured by appropriate additional support for a causal relationship. However, statistical tests: the stronger the association, the more absence of specificity in no way negates a causal likely it is that the relation of "A" to "B" is causal. relationship. oIncreasing amount of exposure increases the risk oAssociation should be compatible with existing theory oResults are replicated in studies in different settings and knowledge using different methods
18 CDM II Written Exam 2, 2010 MT
19 CDM II Written Exam 2, 2010 MT Further Analysis o18 childhood cases diagnosed 1996-2007 from Clyde City, Green Creek, York, Townsend, and Riley Townships invited by SCHD to participate in a case review o14 case families agreed to participate (78%) - Variables examined oFamily history of cancer oHistory of infectious disease and vaccination oParent/guardian work history oPotential radiation exposure oEstimated date of conception, age of mom at oHistory of exposure to mononucleosis, and history conception, of surgery oInfectious diseases, illnesses during pregnancy oPotential radiation exposure oExposure to cigarette smoke, alcohol use, and have oHistory of sexually transmitted diseases past oHistory of prescription and over‐the‐counter oExterminate during pregnancy medications oExposure to hazardous/toxic substance during case oLength of residence in Clyde City and/or Green pregnancy Creek oMaternal work outside the home oTownship and drinking water source oBirth weight of case oHistory of farm residence, exposure to animals oHealth problems and treatment at birth oExposure to hazardous/toxic chemicals oHistory of birth defects and hereditary diseases oSchools attended prior to diagnosis oHistory of breast feeding
- Conclusion of Case Review: oNo Factor(s) found that may have played a role in the development of the cancers - Surveillance oIn 2008, Ohio EPA began environmental surveillance in the community, conducting detailed review of dumps/landfills and operations of area businesses oIn January 2009, began additional air and drinking water monitoring in the area oODH also conducted geographic analysis to see areas of Sandusky Co. where of childhood cancers is most likely - Vickery Environmental oCommercial facility, deep well injection tech. to dispose of liquid industrial and hazardous wastes generated off site oFour class I hazardous underground injection wells for disposal oLocated on S. R. 412, near the Ohio Turnpike, approximately four (4) miles north of Clyde - Results oDumps and landfills and VEI compliant with regulations oWater: inorganic compounds, organic compounds and radiologic substances met standards oAir: no unusual concentrations, monitoring continues oOngoing pesticide testing - Geographic Analysis oStatistically significant cancer burden found not only in Clyde City and Green Creek Township study population during 1996-2006, but also in four-township area (Green Creek, Riley Townsend, and York Townships) surrounding and to the northeast of Clyde during both study periods oIn contrast, number of cancers diagnosed in all of Sandusky County was similar to what would be expected in both - Sandusky County o1996-2006: 36 observed, 33.80 expected, SIR=1.07, 95% CI=0.75-1.47, 2002-2006: 17 observed, 15.68 expected - Policy Development: H.R. 1553, ‘‘Caroline Pryce Walker Conquer Childhood Cancer Act of 2008’’ ohttp://www.conquerchildhoodcancer.com/Conquer_Childhood_Cancer_Act_of_2007.htm ohttp://www.govtrack.us/congress/bill.xpd?bill=h110-1553 - USPSTF: U.S. Preventive Services Task Force, independent panel of private-sector experts in prevention/prim care oUSPSTF conducts rigorous, impartial assessments of scientific evidence for the effectiveness of clinical preventive services, including screening, counseling, and preventive medications (considered "gold standard" for preventive) oUSPSTF Mission: Evaluate benefits of individual services based on age, gender, and risk factors for disease
20 CDM II Written Exam 2, 2010 MT oMake recommendations about which preventive services should be incorporated routinely into primary medical care and for which populations. Identify Research agenda for clinical preventive care. - USPSTF Evidence Review oDo the studies have the appropriate research design to answer the key question(s)? oTo what extent are the existing studies of high quality? (i.e., what is the internal validity?) oTo what extent are the results of the studies generalizable to the general US primary care population and situation? (i.e., what is the external validity?) oHow many studies have been conducted that address the key question(s)? How large are the studies? (i.e., what is the precision of the evidence?) oHow consistent are the results of the studies? oAre there additional factors that assist us in drawing conclusions (e.g., presence or absence of dose-response effects; fit within a biologic model)? ohttp://www.ahrq.gov/clinic/uspstf08/methods/procmanual5.htm ohttp://www.ahrq.gov/clinic/uspstf08/methods/procmanualap7.htm - Net Benefit oLarge proportion of total burden of suffering from target condition (minus the additional burden caused by the preventive service) would be relieved from society by implementing the preventive service, even if the target condition is rare (e.g., screening for PKU) oLarge amount of burden of suffering would be relieved from society (minus the amount of the additional burden caused by the preventive service) by implementing the preventive service (e.g., counseling for smoking cessation) oIn both situations, a population can be defined that has a substantial burden of suffering from the target condition, even if rare, and there is a prevention strategy that reduces that burden by a substantial amount oNet benefit would only be substantial if harms of the intervention are zero or small (as in the examples cited here). Thus, both the magnitude of harms and the magnitude of benefits are critical factors in determining net benefits. ohttp://www.ahrq.gov/CLINIC/uspstf/uspsbrca.htm - Required Readings oCancer Reporting in Ohio . Must be reported within 6 months . Reportable: any primary malignant neoplasm, with the exception of basal and squamous cell carcinoma of the skin and carcinoma in-situ of the cervix oCaroline Pryce Walker Conquer Child Cancer Act of 2008 ↑research, establish a national cancer registry, ↑ info . Cancer kills more children than any other disease . 80% of children diagnosed with cancer already have metastases oCritical Appraisal questions (USPSTF manual) . Do the studies have the appropriate research design to answer the key question(s)? . To what extent are the existing studies of high quality? Internal validity . To what extent are the results of the studies generalizable to the US primary care population? External validity . How many studies have been conducted that address the key question(s)? How large are the studies? Precision . How consistent are the results of the studies? . Are there additional factors that assist us in drawing conclusions Ex. dose-response, biologic effects oMethods for arriving at a recommendation (USPSTF manual) . 2 stage method (title/abstract and article) to see if the article applies to the research question oScreening for breast cancer . USPSTF: biennial screening mammography for women aged 50 to 74 years. (Grade B) . The decision to start regular, biennial screening mammography before the age of 50 years should be an individual one and take patient context into account, including the patient's values regarding specific benefits and harms. (Grade C) . USPSTF concludes that the current evidence is insufficient to assess the additional benefits and harms of screening mammography in women 75 years or older. (Grade Insufficient) . USPSTF recommends against teaching breast self-examination (BSE). (Grade D) . USPSTF concludes that the current evidence is insufficient to assess the mammograps in women > 40 years
21 CDM II Written Exam 2, 2010 MT . USPSTF concludes that the current evidence is insufficient to assess the additional benefits and harms of either digital mammography or magnetic resonance imaging (MRI) instead of film mammography as screening modalities for breast cancer.
