Croup Guidelines – Nsambya Hospital
Croup (larynotracheal bronchitis) is an acute inflammatory condition that causes narrowing of the subglottic region of the larynx. It is usually caused by a viral infection, including (but not exclusively) parainfluenza, influenza, RSV.
Signs:
-Stridor -Barking cough -Hoarseness -Respiratory distress -+/- fever - +/- flu like illness
Where appropriate (if severity allows) a HANDS OFF APPROACH is best for initial assessment as patients can become very distressed with examination and symptoms worsen as a result.
Differential diagnosis:
Other causes of upper airway obstruction.
Main causes: -acute foreign body aspiration -acute anaphylaxis -bacterial upper airway infection (epiglottitis, bacterial tracheitis)
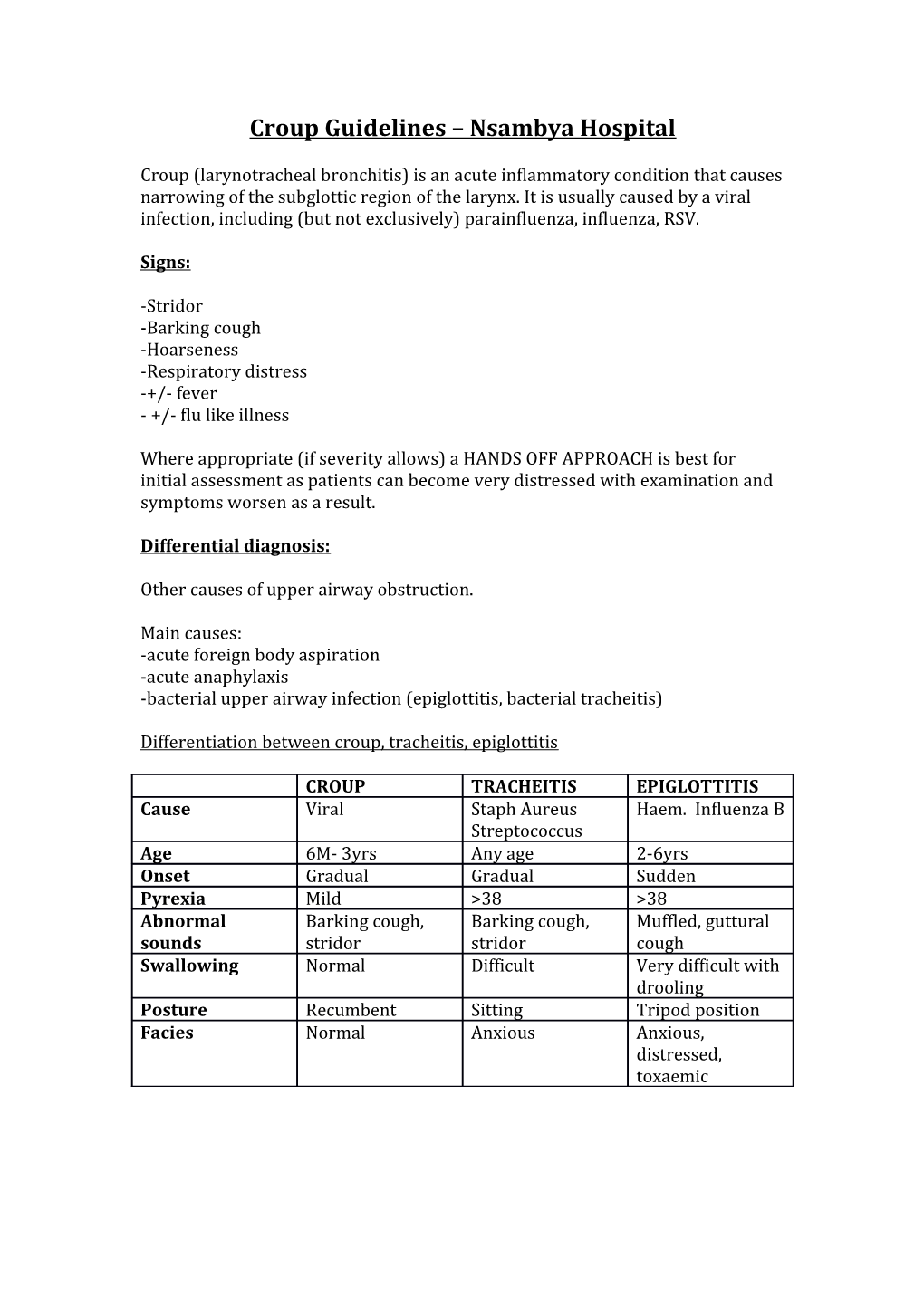
Differentiation between croup, tracheitis, epiglottitis
CROUP TRACHEITIS EPIGLOTTITIS Cause Viral Staph Aureus Haem. Influenza B Streptococcus Age 6M- 3yrs Any age 2-6yrs Onset Gradual Gradual Sudden Pyrexia Mild >38 >38 Abnormal Barking cough, Barking cough, Muffled, guttural sounds stridor stridor cough Swallowing Normal Difficult Very difficult with drooling Posture Recumbent Sitting Tripod position Facies Normal Anxious Anxious, distressed, toxaemic Bacterial tracheitis: infection of tracheal mucosa leading to copious secretions and mucosual necrosis. Child is usually ‘toxic’ looking, high temp, and requires IV antibiotics (usually cefotaxime and flucloxacillin).
Epiglottis is caused by haemophilus influenza B, and is intense swelling of epiglottis and surrounding tissues leading to airway obstruction. . Cough is usually minimal or absent. Child is toxic with a high fever and often drooling. IV cefotaxime and anaesthetic assessment of airway is needed, avoid unnecessary examination.
ASSESSING SEVERITY/SCORING:
Westley Croup scoring:
