Brian C. Toolan MD Orthopaedic Foot and Ankle Surgery The University of Chicago Section of Orthopaedic Surgery and Rehabilitation Medicine 5841 S. Maryland Ave. MC 3079 Chicago Illinois 60637 Phone 773.702.6984 Fax 773.702.0076
Achilles Tendonitis Treatment Options
Definition
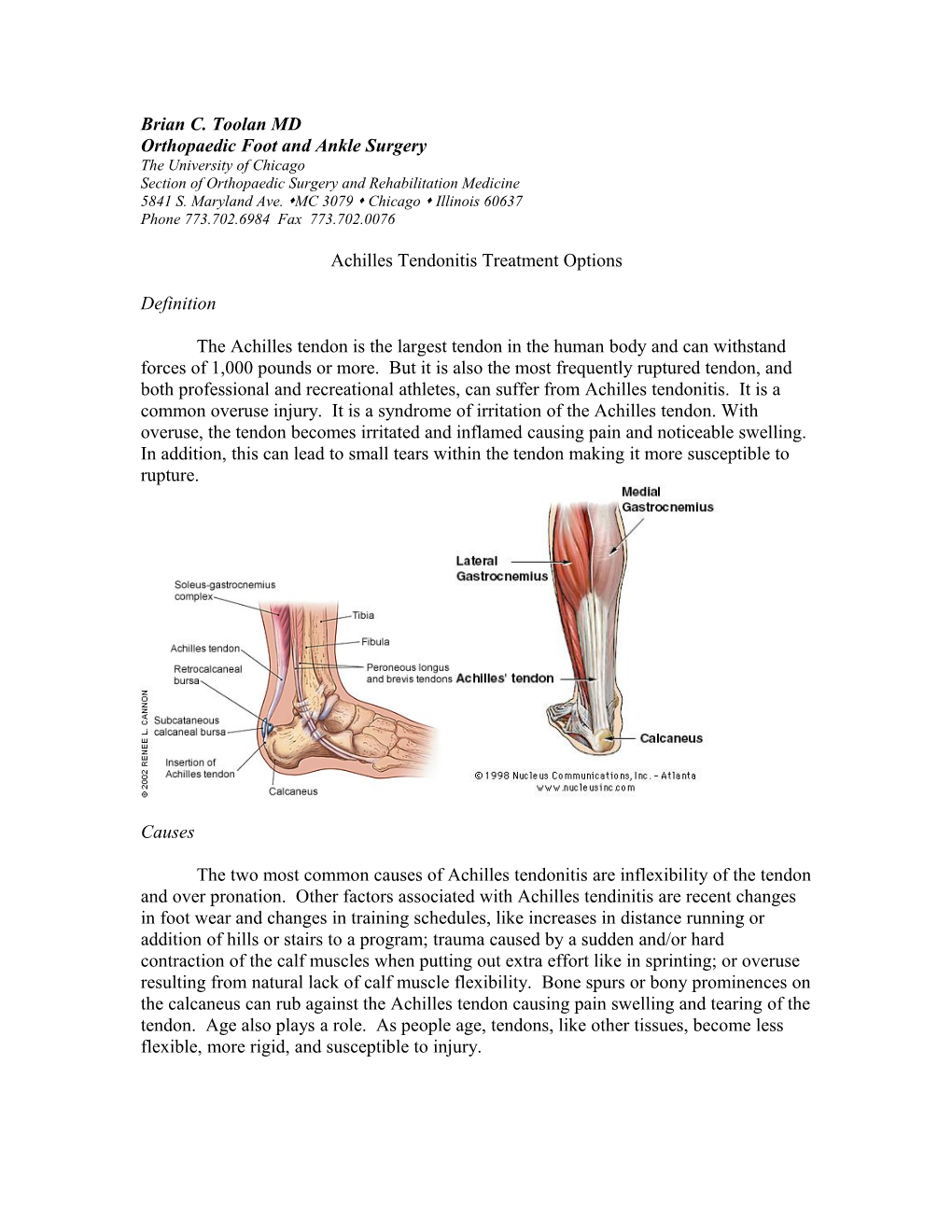
The Achilles tendon is the largest tendon in the human body and can withstand forces of 1,000 pounds or more. But it is also the most frequently ruptured tendon, and both professional and recreational athletes, can suffer from Achilles tendonitis. It is a common overuse injury. It is a syndrome of irritation of the Achilles tendon. With overuse, the tendon becomes irritated and inflamed causing pain and noticeable swelling. In addition, this can lead to small tears within the tendon making it more susceptible to rupture.
Causes
The two most common causes of Achilles tendonitis are inflexibility of the tendon and over pronation. Other factors associated with Achilles tendinitis are recent changes in foot wear and changes in training schedules, like increases in distance running or addition of hills or stairs to a program; trauma caused by a sudden and/or hard contraction of the calf muscles when putting out extra effort like in sprinting; or overuse resulting from natural lack of calf muscle flexibility. Bone spurs or bony prominences on the calcaneus can rub against the Achilles tendon causing pain swelling and tearing of the tendon. Age also plays a role. As people age, tendons, like other tissues, become less flexible, more rigid, and susceptible to injury. Symptoms
The main complaint associated with Achilles tendonitis is pain over the back of the heel. This is where the Achilles tendon attaches to the calcaneus (heel bone). Patients usually experience the most significant pain after periods of inactivity, for example, when first waking in the morning or when getting up after sitting for long periods. Pain will also be experienced with activity like running or walking, and the most severe pain is felt when pushing off or jumping.