22 CDM II Written Exam 2, 2010 MT Patient Communication, Special Topics, Interviewing Patients with Disabilities - Learning Objectives o Explain how Section 504 of the Rehabilitation Act of 1973 and The Americans with Disabilities Act impacts physicians. . In §504, the focus is on non-discrimination. As applied to the schools, the language broadly prohibits the denial of public education participation, or enjoyment of the benefits offered by public school programs because of a child’s disability. To encourage compliance, Congress did not create an additional source of federal funding, but instead, conditioned future receipt of federal funds on the district’s compliance with the new requirements. . The ADA was passed in 1990, and seems to pick up where the Rehabilitation Act left off. Borrowing from the §504 definition of disabled person, and using the familiar three-pronged approach to eligibility (has a physical or mental impairment, a record of an impairment, or is regarded as having an impairment), the ADA applied those standards to most private sector businesses, and sought to eliminate barriers to disabled access in buildings, transportation, and communication. To a large degree, the passage of the ADA supplants the employment provisions of §504, reinforces the accessibility requirements of §504 with more specific regulations, but does little to change a District’s obligations to provide educational services to its disabled students . Handicapped persons” means any person who i. has a physical or mental impairment which substantially limits one or more major life activities, ii. has a record of such impairment, or iii. is regarded as having such an impairment. §104.3(j)(1). [References to particular sections of the Code of Federal Regulations are to Title 34 unless otherwise indicated in the text.] o Explain how these laws impact medical practice. o Discuss how perceptions impact the treatment of others o Explain the difference between visible and invisible disabilities o Legal protections for patients with disabilities, such as the Americans with Disabilities Act (ADA) o History of the disability rights movement that led to the implementation of the ADA o The core components of disability study theory o Limitations in conducting a history of present illness and physical exam in patients with varying abilities o Strategies and techniques for overcoming the limitation of interviewing patients with disabilities o The community resources that are available to help maximize the integration of the disabled into the community - Changing Perceptions “In order for students with disabilities to reach their potential, society needs to change its perceptions of the disabled o 18th and 19th Centuries . People with disabilities were viewed as dependent on others (purely medical model) o 21st Century Shift . Movements for disabled people to movements of disabled people . Demand for people with disabilities to be seen as equal partners - Applicable Law o Section 504 of the Rehabilitation Act of 1973 . Colleges and universities receiving federal financial assistance must not discriminate in the recruitment, admission, or treatment, of students. . Students with documented disabilities may request modifications, accommodations, or auxiliary aids which will enable them to participate in and benefit from all postsecondary educational programs and activities. Postsecondary institutions make such changes, when appropriate, to ensure that the academic program is accessible to the greatest extent possible by all students with disabilities. . Under the provisions of Section 504 Universities and Colleges May Not: Limit the number of students with disabilities admitted Make preadmission inquires as to whether an applicant is disabled Use admissions test or criteria that inadequately measure the academic qualifications of disabled students because appropriate modifications were not made for them. Limit the eligibility of a student with a disability for financial assistance or otherwise discriminate in administering scholarship, fellowships, internships, or assistantships on the basis of disability:
23 CDM II Written Exam 2, 2010 MT
Counsel a student with a disability toward a more restrictive career: Measure student achievement using modes that adversely discriminate against a student with a disability. Establish policies, practices or procedures that may adversely affect students with disabilities. . Federal legislation mandates that academic adjustments are made to ensure that otherwise qualified students with disability have access to educational opportunities. o Americans with Disabilities Act . The Americans With Disability Act was enacted by the Senate and House of Representative of the United States of America in Congress. It was established to be a clear and comprehensive prohibition of discrimination on the basis of a disability. - Section 504 of the Rehabilitation Act of 1973 o “No otherwise qualified individual with a disability shall solely by reason of his or her disability, be excluded from the participation in, be denied the benefits of, or be subjected to discrimination under any program or activity of a public entity.” - The Americans with Disabilities Act (ADA) o Requires all public programs and services be accessible to individuals with disabilities regardless of whether or not the entity receives federal funds o The ADA governs all institutions that receive federal funding o Substantial is defined as when the limitation for an individual is greater than the experience in the general population e.g., Unable to lift 10 pounds without significant pain o Someone who is blind in one eye and has near perfect vision in the other may not be considered substantially limited – - ADA Definition of Disability o Someone with a physical or mental impairment that substantially limits one or more major life activities o The phrase major life activities means functions such as: o caring for one's self o performing manual tasks o walking, seeing, hearing, speaking, breathing, learning, and working - ADA Terminology o What Does “Otherwise Qualified” Mean? . Anyone who can meet the academic and technical standards required for admission or participation in the educational program with or without reasonable modifications (ADA, 1990). - Disabilities according to Section 504 - Medical Conditions: o AIDS o Blindness or Visual Impairment o Specific Learning Disabilities o Arthritis o Emotional or Psychiatric o ADD/ADHD o Cancer Disabilities o Traumatic Brain Injury o Cardiac Diseases o Mobility Impairments o Neurological and o Diabetes o Drug or Alcohol Addiction Neuromuscular Disorder o Epilepsy or Seizure Disorders o Mental Retardation o Deaf or Hard of Hearing o Orthopedic Impairment o Speech Disorders - Disability Statistics o 54 million people have a documented disability 20% of U.S. population o 14.4 million undergraduate students o 1.5 million undergraduate students with a documented disability o http://www.whitehouse.go/news/freedominitiative/freedominitiative.html o U.S. Department of Education 2005 - Disability Statistics o 1 out of 11 (9%) undergraduate college students report having a documented disability o 40% Learning disability o 9% Speech o 4% Visual Impairment o 19% Health o 8% Emotional (Mental Illness) o 14% Orthopedic or mobility o 6% Deaf or Hard of Hearing http://ncesed.gov 2003 Report o http://www.icdi.wvu.edu/disability/U.S%20Tables/US11.htm
24 CDM II Written Exam 2, 2010 MT o Invisible Disabilities . Seen in primary care, . Documentation for pt. school, . Documentation psychiatry, peds most work, etc. . Exemplary commonly . Manifestations for pts. . Unacceptable . Learning disabilities, . Home life, work, school, psychiatric disabilities church, extracurricular . Physician expectations activities, volunteering, etc. . Treatment . K-12 example o Post-secondary example . Documentation . Accessible signage . Doorways, ramps . Exemplary . Height of signs . Provision of wheelchairs . Unacceptable . Braille . Accessible parking . Physician expectations . pictorials . Interpreters . Requirements . Physical plant . AS - Transition Issues From High School to College o Most Students, parents, faculty, staff, and administrators are not aware of the differences between secondary and post secondary services o Often faculty, staff, and administrators are unfamiliar with the laws that govern disability services and potential ramifications if students are not granted “equal access” - Eligibility Criteria for Disability Services o Students requesting academic accommodations must present documentation that meets the eligibility criteria for the institution and should include: o Documentation from a professional licensed clinician/medical professional o Current documentation within the last 3-5 years o Statement of diagnosis o Academic limitations imposed by disability o In some cases, a prognosis or possible future changes in the condition - Additional Responsibilities of OA Staff o Advocating for students who disabilities o Educating faculty, staff, and administrators on disability services o Ensuring equal access and opportunity (leveling the playing field) o Assisting faculty in maintaining academic integrity o Maintaining institutional compliance with federal disability legislation - The Spectrum of Disabilities o Many disabilities are visible while others are invisible or “hidden” o Society discounts or disregards a documented disability if it is not visible o Interactions with patients with disabilities o Sharleen A. Suico, MD, Associate Program Director of PM&R, University of Toledo o Individuals with Disabilities o Surgeon General’s Call to Action to Improve the Health and Wellness of Persons with Disabilities 2005 o Worse health status o Causes o Injury or accident o Inadequate resources for o Nature o Progress slowly o Health maintenance o Timing o Some gradually limit while o Prevention of secondary o Pace others hasten death conditions o Personal implications o Visible to outsiders vs. hidden o Optimizing wellness are o Social implications o Engender stigmatization vs. pity inadequate o Disabilities and paternalism o Disabilities o Suddenly o Disabilities o Diverse o Can affect ANYONE - Can refer to any sensory or physical impairments - Cannot make presumptions that individuals with these conditions are, in fact, disabled
25 CDM II Written Exam 2, 2010 MT - Models of Disability o Medical Model . Problem of the person . Directly caused by disease, trauma or other health condition which requires medical care - Social Model: Socially created problem o Matter of the full integration of individuals into society - World Health Organization o In 2001, approved the International Classification of Functioning, Disability and Health (ICF) o Attempts to integrate medical and social models of disability - Identifies 3 interrelated concepts: 1. Impairments are problems in body function or structure such as a significant deviation or loss 2. Activity is the execution of a task or action by an individual 3. Participation is involvement in a life situation - Umbrella term o Impairments o Activity limitations o Participation restrictions - Dynamic interaction between health conditions and contextual factors o Environmental o Personal attributes - Impairments – the actual injury o Ex. Broken leg - Disability – inability to weight bear on the broken leg o Ex. Affects patient’s gait - Handicap – how the disability affects interactions with the environment o Ex. Unable to ambulate long distances to the store or inside the store - Clinician Implications o Potential effects on patient-clinician communication o Incorporating disability appropriately into treatment plan o Physicians should approach clinic encounters just as they would with other patients . Start with CC . Learn more about any impairments . Relationship between patients and their daily environments . Home set-up . Current physical activity level o Support system o Mode of transportation o Attempt to determine patient’s functionality o Use of assistive devices for mobility and ADL’s - Physicians o Should “Treat” the disability o Not only the impairment o Recommend adjustments to environment and the interplay between them - Common Pitfalls o Fail to seek patient’s perspective on his or her impairments o Assume that the disability is the reason the patient is seeking care o Are unfamiliar with the assistive devices that may help their patient o Are not adequately trained to assess the disability o Do not work in settings that accommodate people with disabilities o Medical insurance coverage often lags behinds attainment of SSI and is often inadequate o Poor and disadvantaged people are more likely to be disabled o Applying for disability benefits can be difficult for patient and provider
26 CDM II Written Exam 2, 2010 MT - Some General Tips: o Before assisting a patient with a disability, ask for permission and follow the patient’s instructions o Remember that the wheelchair is an extension of the user’s personal space. Avoid leaning on the wheelchair o Sit down and speak to patient at eye level, especially if they are in a wheelchair o Do not praise for performing normal tasks o Speak directly to patient and not caregivers if present o If you do not understand what the patient is saying, continue to pay close attention and ask questions to clarify o Introduce yourself once you enter the room of any patient who has a visual impairment o Avoid interacting with guide dogs o In referring to patients with disabilities . Mention the person . Then the disability o Wrong – Handicapped man o Correct - “72 yom with an impaired gait due to a right sided weakness” - Lower Extremity Mobility Difficulties o Asking about physical activity should be part of a complete primary care valuation o Act of Walking . Gait, balance, strength and endurance . Gait cycle – stance phase and swing phase o Lower Extremity Mobility Difficulties o How far they can before becoming short of breath o Observe them when they walking into examining rooms or climb onto examining tables o Get Up and Go Test o Standard cross-walks are timed to normal gait speed - Gait Assistive Devices o Often underscore images of debility o Reluctance due to - Sense of social stigma and other complex emotions o Language shift . Old = Wheelchair bound and confined to wheelchair . New = Wheelchair user o Canes o Crutches o Walkers o Wheelchairs . Manual . Power . Scooters – 3 or 4 wheeled o Physiatrist, Rheumatologist, Orthopedist, or Neurologist - Blindness o Introduce oneself as soon as you enter the room o Ask what kind of assistance persons might want o Offer to assist, but let person make first move o Not automatically assume that vision should be the first topic discussed o Useful questions: . Do you have trouble driving at night? . Trouble seeing someone across the street? . Reading a newspaper? . Seeing details on the television screen? . Going up stairs? o Blindness o Depending on individual preferences, give information in: . Large print
27 CDM II Written Exam 2, 2010 MT . Braille . Audiotape . Digital formats - Tips for working with the Blind o Record all pertinent info about their medications in a useful form to them o Ask pharmacist to dispense medications of similar shape in different sized bottles to help differentiate; Keep this consistent o Wrap rubber bands or other tactile clues around the bottle corresponding to the number of times a day they are to take that medication. . Remove one band with each dose, then replace all bands for the next day - Deaf and Hard of Hearing o 9% of Americans have hearing loss o 10% of them with profound deficits o 1 in 1000 children have severe to profound hearing loss o 4-5 children have hearing deficits that impair verbal communication o Deafened pre-lingually typically have different communication patterns and preferences than post-lingually deafened o Deaf and Hard of Hearing o Tend to prefer “deaf” or “hard of hearing” o Hearing impaired imply hearing loss requires a cure o When spelled with “D” represents cultural or linguistic view of deafness . Not an impairment . Cultural Identity - Hearing Assistive Devices o Hearing Aids o Teletypewriter (TTY) o Assistive Listening Devices (ALDs) . Shorthand phrases o Cochlear implants . Portable and lightweight models o Telecommunications Technologies . Pricey and monthly fees . Vibrator beepers or watches o Telephone Relay Services . Flashing lights . Free at all times . Amplified headsets . 7-1-1 . Closed captioning decoders . Communications assistance o . Video relay services - American Sign Language (ASL) o 500,000 Americans o Hand signals, facial expressions and body movements o Vary from country to country - Lip (Speech) Reading o Imperfect o Only ~30% of English words are clearly readable - Important ?’s for hearing history o Age of onset o Face person while speaking o Preferred language, communication modality o Keep mouth visible o Cultural identification o Speak naturally but clearly without shouting or o Educational history, level of understanding spoke & rushing written English o Ensure adequate lighting o ADA requires accommodations to ensure effective o Eliminate background noise communication – patient’s preference o Sign language interpreters - Patient example o 68 yof with a L MCA CVA o Aphasic o RHP – right hemiparesis
28 CDM II Written Exam 2, 2010 MT o Right sided neglect – vision and sensory
29 CDM II Written Exam 2, 2010 MT - Physiatry o Physical Medicine and Rehabilitation o Assess functional needs and provide nonsurgical interventions o Often work alongside therapists o Aim to construct care plans that maximize health and independent functioning - Guidelines for Appropriate Referrals to Physical Therapist o Adapting to new disability o Significant balance or gait disturbance o Significant ROM or strength impairments o Need assessment for a mobility aid o Need training in use of ambulatory aid o Seating or position problems with a wheelchair - Guidelines for Appropriate Referrals to Occupational Therapist o Adapting to new disability o Need assistance with basic or instrumental activities of daily living (ADLs) o Display limited judgment about safety o Need splint or orthotic fabrication o Need adaptive equipment for work o Need home environment evaluation for possible modifications o Driver’s evaluations - Key concepts o Never make assumptions about the abilities, preference or expectations o Disability marks an interaction between a person’s functional abilities and the environmental demands place on them o Disability can be lessened by modifications in the environment o Many assistive devices and adaptive technologies exist to eliminate gap o Physical therapists, occupational therapists and physiatrist are important resources o Providers should seek to alter their practice environments to make it accessible - Patient Resources o http://www.firstcallnwo.org o Information about resources in NWO o Ability Center of Toledo . Home modification/accessibility program o American Parkinson’s Disease Assoc. o Alzheimer’s Assoc, NWO Chapter o Area Office on Aging o Brain Injury Association of Ohio – Lucas o Kidney Foundation of NWO o National Multiple Sclerosis Society – NWO o Spinal Cord Injury Support Group o Area Office of Aging of Northwestern Ohio . The PASSPORT Program – provide older adults with help at home . Caregiver Support – for families and persons caring for older adults o Lifeline – personal response and support services
30 CDM II Written Exam 2, 2010 MT 1. Abdominal Exam - Case oHistory . A 26 year old female comes to the Emergency Room complaining of abdominal pain in the right lower quadrant. She has had some nausea with one episode of vomiting. She denies any hematochezia (red-blood stools lower GI bleed), melena (black tar stools upper GI bleed) or hematemesis. She had a normal bowel movement within the past 24 hours. She denies any possibility of pregnancy. She has had no fever or chills. oPhysical . Blood Pressure-120/80. Heart Rate-100. Temperature-100.2 . Skin is warm and dry. Heart and lung exam is normal. No jaundice or scleral icterus. On abdominal exam, there is no distension. Bowel sounds are hyperactive. On palpation of the abdomen, there is no hepatosplenomegaly. There is tenderness on deep palpation in the right lower quadrant. There is no guarding or rebound tenderness. The pelvic exam is normal. Rectal exam demonstrated stool present which is occult blood negative. oHistory . Jaundice/Icterus . Ascites . Dysphagia/Odynophagia . Dyspepsia . Frequency/Urgency/Dysuria/Incontinence . Hematuria oInspection . Expose Abdomen . Define Regions Quadrants Suprapubic/Flank Regions Epigastrium . Consider Underlying Anatomy oAscultation . Contour . Typically done prior to palpation . Scars . Bowel sounds (borborygmi) . Symmetry Hyperactive . Venous Pattern Hypoactive . Pulsations Absent (After at least 30 seconds) . Hernias (Para-umbilical, Incisional, Inguinal, . Arterial bruits Ventral) oPalpation & percussion oSpecial Exam Techniquies . Light Palpation . Ascites Observe patient response Fluid wave Guarding (Voluntary/involuntary) Shifting dullness Rebound tenderness Puddle sign Detect abdominal wall pathology oLouder farther away ascites . Deep Palpation . Gallbladder Disease Colon “Murphy’s” sign Abdominal Aorta oHold gallbladder, breath in stop inspirat. Liver (with percussion) . Liver Disease oMid-sternal: 4-8cm Asterixis – “Liver flap” oMid-clavicular: 6-12cm Dilated veins, enlargement Spleen Testicular atrophy Kidneys Dupuytren's Contractures hand facia . Kidney Disease/Bladder Disease Direct palpation CVA tenderness Bladder palpation
31 CDM II Written Exam 2, 2010 MT 2. Cardiac Examination - History Palpation oChest Pain (Onset, Character, Severity, oPMI Exacerbation/Relief) oRight ventricular heave oShortness of Breath (Position, Activity) oLeft ventricular thrust oFatigue oGallop oOthers (Palpitations, Syncope, Cyanosis) oThrill oCAD Risk Factors - Percussion - Cardiac Examination - Auscultation oPast Medical History oOrderly Approach oMedications taken . Aortic area oCardiac Surgery or Hospital Admission . Pulmonic area oRheumatic Fever . Tricuspid area oCongenital Heart Disease . Mitral area oMurmur . Epigastrum oPatient position - Identify heart tones . Sitting up, Lying down, Laying on left side, Other oS1 – Closure of tricuspid and mitral valve. High maneuvers pitch. Diaphragm. oJugular Venous Distension/Pulsation oS2 – Closure of pulmonic and aortic valve. High . Estimate of increased right-sided pressures pitch. Diaphragm. . Normally 3 – 4 cm above sternal angle . May split with inspiration . Pulsations consist of “a” wave (absent in A-fib) Fixed, wide, paradoxical and “v” wave (increased in TR) oExtra sounds in systole . Hepatojugular reflux . Click d/t prolapse of MV (High pitch - Description of Findings Diaphragm/Apex) oTiming in relation to cardiac cycle oExtra sounds in diastole oLocation . S3 – Rapid ventricular filling Low pitch, Bell, Apex ↑ filling pressures, dilated ventricles Normal in children . S4 “atrial kick” – Atrial filling into ventricle Low pitch, Bell, Apex Ventricular hypertrophy oExtra sounds in systole and/or diastole . Rub d/t pericardial friction . Murmur - Auscultation – Murmurs oCauses 1) Diseased/Leaking Valve 2) High output 3) Structural defect (ASD/VSD) 4) Altered flow in great vessels oDescribing Murmurs . Timing, Location, Radiation, Intensity (I – VI), Pitch, Quality oSpecial maneuvers (+ Vascular, pulses) 1) Valsalva, 2) Squatting/standing 3) Exercise 4) Hand grasp 5) Amyl nitrate
