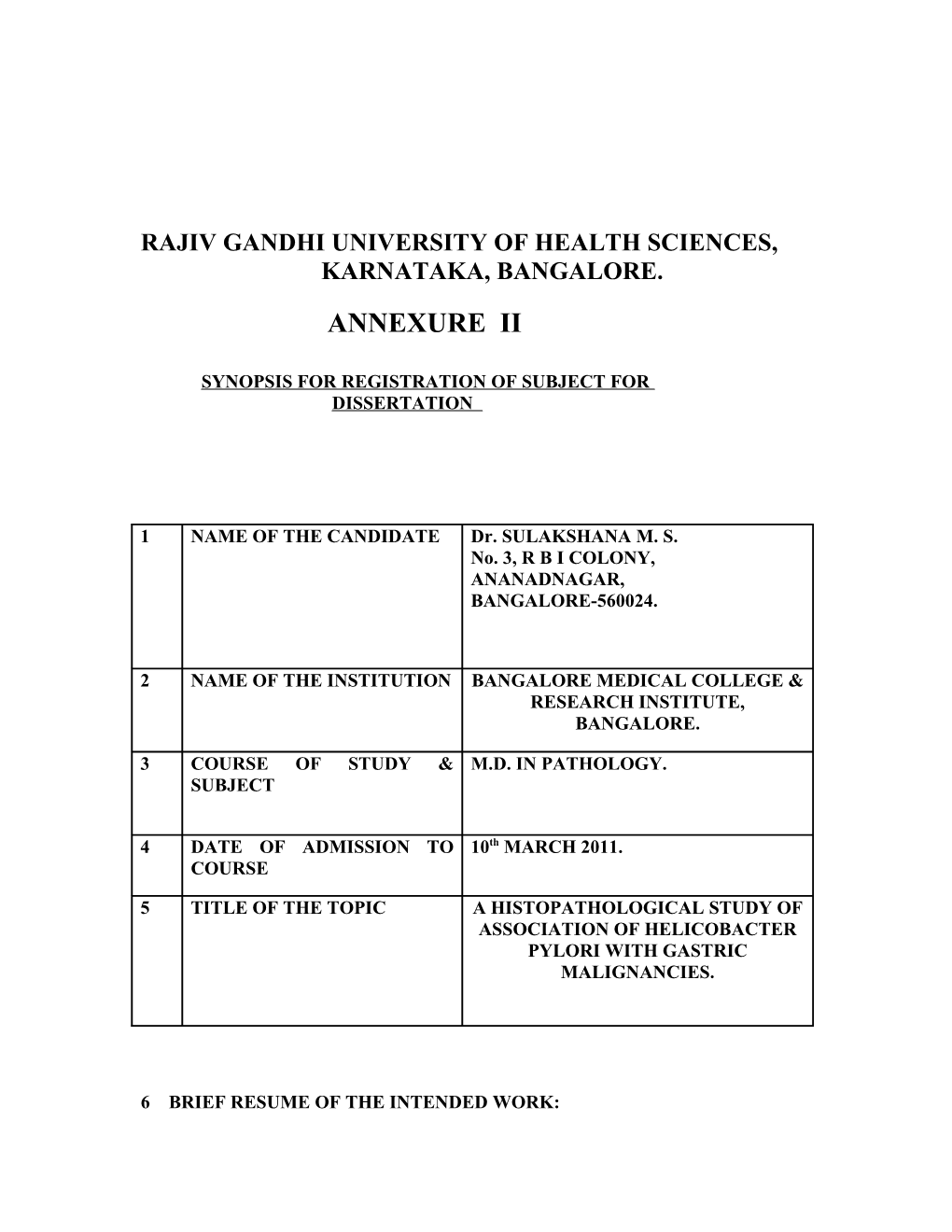
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES, KARNATAKA, BANGALORE.
