Effective Date: November 1, 1996 CT Birth to Three System Date Revised: July 1, 2016
Title: INSURANCE
Purpose: Birth to Three programs must work with the CT Birth to Three System to access insurance coverage for early intervention services listed on a child’s IFSP
Overview
The Birth to Three State Statute 17a-248g requires that programs assist in the billing of private insurance for Birth to Three Services. The Affordable Care Act (ACA) restricts the use of financial limits so insurance companies may equate these dollar limits to another unit of measure. The CT Birth to Three System has a contractor to process all direct service billing for children who are covered by commercial insurance coverage. Per their contract all Birth to Three programs are required to work with the billing contractor for the billing of private insurance except for assistive technology devices. Insurance Billing Requirements State statutes and regulations combined with this procedure ensure that the state meets the following requirements of the IDEA Part C Regulations: (1) the Connecticut Birth to Three System will not disclose any personally identifiable information for the purpose of billing commercial insurance or Medicaid without parental consent, (2) coverage for Birth to Three services will not decrease the available annual or lifetime limits for the child or family, (3) the state will not collect insurance plan co-pays or deductibles, (4) the total reimbursement from insurance and parent fees will not exceed the states cost for services, (5) in order to receive early intervention services, parents are not required to sign up for, or enroll in Medicaid or commercial health insurance programs and can withdraw consent to bill health insurance at any time, (6) enrollment in Birth to Three will not adversely affect the availability of health insurance to the child, the child’s parent or child’s family members, and (7) will not result in any increase in premiums or discontinuation of Medicaid or insurance benefits for the child or the child’s family. The parent is responsible for paying premiums.
Completing Insurance Information Forms
Once a family has signed the Insurance Information Form 1-3, the provider should place the original in the child’s file and ensure that the data system accurately reflects the insurance information including the policy number. It is especially important to indicate those children who are covered by Medicaid (also called HUSKY A) and their Medicaid number.
If someone has both commercial insurance and Medicaid, the commercial insurance is primary. Medicaid will pay for services not covered by the commercial plan. If a child is insured by Medicaid (even if it is secondary to a commercial plan), Medicaid can’t be Insurance page 2
“balance-billed” for Medicaid covered services provided by an enrolled provider. Select Commercial insurance as Yes in the data system and Medicaid as No until a new billing system is developed.
Most Connecticut insurance plans do not require that a copy of Form 1-3 be sent to them prior to or with the first claim, although this varies with each plan. The billing contractor will validate insurance policies based on the data entered into the Birth to Three data system (see attached flow chart). A report will indicate when more information is needed to validate the policy. Some plans may require prior authorization and the Birth to Three billing contractor will assist with notifying programs when this is true after a claim has been denied. If there is a need to submit additional information such as a copy of the evaluation, a copy of IFSP, or an updated contact note the billing contractor will notify the program directly.
Exceptions to State Statute on Insurance Billing Insurance plans that are not required to follow state mandates (plans that are self- funded by an employer, also called ERISA, non-mandated plans, or plans written by companies that do not sell health insurance in Connecticut) may not pay or, if they do, may apply payments for Connecticut Birth to Three services against the maximum annual or lifetime caps of the policy. The policy validation process completed by the billing contractor will confirm whether the family’s insurance plan falls under one of these categories. In that case, the program will have the family complete Form 1-3a.
Form 1-3a, Informed Consent to Bill Health Insurance Plans Exempt from State Insurance Mandates, ensures that families understand that their annual or lifetime caps may not be protected. If a family, whose plan does not follow the Connecticut Birth to Three insurance statute, does not authorize billing of their plan, the Birth to Three System will impose a monthly fee in addition to the monthly family cost participation fee. The additional fee will range from $8.00 to $75.00 a month depending on the family‘s reported annual income level. Families that do authorize billing of their insurance, knowing that it does not follow state laws regarding annual and lifetime caps, will not be charged any additional fee even if the family’s plan does not reimburse Birth to Three services. Because it is not always apparent which plans conform to the state statute, if a parent signed form 1-3 and the billing contractor discovered that the plan is exempt from state insurance mandates, the service coordinator should do the following: Explain the situation to the family and ask them if, knowing that their plan is exempt from state mandates, they wish to change their mind about allowing their insurance to be billed. If they wish to continue to allow the billing, they must sign Form 1-3a indicating that they understand the implications. If they choose not to have their plan billed then they complete a new Form 1-3 which indicates the amount of the additional monthly fee based on their reported annual income. The program must then change the information in the data system to indicate that the family will be charged the additional monthly fee. The family will not be asked to pay the higher amount retroactively. Consent to Bill Insurance and Family Cost Participation Insurance page 3
For families with annual incomes of $45,000 or more that do not authorize billing of their insurance (mandated and non-mandated alike), the Birth to Three System will impose a monthly fee in addition to the monthly family cost participation fee. The additional fee will range from $8.00 to $75.00 a month depending on the family‘s reported annual income level. (See the current system of payments for the detailed amounts.)
Commercial Insurance Billing Delivered services must be entered into the attendance section of the Birth to Three data system. The billing contractor will obtain insurance and attendance information directly from the data system for each child and file the claims on authorized services on a monthly basis. The billing contractor will determine if any additional information is needed when a claim has been denied. A program may receive the Explanation of Benefits (EOB) directly from the insurance company if the billing contractor cannot access the information electronically, if this happens the program should forward the EOB to the billing contractor. Most payments can be viewed from the billing contractor’s Birth to Three website.
When the insurance company pays a claim, the check or electronic transfer (ETF) will in most cases be sent directly to the Birth to Three program. The program will indicate on the monthly invoice the amount from the billing contractor’s report for the period from the 1st of the month to the last day of the month for the month prior to the invoice month. .
The program will deduct 100% of total receipts from the subtotal of Billable Services on the invoice.
The billing contractor will keep records for each child on claims filed and track payments (or denials) received back to each claim. The lead agency will monitor that the total amount received from insurance and parent contribution does not exceed the amount paid by the State of CT for that child. Any amount in excess of this total will be refunded to the family.
If in the course of the billing contractor submitting claims they identify a change in the family’s address, member or group number, they will be able to make those changes directly in the Birth to Three data system or will notify the program that information is needed A note in the data system will indicate the date of change and whether it was made by the program or the billing contractor. . In those cases where the change will affect the billing or family’s caps the billing contractor will notify the program that an updated Insurance Information (Form 1-3 or 1-3a) is required.
Insurance Reimbursement for Eligibility Evaluations The service coordinator must ask the family to give permission using Form 1-3 for the Connecticut Birth to Three System to bill insurance (commercial OR Medicaid) for evaluations as well as for IFSP services. This should be done at intake for new referrals. The service coordinator must review the form and the insurance billing process with the parent, with additional information Insurance page 4 about the family cost participation fees once the child has been determined to be eligible.
Most plans no longer require prior authorization for Connecticut Birth to Three insurance claims however the must secure prior authorizations required by an insurance company such as Tricare. In order to bill an insurance company for the evaluation of a non-eligible child, Form 1- 7a must be signed by the child’s physician. Insurance plans may be billed for more than one evaluation for children who have subsequent evaluations after being determined not eligible.
Insurance Billing for Children with Autism Spectrum Disorders
Services for children enrolled in the CT Birth to Three System who have been diagnosed with an autism spectrum disorder by a licensed physician, licensed psychologist or licensed clinical social worker, will be billed to insurance companies. The Birth to Three program is responsible for ensuring that the data system has the correct ICD-10 code to indicate autism (F84.00). This can be on the eligibility screen if the child enters the system with the diagnosis but must also be indicated for all children on the IFSP screen regardless of when the diagnosis is made.
Insurance Payments Received By Families
State law requires Connecticut insurance companies to reimburse for early intervention services provided by programs. If the reimbursement by the insurance company is received by the family, the family is obligated to reimburse the program.
The EOB will alert either the billing contractor or the program that a family has received an insurance check and has not reimbursed the program. In this instance, the billing contractor will notify the program and the Birth to Three Fiscal Office of the situation and the billing contractor will then bill the family for the amount they received directly from their insurance company.
If the family fails to pay and the amount equals at least three months of the parent’s cost participation fee, the billing contractor will notify the Birth to Three administration, who will then notify the program that, if the child is still enrolled in the Birth to Three System, direct services will be suspended until the family pays the full amount of the insurance receipts they received. If the family pays, the billing contractor will send the insurance amount to the program. .
Discounts Requested By Insurance Companies through Claims Processing Companies
Any forms received from claims processing companies (e.g. MultiPlan or OmniClaim) requesting the Birth to Three program to accept a discounted payment for Birth to Three claims, should be forwarded to the billing contractor within 2 business days of recipt. Insurance page 5
Flexible Spending Accounts Flexible Spending Accounts are sponsored by the parent’s employer. It allows the parent to set aside “pre-tax” dollars for medical expenses. The account is managed by the parent and can include an automatic withdrawal option. If the automatic withdrawal option is activated, any portion of the insurance claim not covered by the insurance carrier can then be withdrawn and either mailed to the provider processing the claim or directly to the family. The potential could be to totally deplete the flexible spending account prematurely or to accidentally charge the family for co-pays, deductibles or unreimbursed claims. Programs would be responsible for reimbursing families if this happens. The automatic withdrawal option should be discussed with the parent who could inquire about deactivating the option or at least be aware of the potential possibilities.
Health Savings Accounts or HSAs A Health Savings Account (HSA) is a special account owned by an individual used to pay for current and future medical expenses and are used in conjunction with a High Deductible Health Plan (HDHP).
The HSAs are a means by which a family or individual with a specific HDHP is allowed to set aside pre-tax money to cover the high deductible. When a claim is processed, the owner of the HSA is allowed to make the determination whether he or she want the claim to be paid out of the HSA or their own pocket. Some HSAs have automatic options that will pay the deductible portion of the claim which is not in line with the Birth to Three policy of not collecting the deductible from the family. This creates a problem in that the program is required to return the money if it is, in fact, paying the deductible. The Insurance Information Form 1-3 has a check box to indicate whether the family insurance plan has a Health Payment Account, however some families may not know if they have one. When it is clear that a family has an HSA the insurance billing contractor will notify Birth to Three program and the program will update the Birth to Three data system that same day. Services for families with HSAs will not be billed unless the parent signs Form 1-3HSA indicating that they have confirmed that their deductible has already been met and that Birth to Three services may now be billed.
In some cases the billing contractor cannot determine whether a family has an HSA so every effort should be made by programs to help the family explore this before services are provided and billed. This may mean calling the insurance company or sending an encrypted image of the card to the billing contractor to be sure.
PLEASE NOTE: This letter was originally written in April of 2004 and continues to be referenced for billing guidance. Updates have been made to reflect the current name of the Lead Agency and the rates that became effective on April 1, 2010; however additional updates to the language have not been made. Insurance page 6
Joint Letter from Dept. of Insurance and Dept. of Developmental Services
April 12, 2004 (original date of letter) To: Re: Health Insurance Coverage for Early Intervention Services
The State of Connecticut Insurance Department and Dept. of Developmental Services (DDS) have determined that guidance is necessary for carriers to comply with sections 38a- 490a and 38a-516a of the Connecticut General Statutes (C.G.S.) as amended by Public Act 03-3 of the June 30 Special Session for coverage of early intervention services provided as part of an individualized family service plan pursuant to section 17a-248e of the C.G.S. In Connecticut, these services are provided through a program referred to as the “Birth to Three” program administered by the Dept. of Developmental Services.
Early Intervention Services Pursuant to sections 38a-490a and 38a-516a of the C.G.S., early intervention services must be covered in all health insurance policies of the type specified in subdivisions (1), (2), (4), (11) and (12) of section 38a-469 of the C.G.S., but may be subject to any cost-sharing provisions of the contract or subscriber agreement. For purposes of this coverage, early intervention services include the services listed below. Such services do not include assistive technology devices and services or transportation and related costs, unless otherwise provided for within the policy or subscriber agreement. Audiology Family training, counseling and home visits Health services (only those necessary to enable a child to benefit from the other early intervention services during the time the child is receiving other early intervention services) Initial evaluation Medical services only for diagnostic or evaluation purposes Nursing services Nutrition services Occupational therapy Physical therapy Psychological services Service coordination Social work services Special instruction Speech-language pathology Vision services Such services are provided by entities contracted by the Connecticut Dept. of Developmental Services and must be covered if provided by any of the categories of qualified personnel listed below. Such qualified personnel do not include paraprofessionals or parent-to-parent support personnel. For purposes of this coverage, the entities will be considered participating providers for managed care plans, and benefits will be payable in accordance with the in network level of coverage. Audiologists Board certified behavior analysts and associate behavior analysts Insurance page 7
Early intervention associates with a BA in education, human services or a related area with a minimum of one year’s experience in working with infants and toddlers and credentialed by DDS as an infant toddler family specialist Family therapists Nurses Nutritionists Occupational therapists and certified occupational therapy assistants Orientation and mobility specialists Pediatricians and other physicians Physical therapists and registered physical therapy assistants Professional counselors Psychologists Social workers Speech and language pathologists Special educators, early childhood educators, teachers of the hearing or visually impaired
Claims
Prior to a claim submission, the contracted entity will forward the Initial Evaluation Form used for the Birth to Three program to the carrier to provide notification that a child is being evaluated for acceptance into the Birth to Three program. Birth to Three early intervention services, including the initial evaluation, are not subject to prior authorization by the carrier. If the child is accepted into the Birth to Three program as determined by the Dept. of Developmental Disabilities, the entity will forward the Individual Family Service Plan to the carrier. Claim submissions for the initial evaluation and any subsequent services for children accepted in the Birth to Three program will be stamped with the Birth to Three logo.
The entities that have contracted with DDS will bill third-party payors for early intervention services as defined above. In accordance with Public Act 03-3 of the June 30 Special session, each carrier must cover such early intervention services up to $3200 each year with a maximum of $9600 over a three year period. (Per Public Act 09-3 the maximum amount has been raised to $6,400 per year or $19,200 over the course of three years). The agencies have agreed to submit claims using the four HCPC codes described in the attachment along with the related ICD-9 codes and modifiers to identify the type of provider. The provider type modifiers are as follows: AH = clinical psychologist AJ = clinical social worker GN = services delivered under an outpatient speech language pathologist plan of care GO = services delivered under an outpatient occupational therapy plan of care GP = services delivered under an outpatient physical therapy plan of care HN = Bachelors degree level HO = Masters degree level TD = registered nurse
The fee schedule payable to the entities for early intervention services is set by the Dept. of Developmental Services and is updated periodically. The current fee schedule for each of the HCPC codes is listed below. If a carrier has a contractual arrangement with a specific Insurance page 8 entity, the fee payable will be the lesser of the contractual rate in the carrier’s provider contract or the fee schedule as set by the Dept. of Developmental Services.
The following rates took effect on April 1, 2010: HCPC code rate per 15 minute unit rate per hour
H2015 $ 28.82 $ 115.28
T1015 $ 24.18 $ 96.72
T1027 $ 10.81 $ 43.24
T1024 $19.33 $ 77.32 (per discipline)
Effective Date
All carriers are expected to accept the codes and follow the procedures outlined in this letter for claims incurred beginning April 1, 2010. Questions may be directed to Linda Goodman of the Dept. of Developmental Services at 860-418-6147 or Richard Fisher of the Insurance Department at 860-297-3934. Thank you for your cooperation regarding this important issue for Connecticut consumers. Sincerely,
Commissioner Commissioner Insurance Department Department of Developmental Services Insurance page 9
Attachment: Birth to Three Service Codes with modifiers HCPC Description: includes official HCPC descriptor in quotes Modifiers Code and then functional definition
H2015 “Comprehensive Community Support Services” AH, AJ, GN, GO, Child Visit GP, HN, A face-to-face meeting at the child and family’s home or HO, TD community-based sites such as child care or play groups with the child, the child’s caregiver, or both and professional staff members for the purpose of furthering the child’s developmental progress.