a wave: atrial contraction. c wave: RV contraction (tricuspid valve bulging into atrium). v wave: ↑ atrial pressure due to filling against closed tricuspid valve. 32 CDM II Written Exam 2, 2010 MT
33 CDM II Written Exam 2, 2010 MT 3. Male Genitalia + Rectal Exam 4. Observation and Vital Signs - History - General Inspection - Testicles . Overall appearance oLumps, Pain, Asymmetry . State of Comfort - Penis . Dress, demeanor and body position oDischarge, Lesions, Curvature, ED . State of awareness and speech - Hernia . Body habitus oPain, Bulging, Reducibility . Odors - Anus - Blood Pressure oBleeding, Masses, Pain . Choose appropriate cuff - General Approach . Patient position oMake patient as comfortable as possible. . Palpate artery oWarm room/Warm hands . Inflate cuff until pulse disappears oPatient standing or lying down . Auscultate blood pressure oGloves . Special situations (leg pressures, palpation, oEquipment (Lubricant, Hemoccult, Cleansing pulse deficit, auscultatory gap, orthostatic BP) towel) - Pulse - Inspection and palpation . Carotid, radial, ulnar, brachial, femoral, oPenis – Skin, Retract foreskin, Glans popliteal, dorsalis pedis, posterior tibial . (Phimosis, Paraphimosis) . Assess amplitude, contour, rate, regularity and oScrotum – Skin, Testes, Spermatic cord symmetry . Epididymis . Normal heart rate 60 – 100 bpm . (Varicocele) . Tachycardia, Bradycardia oHernia – Direct/Indirect - Respiration - Rectal Exam . Rate (10 – 12), Depth, Regularity oStanding vs. lateral decubitus . Tachypnea, Dyspnea - Observation – Hemorrhoid, excoriation, - Temperature ogenital warts . Oral, Rectal, Axillary, Ear - Palpation – Tenderness, masses, prostate - Skin and appendage exam . Body hair (distribution, texture, color) Indirect Direct . Nails (architecture, color, lesions) Frequency Most common, all Less common . Skin (color, texture, temperature, hydration, ages, both sexes scars, lesions) Age & Sex Often in children, Usually men >40, - Percussion may be in adults rare in women . Sets the chest/abdominal wall and underlying Origin Above inguinal Above inguinal tissues into motion, producing audible sounds ligament, near ligament, close to and palpable vibrations. Helps determine if midpoint pubic tubercle underlying tissues are air-filled, fluid-filled or Course Often into the Rarely into the solid. scrotum scrotum . Pleximeter finger struck by plexor finger. During Hernia touches finger Pushes side of finger - Auscultation cough . Stethoscope oQuiet room oGood earpieces oConcentration oDiaphragm/Bell
34 CDM II Written Exam 2, 2010 MT 5. Lung Exam oObserve for use of accessory muscles May be sign of respiratory distress - Signs and Symptoms oParadoxical breathing oDyspnea – Shortness of Breath - Palpation . Subjective sensation of ventilatory insufficiency oSkin – subcutaneous emphysema . Grade I – Speaks in full sentences oRibs – fracture, tumor, contusion, costochondritis . Grade II – Speaks with frequent pauses oTracheal deviation . Grade III – Speaks in single syllables oTactile fremitus – vibration of larynx which is . Grade IV – Unable to speak transmitted to chest wall by tracheobroncial tree. oOrthopnea – Shortness of breath lying down Elicited by asking patient to say “99”. oParoxysmal Nocturnal Dyspnea . Tactile fremitus . Both of these are typically associated with Decreased in conditions that reduce transmission pulmonary edema of sound to chest wall (pleural effusion, oDyspnea can be physiologic (Fever, Exercise) or pneumothorax, airway obstruction) psychologic (Anxiety), and WHEN. Increased in conditions such as lung oCough – Productive vs. Non-productive consolidation due to pneumonia . Productive (Smell, Color) – Typically suggests the - Percussion presence of bacterial infection oProcess of striking the chest wall and then perceiving . Non-productive – Typically suggests “atypical” the character of vibrations that are heard by the ear. infections or non-infectious etiology (ie GERD, Percussion sets the chest wall and underlying tissues in asthma) motion. oHemoptysis – Blood in sputum oPercussion notes may be tympanic, hyperresonant, . True hemoptysis – Bronchial or lung source resonant, dull or flat depending on the nature of the . False hemoptysis – Nasopharyngeal or oral source underlying tissue. Etiologies of true hemoptysis include neoplasm . Dull – pleural effusion, consolidation, and bronchitis (bacterial, fungal, TB) empyema, etc. oChest Pain – Need to differentiate from cardiac causes. oHyperresonance/tympany,emphysema, oPleuritic Chest Pain – Made worse with deep breathing. . pneumothorax Etiologies include infection, neoplasm and collagen oPercussion may also be used to estimate diaphragmatic vascular diseases (RA, SLE, Scleroderma, etc.) excursion (5 – 6 cm) - Lung Segments – Bronchopneumonia often lobar. - Auscultation Obstruction of a bronchus may affect only a single lobe or oUsed to estimate amount of air flow through segment. tracheobronchial tree. Patient needs to be instructed to oMust examine the patient without a gown. breathe more deeply than normal through an open oMust examine anterior, posterior and lateral lung fields mouth. in patients with pulmonary symptoms. oAdventitial (extra) Sounds - Inspection . Crackles (Rales) – short, discrete, non-musical sound oSkin – Sinus tracts – underlying path. caused by previously deflated airway suddenly . Restrictive soft tissue – scarring. reinflated during inspiration. Seen with pneumonia, . Laceration – pneumothorax? pulmonary edema, interstitial lung disease, etc. . Hematoma- rib fracture? . Wheeze (Rhonchi) – continuous musical sound of - Inspection long duration caused by rapid passage of air through oStructural Deformities narrowed or obstructed bronchus. Seen with . Kyphosis asthma, foreign body occlusion, tumor, COPD. May . Lordosis also be associated with prolongation of expiratory . Scoliosis phase. . Pectus excavatum – May displace heart oPleural Rub – pleural surfaces usually rub smoothly . Pectus carinatum against one another. When inflamed, may produce . Barrel chest – Increased AP diameter rubbing sound (like leather strap). Seen with pleuritis or - Inspection pulmonary infarction. oRespiratory patterns oAbnormally transmitted sounds . Tachypnea – rapid and shallow . Egophony – “bleating like goat” . Hyperpnea – rapid and deep (Kussmaul) E to A changes . Cheyne-Stokes . Whispered Pectoriloquy – “1, 2, 3” . Ataxic oBronchophony oAssessment of chest expansion . When these are heard abnormally, it is often a . Should be symmetric reflection of the voice being heard more clearly - Inspection through airless lung such as in pneumonia.
35 CDM II Written Exam 2, 2010 MT
- Other findings in patients with hypoxemic lung disease oClubbing of fingers, Cyanosis, Plethora (neonatal polycythemia) 6. Head & Neck - Eye Exam - Head – Observation and Palpation oExternal Eye - Skull – Shape and Symmetry oEyelids – Symmetry (ptosis) - Scalp – Hair and Skin oConjunctiva - Face – Asymmetry, Tics, Expression oLacrimal gland oEar – Otoscope, Insufflation bulb, Tuning Fork oInternal Eye External ear oSclera – dense, avascular (“white”) oEar canal oCornea – continuous with sclera oTympanic membrane oIris – circular, contractile (“color”) oHearing: Whisper, Ticking watch oLens – behind iris, thickness changes by action of oRinne – Tuning fork on mastoid cliary body oWeber – Tuning fork in midline oRetina – sensory network of eye . (Conductive vs. Sensorineural loss) oVisual acuity – Monocular, binocular . (Tinnitus, Vertigo) oSnellen chart – 20 feet away oNose – Otoscope (Nasal speculum) oMyopia (near sighted) oExternal nose – Shape, size and color o20/200 – Patient can read at 20 feet what average . Evaluate patency person can read at 200 - Palpate oRosenbaum near vision card oNasal Cavity oHyperopia (far sighted) oMucosa oPeripheral vision oDischarge . Estimated via confrontation o(Epistaxis, rhinorrhea) 90 degrees temporal oSinuses 60 degrees nasally oFrontal 50 degrees superiorly oMaxillary 70 degrees inferiorly oTransillumination? - Color Vision - Mouth and Oropharynx - External Exam oLips oObservation: lids, conjunctivae, lacrimal gland oBuccal mucosa, Teeth and Gums oCorneal reflex: oOral Cavity – gloves, tongue blade, gauze and light . CN V – sensory oSalivary duct openings . CN VII - motor oTongue (CN XII – Hypoglossal) oPupillary response: oHard/soft palate (CN IX and X) . Symmetry (anisocoria) oUvula . Accommodation (PERRLA) oPosterior pharynx oExtraocular Eye Muscles: CN III, IV, VI - Neck - Internal Exam oObservation – Symmetry and Masses oOphthalmoscope (Direct, Panoptic) oPalpation oPatient cooperation . Lymph nodes oLens setting (start at 0) . Carotid arteries oMyopia – minus diopters . Jugular veins oHyperopia – plus diopters . Trachea oApproach at 15 degree angle to see red reflex . Thyroid (Hyper/hypothyroid) oOptic disc – Disc margins, papilledema - oVessels – Follow outward from disc oAV ratio (3:5) oVenous pulsations oAV crossings (AV nicking) oHemorrhages oMacula densa (Fovea centralis)
36 CDM II Written Exam 2, 2010 MT
37 CDM II Written Exam 2, 2010 MT
7. Neurological Exam . Aphonia: Whisper - General Approach . Dysphonia: Raspy, hoarse voice oSurvey of Mental Status and Speech . Apraxia: Loss of purposeful movement without o Cranial Nerves paralysis (Broca’s) o Motor System - Cranial Nerves o Sensory System oNumber 1 (Olfactory) o Reflexes . Assess patency of nasal passages o Special Maneuvers . Test each separately - Survey of Mental Status and Speech . Coffee, tobacco, soap oReflection of higher cerebral function Anosmia: Absence of sense of smell o(assess dress, grooming, hygiene, facial expression, oNumber 2 (Optic) mood) . Screen for visual acuity oAssess State of Consciousness . Inspect fundi . Alert-CNS function present and normal . Determine visual fields . Lethargic-CNS function present but slowed and with oNumber 3 (Oculomotor) moderately reduced content oNumber 4 (Troclear) . Stunorous-CNS function present but minimal (i.e., oNumber 6 (Abducens) responds yes or no, follows simple commands) . Shape, size, equality of pupils . Coma-No higher cerebral function. Defensive . PERRLA responses present . Direct/Consensual reaction . Metacoma-Complete unresponsiveness . Accommodation: Process of maintaining clear vision oOther Terms as gaze shifts from distant to near . Confusion-Incoherence in thinking *3 Components . Delirium-State of confusion characterized by . Convergence of eyes hallucination or agitation. Suggests psychiatric . Pupil constriction disease. . Thickening of lens - Perform Basic Mental Status Examination - VISUAL FIELD ABNORMALITIES oOrientation-Person, Place, Time oHemianopsia: Blindness in one half of visual field. oAttention/Concentration – Serial 7’s oBitemporal Hemianopsia: Optic chiasm. Decussating oMemory-Remote, Recent, Immediate recall nasal fibers. oCalculation oHomonymous Hemianopsia: Optic tract post to chiasm. oJudgment/Insight Left/right determined by field of vision lost. - Survey Mental Status and Speech o“Cortical blindness” – Destruction or lesion of calcarine oSpeech cortex. . Aphasia-Inability to speak oAmaurosis fugax – Transient monocular blindness due to . Dysphasia-Uncertainty or error in choice of words vascular cause (thromoembolic) oTypes of aphasia . Other causes of monocular visual loss include: . Broca’s (nonfluent): Frontal lobe anterior to Muscae volitantes (“floaters”) face/tongue/mouth area of motor cortex. Vitreous hemorrhage . impaired repetition Glaucoma . comprehension intact Retinal detachment . usually right hemiplegia Papilledema oWernicke’s: Posterior portion of superior temporal gyrus Migraine . fluent Optic nerve lesion . comprehension poor - Number 3, 4, 6 (continued) . repetition poor oExtraocular movements (EOM) – 6 fields . usually no hemiplegia oPtosis – Oculomotor nerve oConduction: Above Sylvian fissure oNystagmus – Rhythmic oscillation of eyes . “fluent” aphasia . Analogous to tremor . intact comprehension . Vertical, Horizontal, Rotary . poor repetition . Causes – Impairment of vision in early life oSpeech (other terms to describe abnormalities) . Labyrinthine or cerebellar disorders . Dysarthria: Inability to articulate due to motor defect . Drug toxicity involving lips or tongue (Broca’s) . Nystagmus described by direction of fast component . Aphonia/Dysphonia: Due to disease of larynx or its - Number 5 (Trigeminal) has two components: innervation oMotor-Temporal/Masseter: test symmetry and strength
38 CDM II Written Exam 2, 2010 MT
oSensory – Pain oArms held tight to sides w/fingers flexed . Light touch oLegs extended . Dull/sharp Decerebrate rigidity . Hot/cold (test tube) oJaws clenched, forarms extended . Corneal-approach from side - Screening tests - Number 7 (Facial) has two components: oGait oLook for asymmetry oObserve posture, movement of arms & legs, balance; . (raise eyebrows, frown, smile, show teeth, puff out Heel to Toe walking poorly done with cerebellar disease cheeks) oRomberg oTaste . Patient stands with feet together and eyes open . Bell’s palsy LMN paralysis – Whole side affected . If loss of balance with eyes open , this suggests . Hemiparesis UMN lesion cerebellar disease or vestibular disease Muscles forehead/eyes (both sides brain) . If loss of balance with eyes closed only, this suggests Muscles lower face (one side of brain) loss of position sense. - Number 8 (Acoustic) Whispered voice, Weber/Rinne - Other Maneuvers o(Vestibular) Cold H2O calorics oHop in place on each foot - Number 9 (Glossopharyngeal) Soft palate elevation oShallow knee bend on one leg - Number 10 (Vagus) Gag reflex oWalk on toes or heels oHoarseness . These usually bring out gross motor abnormality - Number 11 (Spinal Accessory) Trapezius-Shrug shoulders - More sensitive exam requires one or more of the following oSCM-Turn head oAssess muscle strength and muscle size - Number 12 (Hypoglossal) Protrusion of tongue oHand grasp oAsymmetry oLimbs and trunk oDecreased mass - Grading Muscle strength - Motor System o0/5 No movement oReview Upper Motor Neuron (Corticospinal/Pyramidal) o1/5 Fasciculations /Twitches . Fibers originate in motor cortex o2/5 Movement with gravity . Most cross over in brainstem o3/5 Movement against gravity . Synapse with anterior horn cells o4/5 Diminished . Control fine, discrete, conscious movement o5/5 Normal oReview Lower Motor Neuron (Anterior Horn Cell) - Assess muscle tone . “Final Common Pathway” oTone refers to resistance to passive movement . Mediate transmission of impulse to muscle