Diagnosis
Diagnosis is made by patient history and physical exam. Sometimes the physician will request and MRI to asses for tears within the tendon or if surgical treatment is indicated.
Treatment
Treatment is dependent on the degree of injury to the tendon. Usually a period of rest, which may include limiting activity and/or immobilization for 3-4 weeks, is needed until the pain is resolved. Anti-inflammatory medications may also help. In addition, physical therapy and orthotics may benefit after immobilization. These conservative treatments are usually successful.
If conservative treatment is failed, surgery is an option of last resort. Surgery would involve removing the torn parts of the tendon and scar tissue, and repairing the tendon if necessary. Bone spurs may also require removal to reduce the chance of re- tearing the tendon. It requires four to six weeks of casting non-weight bearing to allow the tendon to heal followed by physical therapy to regain motion and strength.
Surgical repair of chronic Achilles tendonitis
The procedure generally involves making an upside down figure 7 incision in the back of your lower leg and repairing the torn tendon. There are the risks of having surgery which include infection, wound healing problems, and risks associated with having anesthesia.
The surgery takes approximately 90 minutes and can be performed on an outpatient basis, meaning you can go home the same day. The degenerated tendon is removed and repaired. If there is so much degeneration that the tendon cannot be repaired, sometimes you will have a tendon transfer. A tendon transfer entails taking another tendon and making it your new Achilles tendon. The tendon that is used is called the FHL tendon and its function is to bend the very tips of the lesser toes, but this function is not missed. Post operative management
There are many factors that affect your healing time. The most important is to be patient, YOUR FOOT MAY NOT TOUCH THE GROUND until your surgeon or therapist tell you that it’s o.k. This means you must use assistive devices, like crutches, a walker or roll-a-bout to get around. We do not want you to use a wheel chair because your entire body gets weak and it will lengthen your recovery time. Another factor is smoking. YOU MUST NOT SMOKE while you are recovering. It will delay your healing. This includes second hand smoke. Smoking decreases the blood flow to your surgical site. This means that oxygen and nutrients essential for healing are decreased and will lengthen your recovery. It is also possible that the tendon will not heal, or your wound will not heal and the skin dies. In the event that you do not heal, you will require additional surgery to get the tendon to heal. Another factor is swelling. This is something that can be avoided by elevating your foot above heart level. Swelling can also be controlled with ice therapy. Icing for 20-30 minutes in intervals will significantly decrease your swelling. The best thing to use for ice therapy is crushed ice or frozen vegetables because they can conform around your cast or splint. By eliminating swelling, you can reduce or eliminate your pain. Elevate and ice your foot 20-30 minutes for pain control first. If elevation and ice do not adequately control the pain, you may then take your pain medication. It is important to only take your pain medication when you need it. Just because the prescription says you may take it every 4-6 hours, does not mean that you have to.
Pain management The first 2-3 days after surgery will be the most uncomfortable. You will have both swelling and pain. During this time it is very important that you decrease your activity level, elevate the operated foot above heart level, and use ice therapy. You will notice when you put your foot down, it will begin to swell immediately and you will experience a throbbing pain, your toes my turn a dark bluish-purple. To treat this, elevate and ice and it should go away. Over the next two weeks, you will be able to increase the amount of time you can have your leg down. It is still important to keep your leg elevated as much as possible. After surgery, you will be given a prescription for pain medication. You should not need any refills. If you are out of pain medication, perhaps you are being too active and need to decrease your activity level. Before taking a pain pill, we suggest that you try elevation and ice for 20-30 minutes and if this fails to resolve you pain, you should take your pain medication.
Casting
Immediately after surgery, you will be placed into a splint. This is to help protect the surgical repair and allow for skin healing. It is like a cast, made of plaster and is open in the front to accommodate for swelling.
At two weeks after surgery you will return and have your sutures removed. You may desire to take some of you pain medication before having your sutures removed. You will be placed into a lighter-weight fiberglass cast for another 2 weeks. After your month of immobilization you will be placed into a CAM boot, a removable waking boot, so that you can start physical therapy.
Physical Therapy
Physical therapy begins at 4 weeks after surgery. The goals of rehabilitation are wound healing, range of motion with emphasis on neutral dorsiflexion, regaining muscle strength, normalize gain and return to previous functional level.
All exercises are done within the limits of pain. You will work on range of motion to 7- 10 degrees of dorsiflexion (bending your ankle toward your head) and full plantarflexion (bending your ankle down toward your toes. We do not want you to move your ankle past 7-10 degrees, so that you do not stretch out the repair and have difficulty with strength and gait. You may begin strengthening in plantarflexion only.
You will increase weight bearing directed by your therapist. First you will be off the crutches and then out of the CAM Boot. You will begin working on normalizing your gait. This process may take approximately 6 weeks to return to shoes, however, you will still work on strengthening and normalizing your gait for several months after surgery. Your goal will be to be able to perform a single heel rise.
It is important to remember that you may still have good and bad days after your treatment is completed. It can take six to nine months to return to your normal level of activity. Although there will be some bad days, over time you will get progressively better. We will see you back at the six month anniversary of your surgery. At six months, the foot should “feel normal”, range of motion is greatly improved, swelling is decreased and there are no problems with the foot with normal daily activities.
At any time during your treatment, you may call the office at (773) 702-6984 with any questions or concerns, or call the nurse at 773-834-0355.