HCPC Description: includes official HCPC descriptor in quotes Modifiers Code and then functional definition
T1015 “Clinic Visit/Encounter, All inclusive” AH, AJ, GN, GO, Center-based Individual Visit GP, HN, A face-to-face meeting of the child, the child’s primary caregiver, HO, TD or both, with qualified professionals at a Birth to Three program’s site, for the purpose of furthering the child’s developmental progress.
T1027 “Family Training and Counseling for Child Development” AH, AJ, GN, GO, Parent-focused Group Session GP, HN, A face-to-face meeting of a group of children’s parents and HO, TD person filling the role of the parents with qualified professional(s) for the purpose of support and guidance.
T 1024 “Evaluation and treatment by an Integrated, Specialty Team AH, AJ, contract to provide coordinated care to multiple or severely GN, GO, handicapped children” GP, HN, HO, TD Initial Evaluation/Assessment A formal, multidisciplinary evaluation of a child’s developmental status and family situation, including but not limited to, measuring fine and gross motor skills, cognitive ability, communication skills, affect and temperament, self-care and feeding skills, socialization, family interaction, and social and economic support system available to the family.
Each child referred receives an initial evaluation. If the child is found eligible, it becomes an evaluation/assessment. A child found not-eligible may be re-evaluated after three months. Insurance page 10
Qualified Professional: means those persons who are qualified to provide services under this agreement as defined in sections A through G below. A Nurse, must be a currently licensed RN by the CT Dept. of Public Health B Occupational Therapist, must be a currently licensed Occupational Therapist by the CT Dept. of Public Health. Also includes Certified Occupational Therapy Assistants licensed by the CT Dept. of Public Health. C Physical Therapist, must be a currently licensed Physical Therapist by the CT Dept. of Public Health. Also includes Physical Therapy Assistants licensed by the CT Dept. of Public Health. D Psychologist, must be a currently licensed clinical psychologist by the CT Dept. of Public Health or must be a certified school psychologist, certified by the State Dept. of Education. E Social Worker must be a currently licensed clinical social worker by the CT Dept. of Public Health F Speech Language Pathologist, must be a currently licensed speech pathologist by the CT Dept. of Public Health G Related Field: Includes certified teachers, audiologists, Board Certified Behavior Analysts (MA level or BA Level), marriage and family therapists licensed by the Dept. of Public Health, professional counselors licensed by the Dept. of Public Health. Will use modifiers of bachelors or masters degree. Also includes Bachelor’s degree in education, human services, or related area and at least one year’s experience in working with infants and toddlers and credentialed by the Department of Mental Retardation as an Infant Toddler Family Specialist. Will use bachelors degree modifier.
Modifiers: AH = clinical psychologist AJ = clinical social worker GN = services delivered under an outpatient speech language pathologist plan of care GO = services delivered under an outpatient occupational therapy plan of care GP = services delivered under an outpatient physical therapy plan of care HN = Bachelors degree level HO = Masters degree level TD = RN
______References: Form 1-3 Insurance Information Form Form 1-3a, Informed Consent to Bill Health Insurance Plans Exempt from State Insurance Mandates Form 1-7, Physician’s Authorizing Statement and Signature for Diagnostic/Evaluation Services for Children not Found Eligible Form 1-7a, Physician’s Authorizing Statement and Signature for Diagnostic/Evaluation Services for Children eligible but not choosing services at this time Assistive Technology Procedure Payments to Programs Procedure 38a-516a and 38a-490a of the C.G.S. Section 17a-248-12 of the Regulations of CT State Agencies Public Act 09-3 Insurance page 11
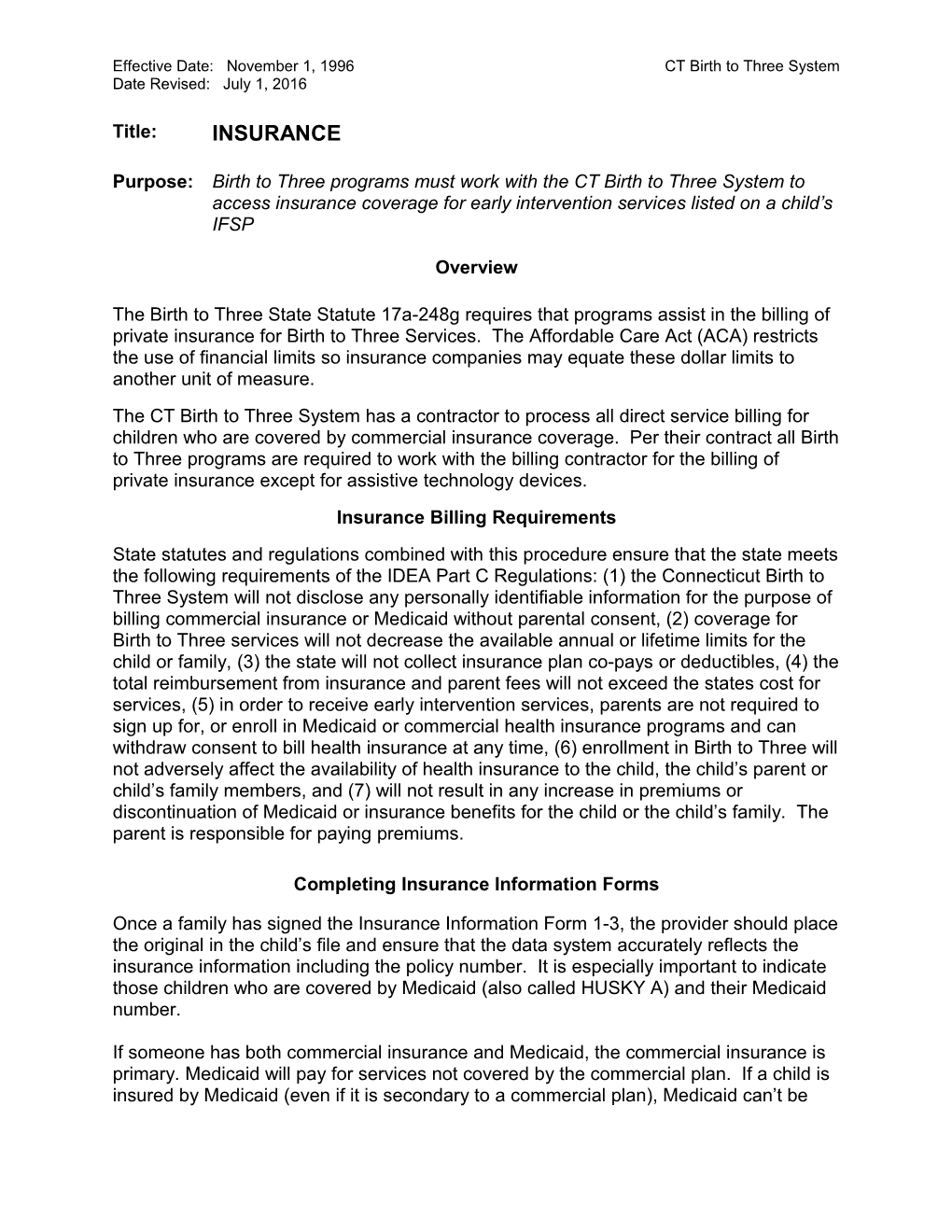
Insurance Policy Valid?
No Yes
Information Needed1
Data System Changed No Changes Needed Visits Submitted
Ins. Verified Indicator Set2 OK Denied3
Policy resubmitted $$$4
Insurance Policy Valid? Yes ICD10 / Prior HCPC Auth. Issue3 Needed3
No1
Corrected / Completed4 Insurance billing contractor to explore with carriers and EIS programs Visits resubmitted
OK 1) Billing contractor web portal report 2) CT Birth to Three data system 3) Billing contractor web portal report 4) Billing contractor web portal report $$$4