part of oIncreased tone – UMN lesions, Parkinson’s reflex arc oDecreased tone - LMN lesions . Modified by influences of Extrapyramidal tracts - Assess Coordination Motor pathways from cortex, basil ganglia . Cerebellar or decreased position sense brainstem and cord oHands – Rapid rhythmic alternating movements Maintains muscle tone, controls body movement . Touch each finger of hand . Modified by influences of Cerebellar System . Point to point testing Receives sensory motor input oLegs – Heel to shin coordinates muscular activity, maintains - Abnormalities of movement equilibrium and posture oFasciculations – Twitching movements of muscle oDistinction between UMN and LMN paralysis bundles. . UMN (Corticospinal) Paralysis . If with muscle atrophy, suggests LMN disease Muscle groups affected diffusely oTremor – Involuntary tremulous movement of rhythmic Never individual muscles nature Atrophy slight, due to disuse. . Rest – “Pill rolling” of Parkinson’s disease Spastically with hyperactive DTR . Postural – Hyperthyroid/Anxiety Extensor plantar reflex (Babinski) . Intention – Cerebellar ataxia No fascicular twitches oTic-Repetitive twitching of muscles (esp. face, trunk) . LMN (Spinomuscular) Paralysis oChorea – Involuntary movement of face, extremities Individual muscles affected . Rapid, jerking, irregular, unpredictable Atrophy pronounced . At rest or with movement Flaccidity/hypotonia with loss of DTR . (Sydenham’s chorea with rheumatic fever) Flexor reflex (or absent reflex) oAthetosis – Involuntary movement of face, extremities Fascicular twitches may be present . Slow, twisting, writhing Decorticate rigidity (near c. hemispheres) . At rest or with movement . (Cerebral palsy)
39 CDM II Written Exam 2, 2010 MT
oMyoclonus – Involuntary sudden rapid jerks oDermatomal . Faster than chorea o“Glove and Stocking” (peripheral neuropathy) . (May occur when falling asleep, myoclonic seizure, oPosterior column (loss of position, vibration, hiccup) stereognosis, two point discrimination) oAsterixis – Involuntary and brief loss of muscle tone in - Reflexes outstretched fingers or hands resulting in non-rhythmic oReflex Arc flapping of fingers or hands. Must watch for 1 to 2 . Tap on tendon minutes with arms forward, hands crocked up and Stretch spindle fingers outstretched. Peripheral (afferent) nerve . (Metabolic encephalopathy-Hepatic, Uremic) Posterior nerve root oTardive dyskinesia – Choreiform movements affecting Synapse with motor neuron primarily tongue, lips and face. Anterior horn cell . Grimacing, protrusion of tongue, opening/closing of Motor anterior (efferent) nerve mouth. (Psychotropic drugs, esp. phenothiazines) Neuromuscular junction - Sensory System . Muscle contraction oSensory Pathways - Reflex arc requires . Spinothalamic tracts (Pain, temperature, crude oIntact sensory nerve touch) Crosses over immediately after synapse with oFunctional synapse nerve second sensory nerve. oIntact motor nerve . Posterior column (Position, vibration, fine touch) oNeuromuscular junction Ascends immediately into medulla oCompetent muscle Synapses with second sensory nerve and crosses - Higher motor pathways may modify reflex activity over - Deep . All sensory nerves meet in thalamus where the oBiceps C-5,6 general quality of sensation is perceived (pleasant oTriceps C-7,8 vs. unpleasant) oRadial C-5,6 . Synapse with third group of neurons to sensory oPatellar L-2,3,4 cortex oAchilles (ankle) S-1,2 . Sensory Cortex - Superficial . Sensory testing rapidly fatigues the patient oAbdominal T-8-12 producing unreliable and inconsistent results oCremasteric L-1,2 oTouch – cotton swab, finger oPlantar flexion L-4,5 oPain – pinprick oAnal S-1,2 oThermal – Hot/Cold - Pathologic oPostural Sense/Position Sense/Proprioception – oBabinski “Complex” - Grading of Reflexes oVibratory Sense – “Simple” o4+ Hyperactive - Stereognosis: perceive the form of an object by using the sense of touch o3+ Brisker than average oCutaneous number writing o2+ Average/Normal oTwo point discrimination o1+ Diminished/Low normal . 1mm tip of tongue oNo response . 2-3mm lips - Assess symmetry of response . 3-5mm dorsum of hands - Indicate use of reinforcement . 4-7mm body surface - Special Maneuvers - Dermatomes oMeningeal Signs oC3 Front of Neck oFlexion of neck produces resistance or pain oC 6,7,8 Hand oBrudzinski’s oT4 Nipples . Flexion of neck—Flexion of hips/knees oT10 Umbilicus oKernig’s oL3 Knee . Flex leg at hip and knee then straighten knee . oS1 Heel Note resistance or pain - Need to distinguish types of sensory loss: oPositive test also in neck injury, disc disease or par
40 CDM II Written Exam 2, 2010 MT 8. Muscoloskeletal - Definitions oHeberden/Bouchard oSymmetry - History oSynovitis (DIP/PIP) - Surrounding tissue– oPain: when? where? oArthritis vs. Arthralgias - Exam – atrophy, nodules, skin oStiffness oMyalgias Inspection/Palpation oOsteoarthritis: nodules oSwelling oTendonitis – oRange of Motion oBoutonneire oRadicular distribution Tenosynovitis oSwelling/Tenderness/W oSwan Neck oTrauma – mechanism oBursitis armth/Erythema oFunction – ADL’s oTophi (Sodium Urate) oCrepitation
Ethics: Medical Errors – Feb. 1 st - Objectives 1) The changing nature of modern health care delivery 2) Various causes of medical errors 3) Strategies for reducing potential sources of error and increasing patient safety - An error is defined as: ofailure of a planned action to be completed as intended (error of execution) or ouse of a wrong plan to achieve an aim (error of planning) - To Err is Human oIOM landmark report: Kohn LT, Corrigan JM, Donaldon MS: To Err is Human: Building a Safer Health System. Washington DC: National Academy Press; 2000 oBetween 44,000 and 98,000 people die every year in the U.S. hospitals because of medical errors oMost studies focus on errors as a function of deficiencies in expertise and training oWhat is missing is the way in which clinicians in complex organizations experience errors in the context of daily clinical practice - Safety in Health Care Delivery oLiterature about differences between academic and non-teaching hospitals in regards to Preventable Adverse Events (PAEs) oMore data in the in-patient setting oPatient Safety Indicators( PSIs) developed by the Agency for Health Research and Quality (AHRQ) to identify patient safety problems using administrative data - Two Types of Failure 1) Active 3) Latent . Unsafe acts by those working at the point of . consequences of decisions of designers, production: those whose hands are on the managers, and policy-makers who operate at a controls when accidents occur distance from the point of production . Sharp end errors . blunt end . More visible . relate to shaping the systems in which humans 2) operate oExamples of latent (system) failures include: . the flawed design of the medication administration process . the process of assuring the correct matching of organs and donors . the process of side identification prior to medical procedures oEfforts to reduce med errors are most effective when they focus on preventing latent rather than active failures - Error Reduction oDesign reliable processes that are resistant to human errors in execution oPromote effective team functioning oAddress systematic factors that often underlie poorly defined processes: . lack of organizational leadership for safety . absence of a suitable organizational culture . failure to incorporate human factor knowledge into policy design