0 1 point 2 points 3 4 points 5 points points points Inspiratory Nil When At rest stridor agitated/active Intecostal Nil Mild Moderate Severe recessions Air entry Normal Mildly Severely decreased decreased Cyanosis None With At rest agitation/activity Level of Normal Altered consciousne s
<4 = Mild croup 4-6 = Moderate >6 = Severe croup
INVESTIGATIONS
CBC may be non specific. CXR: can exclude other causes if no improvement with initial management, or if suspicious of inhaled foreign body, epiglottitis,
May reveal ‘steeple sign’ – subglottal narrowing of airway. But CXR findings not specific, nor always present. TREATMENT
Mild
Oral dexamethasone single dose of 0.6mg/kg Can go home with croup advice (ie red flag signs of deterioration) Do not need a period of observation
Moderate
Oral dexamethasone single dose of 0.6mg/kg Observation needed for at least 2 hrs – home with advice if completely settled If worsening – nebulized adrenaline 2mls of 1:1000 and further observation needed Can use nebulized budesonide 2mg.
Severe
PO/IV dexamethasone 0.6mg/kg Oxygen by facemask/nasal cannula if child tolerates Nebulised adrenaline 2ml of 1:1000 to be repeated as often as every hour if needed but close monitoring required. Repeated nebulized budesonide if responsive Admission as inpatient. Close monitoring Consider anaesthetic review if deterioration and needing intubation/surgical airway
Antibiotics do not need to be routinely started, unless there is doubt as to diagnosis of croup (e.g. suspecting tracheitis/ epiglottitis) or poor response to initial therapy.
Supportive care:
Need to keep the child calm, avoid disturbance as much as possible. Encourage breastfeeding and oral fluids. Avoid IV fluids/cannula if not necessary as this can cause the child more distress and increase symptoms.
Dr Y Zhou Nov 2014.
References: WHO Hospital care for children 2013 edition NHS guidelines for management of croup www.patient.co.uk