ANNEXURE II
SYNOPSIS FOR REGISTRATION OF SUBJECT FOR DISSERTATION
1 NAME OF THE CANDIDATE Dr. SULAKSHANA M. S. No. 3, R B I COLONY, ANANADNAGAR, BANGALORE-560024.
2 NAME OF THE INSTITUTION BANGALORE MEDICAL COLLEGE & RESEARCH INSTITUTE, BANGALORE.
3 COURSE OF STUDY & M.D. IN PATHOLOGY. SUBJECT
4 DATE OF ADMISSION TO 10th MARCH 2011. COURSE
5 TITLE OF THE TOPIC A HISTOPATHOLOGICAL STUDY OF ASSOCIATION OF HELICOBACTER PYLORI WITH GASTRIC MALIGNANCIES.
6 BRIEF RESUME OF THE INTENDED WORK: 6.1) NEED FOR STUDY:
Helicobacter pylori, formerly known as Campylobacter pylori, is a curved spirochaete- like bacterium, of which two major genotypes exist. It is the most common cause of chronic gastritis. This organism colonizes the gastric mucosa (particularly the antrum and the cardia) in a variety of ways: free in the mucus, surface adhesion and intercellularly. Helicobacter pylori is known to cause pangastritis which is associated with multifocal mucosal atrophy, reduced acid secretion, intestinal metaplasia, and increased risk of gastric adenocarcinoma and lymphoma. H.pylori has now acquired the dubious distinction of being the first bacterium classified as a carcinogen.1
H.pylori has been found in 90 % of patients with chronic gastritis, 95 % with duodenal ulcer, 70 % with gastric ulcer, and 50 % with gastric malignancies.2
H.pylori can be recognized in routine Hematoxylin and Eosin stains. However, if the density of the organism is low, its detection can be greatly facilitated by the use of special stains like Giemsa, Warthin Starry or Steiner silver stains, the Alcian yellow-toluidine blue method, Genta stain and Triple stain.3 However, the detection of H.pylori by the fluorescent stain- Acridine orange is rapid and simple.
Hence, the present study will be done to know the association of Helicobacter pylori with gastric malignancies and also the sensitivity and specificity of detection of Helicobacter pylori by the use of special stains like Fluorescent stain- 0.01 % Acridine Orange.
6.2) REVIEW OF LITERATURE :
Gastric carcinoma is one of the most common forms of cancer, with approximately 900,000 new cases diagnosed every year and a leading cause of cancer-related deaths in many parts of the world.4 Significant advances toward the understanding of gastric carcinogenesis have been achieved since the description of Helicobacter pylori by Marshall and Warren, in 1984 5, and its later classification as a class I carcinogen (by the International Agency for Research on Cancer).6
Correa et al established that there was a high incidence of progression of Helicobacter pylori associated chronic gastritis to gastric carcinoma in Columbia.7
In 1998, Watanabe et al established that long-term infection with H. pylori generated adenocarcinoma in Mongolian gerbils.8 A long-term, prospective study in Japan by Uemura et al indicated that gastric adenocarcinoma developed in persons infected with H. pylori and not in uninfected persons.9 Kang et al in Korea established that there was a significantly increased risk for the development of gastric carcinoma among Helicobacter pylori carriers.9
A study in China by Forman et al has shown an unequivocal association between gastric cancer mortality rates and Helicobacter pylori infection rates.10
In a study done by Khanna et al in India, Helicobacter pylori was detected in 66% of patients with gastric cancer. 11
6.3) OBJECTIVES OF STUDY:
1) To study the association of Helicobacter pylori with Gastric malignancies.
2) To demonstrate Helicobacter pylori by the use of special stains.
7 ) MATERIALS AND METHODS:
7.1 : SOURCE OF DATA :
A histopathological study will be conducted on 100 biopsy specimens obtained by upper GI Endoscopy received by the Department of Pathology, Victoria Hospital,
Bowring and Lady Curzon Hospital, Bangalore from the Department of
Gastroenterology, Victoria Hospital, Bowring and Lady Curzon Hospital, Bangalore over a period of two years between November 2011 to May 2013.
7.2: METHODS OF COLLECTION OF DATA:
A) STUDY DESIGN:
Prospective study. B) STUDY PERIOD:
November 2011 to May 2013.
C) PLACE OF STUDY:
Department of Pathology, Victoria Hospital and Bowring and Lady Curzon Hospital,
Bangalore.
D) SAMPLE SIZE:
100 gastric biopsy specimens.
E) INCLUSION CRITERIA:
1) Informed consent is taken from all the patients included in the study.
2) Only those biopsy specimens which are received from the Department of
Gastroenterology, Victoria Hospital, Bowring and Lady Curzon Hospital, Bangalore and also those which are referred to the Department of Pathology, Victoria Hospital,
Bowring and Lady Curzon Hospital, Bangalore are included in the study.
3) All biopsy specimens obtained from malignant appearing lesions of the stomach on upper GI Endoscopy are included in the study.