41 CDM II Written Exam 2, 2010 MT - How do Residents Assess their Errors? o1999 study involved 26 residents in a large teaching hospital oFew medication-related errors since institution had a computerized order entry system in place for several years oRespondents categorized their errors as errors of omission, diagnosis and treatment and commission oTwo factors cited as contributing to ‘mishaps’: . Practitioner’s knowledge . Communication Busy ER Hostile superior Practitioner’s interpersonal skills - How do Residents Assess their Errors? oAnalysis of “practitioner’s knowledge” really referred to practitioner’s awareness of certain pertinent information i.e. previous diagnoses/treatment or history issues that were not communicated effectively to the practitioner oCommunication failures of one kind or another were an associated or contributory factor in 91% of mishaps - Potential Sources of Medical Mishaps oNature of modern medical care: . shorter hospital stay . rapid turnover of acutely ill patients . residents provide most of frontline care especially at academic medical centers . complex investigation and coordination of care by many medical specialists . multiple handoffs at many points of care requiring effective communication oComplexity of modern administrative systems: . horizontal differentiation of labor . vertical divisions of hierarchy and power . different institutional attitudes regarding safe care, the likelihood that an error would be reported (incident reports) and the willingness to discuss potential safety issues openly oFailure of Communication . not simply due to faulty transmission and exchange of information . timeliness is key . use of appropriate medium for message or task . may result from a system’s culture where there is excessive concern about appearing incompetent, role conflicts and struggles with interpersonal powers - STICC: U.S Forest Service System - Situation: Here is what I think we have - Task: Here is what I think we should do - Intent: Here is why - Concern: Here is what we should keep our eyes on - Calibrate: Now talk to me. Tell me if you do not understand, cannot do it, or see something I do not. SMALL GROUP DISCUSSION & Reading - Active failures - Error-producing conditions oSlips: prescribe wrong med oWork environment oLapses: forgot to do something . Environment, staffing, workload oMistakes: lack of knowledge oTeam oViolations: unqualified med student write . Communication, supervision prescriptions oIndividual . Heath, morale, skills & knowledge Dosing, but pharmacists often correct (defences) oTask - . Protocols, not routine oPatient . Unhelpful, complex disease, language
42 CDM II Written Exam 2, 2010 MT Ethics: Informed Consent and Refusal of Care – Feb. 22 nd - Case: oDocumentation. o76 yo female with end-stage COPD - What is Decisional Capacity? The ability to make an oPresents with SOB, SaO2 85% authentic choice. oAppears competent oAbility to receive information oRefuses intubation oAbility to process and understand information oLater desaturates and becomes unresponsive. oAbility to deliberate - Informed Consent in Medicine: oAbility to make and articulate choices. oTerm coined in 1957 - CAPACITY IS: oDelineates relationship between physician an oDynamic authoritarian and patient as an autonomous agent oSituational oA fundamental right of patient autonomy. oTask-specific. - Patient Autonomy oAbility to make and carry out decisions about one’s - DETERMINATION OF CAPACITY life oRoutine communications and interactions oPatient knows his goals and values best oClinical judgment oFreedom to choose between alternative methods oStandardized tests (example: MMSE). of management, based on expected results. - Competence and Incompetence - Legal Foundations of Informed Consent oLegal: able to manage his or her affairs oBattery: intentional, nonconsensual, offensive oMedical: able to participate in decision-making touching of the patient by physician oGeneral (global) vs. specific competence oNegligence: failure to satisfy a professional oPhysicians must make individual assessments. standard of care. - Does the Patient Possess Adequate Decision-Making - Essential Elements of Informed Consent Capacity? oPatient Capacity oIs he able to receive information? oInformation oIs he able to process and understand information? oVoluntariness. oIs he able to deliberate regarding the choices? - Informed Consent in Medicine: Three Basic Types oIs he able to make and articulate choices? 1. Express: granting of authority to render - Mini-mental status examination treatment oORIENTATION 2. Implied: consent derived from the conduct of . What is the (year) (season) (date) (day) the involved parties (month)? 3. Consent implied in law: emergency treatment . Where are we? (state) (county) (town) for patients unable to give consent. (hospital) (floor) - Negligence in Informed Consent: oREGISTRATION oPhysician had a duty to disclose information . Name three objects and ask patient to repeat oPhysician breached that duty oATTENTION AND CALCULATION oPatient was harmed . Serial 7’s (one point for each correct up to 5) oHarm was the result of an undisclosed risk . Option: Spell “world” backwards oPatient would not have consented to the oRECALL treatment had he known of the risks. . Ask for the 3 objects repeated above - ED Obstacles to Informed Consent oLANGUAGE oNo prior existing physician-patient relationship . Name a pencil and watch. (2 points) oTime constraints . Repeat “no ifs, ands, or buts”. (1 point) oPatients may not choose facility, or physician . Follow a 3-stage command. (3 points) oPreservation of life and prevention of suffering are . Read and follow the command “Close your our primary goals. eyes”. (1 point) - Refusal of Medical Care . Write a sentence. (1 point) oPROCESS (not merely a signature) . Copy a design. (1 point) oDetermination of Capacity - oDelivery of Information oProvision of Appropriate Medical Care
43 CDM II Written Exam 2, 2010 MT - Factors Affecting Patient Capacity - Which of the following are emergencies allowing oMental capacity exception to informed consent? oDelirium oCardiac resuscitation oPain oIntubation oAnxiety oChest tube oConfusion oAdministration of blood for shock oDepression oLP oPharmaceutical/illicit drugs oArthrocentesis - When Capacity is Impaired oIV oIdentify advance directives or power of attorney - Case: documents o76 yo female with end-stage COPD oIdentify a surrogate decision maker oPresents with SOB, SaO2 80% oHonor patient-centered values oAppears competent oSubstituted judgment oRefuses intubation oBest interest. oLater desaturates and becomes unresponsive. - Exceptions to Informed Consent: - Case: oEmergencies o37 yo intoxicated female . Immediate intervention is necessary to prevent oForehead laceration death or serious harm oRefuses sutures . Delay to obtain consent could be harmful oRequests discharge. . Presumption that most patients would consent - Case: if given the time and choice. o24 yo pregnant patient, brought by EMS after oPatient unable to consent vaginal bleeding . Surrogate consent should be obtained when oHemodynamically stable possible oRequests discharge . Decisions should be based on patient’s - Case: treatment preferences o27 yo WF, HIV+, left AMA with central line in place . Alternatively, substituted judgment based on oHas been using line for IVDU patient’s preferences and values oRefuses removal of central line . Legal action may be sought to override - Case: surrogate decisions o37 yo male with an amputee fetish oPatient waiver of consent oAmputated own arm with self-constructed oPublic health requirements guillotine oTherapeutic privilege oCalled 911 because of bleeding - oRefused limb reattachment - Conclusions oAssess capacity in ALL patients oProvide information, including risks, alternatives, and patient’s right to a medical screening exam oProvide the best possible medical care oDocument essential elements. Small group reading & discussion - Incompetence: legal term (needs to be in court) - Capacity (clinical) = Competent (legal) - Emergency determination of capcity: balancing autonomy and beneficence oJustice: how decisions affect others oNonmaleficense: avoid harm oBeneficence: do good oDMC = Determination of Decision-making Capacity
44 CDM II Written Exam 2, 2010 MT
45