F) EXCLUSION CRITERIA:
1) All biopsy specimens received from other sources other than from Department of
Gastroenterology, Victoria Hospital and Bowring and Lady Curzon Hospital, Bangalore are excluded from the study. 2) All biopsy specimens obtained from known cases of gastric malignancies are excluded from the study.
G) METHODOLOGY :
The biopsy specimens obtained by upper GI Endoscopy are fixed in 10 % aqueous formalin and Bouin’s fixative and subjected for tissue processing. The processed tissue is embedded in paraffin to obtain 3 micron thin serial sections. These sections are stained with routine Hematoxylin and Eosin stains and examined under the microscope for malignant neoplastic lesions. If malignant lesions are present, further evaluation for the presence of Helicobacter pylori is done in routine Hematoxylin and Eosin sections, and also by the use of special stains like Warthin-Starry stain, Giemsa stain, Triple stain, and Fluorescent stain 0.01 % Acridine Orange.
H) STATISTICAL ANALYSIS:
Descriptive statistics like Proportions, Sensitivity and Specificity, etc will be used as and when required.
7.3 DOES THE STUDY REQUIRE ANY INVESTIGATIONS OR INTERVENTIONS TO BE CONDUCTED ON PATIENTS OR OTHER HUMAN OR ANIMALS? IF SO DESCRIBE BRIEFLY.
Yes, Upper GI Endoscopy.
7.4 HAS THE ETHICAL CLEARANCE BEEN OBTAINED FROM YOUR INSTITUTION?
Yes.
8 LIST OF REFERENCES:
1) Stricker T, Kumar V. Robbins and Cotran Pathological Basis of Disease. In: Kumar V, Abbas AK, Fausto N, Aster JC, editors. 8th ed. Pennsylvania: Saunders Elsevier; 2010; Chapter 7, Neoplasia; pg 315-316.
2) Rosai J. Rosai and Ackerman’s Surgical Pathology. In: Rosai J, editor. 9th ed. Missouri: Elsevier Inc; 2009; Chapter 11, Gastrointestinal tract; pg 651-652.
3) Ghoussoub RA, Lachman MF. A Triple stain for the detection of Helicobacter pylori in gastric brushing cytology. Acta Cytol 1997 Jul-Aug; 41(4):1178-82.
4) Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics. CA Cancer J Clin. 2002; 55:74–108.
5) Marshall BJ, Warren JR. Unidentified curved bacilli in the stomach of patients with gastritis and peptic ulceration. Lancet. 1984; 1:1311–5.
6) IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Lyon, 7– 14 June 1994. Schistosomes, liver flukes and Helicobacter pylori. IARC Monogr Carcinog Risks Hum. 1994; 61:1–241.
7)Correa P et al. The role of Campylobacter pylori in gastro-duodenal disease. Progress in Surgical Pathology. 1989; 191-210.
8) Watanabe T, Tada M, Nagai H . Helicobacter pylori infection induces gastric cancer in Mongolian gerbils. Gastroenterology. 1998;115:642–8.
9) Kang HC, Chung IS. Helicobacter pylori infection and gastric adenocarcinoma in Korea: prevalence and distribution of Helicobacter pylori in resected specimen of gastric cancer. Korea Cathol Med Coll 1992;45:849-62.
10) Forman D, Sitas F, Newell DG, et al. Geographic association of Helicobacter pylori antibody prevalence and gastric cancer mortality in rural China. Int J Cancer 1990;46:608-11.
11) Khanna AK, Seth P, Nath G, Dixit VK, Kumar M. Correlation of Helicobacter pylori and gastric carcinoma. J Postgrad Med 2002;48:27.
9) SIGNATURE OF THE CANDIDATE :
(Dr. SULAKSHANA M. S.) 10) REMARKS OF THE GUIDE: Recommended for study.
11) NAME AND DESIGNATION OF :
11.1 GUIDE : Dr. SIDDIQUE M. AHMED, MD, Professor, Department of Pathology, Bangalore Medical College & Research Institute, Bangalore.
11.2 SIGNATURE:
11.3 CO-GUIDE: Dr. PARVESH KUMAR JAIN Assistant Professor, Department of Gastroenterology, Victoria Hospital, Bangalore.
11.4 SIGNATURE:
11.5 HEAD OF THE DEPARTMENT: Dr. A. R. RAGHUPATHI, M.D Professor and H.O.D, Department of Pathology, Bangalore Medical College & Research Institute, Bangalore.
11.6 SIGNATURE: 12) 12.1) REMARKS OF THE CHAIRMAN AND PRINCIPAL:
12.2) SIGNATURE: