www.Eye-Courses.com
Introduction: Motility refers to the movement and alignment of the eyes. If the eyes are not aligned with each other and do not move in sync with each other than we would say that the patient has a motility problem and double vision may result.
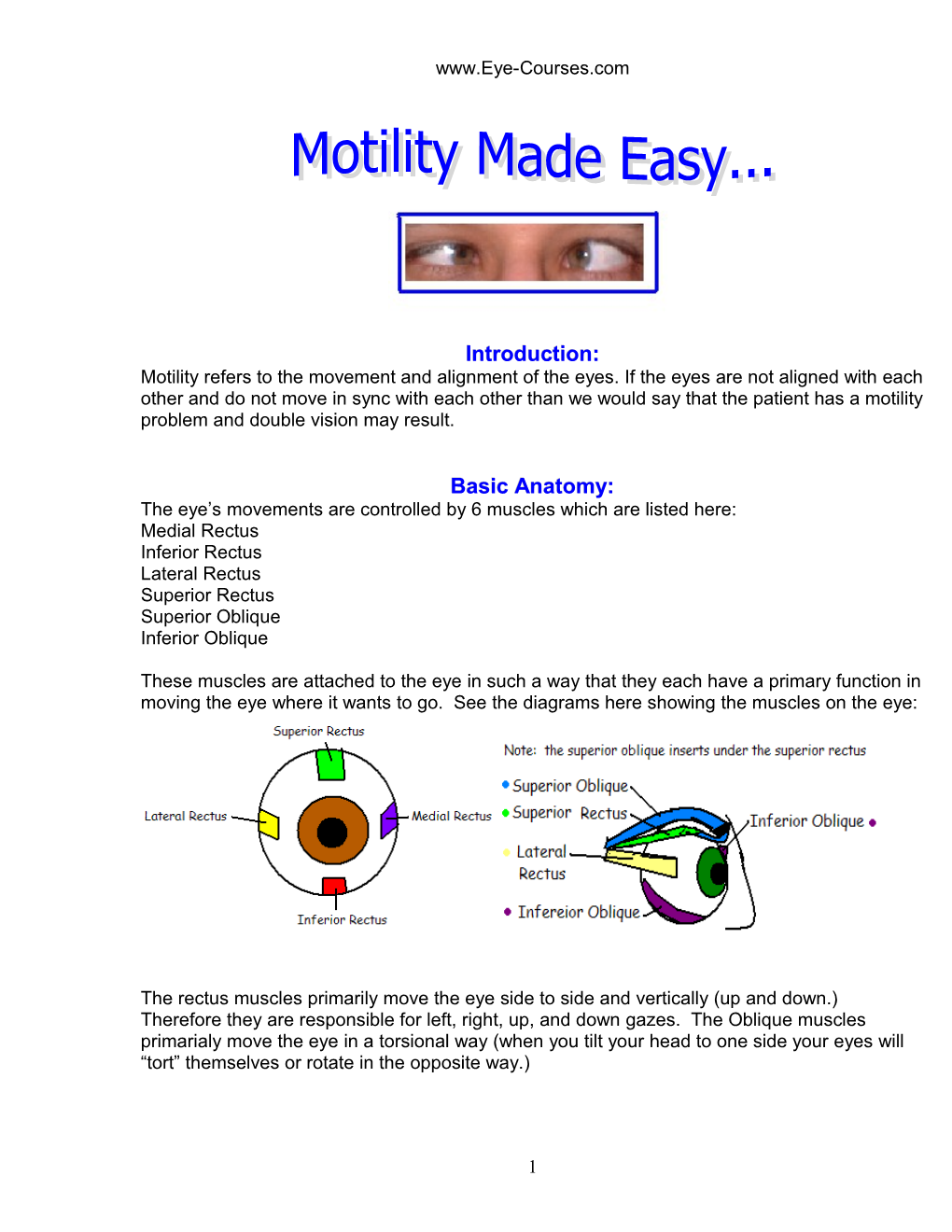
Basic Anatomy: The eye’s movements are controlled by 6 muscles which are listed here: Medial Rectus Inferior Rectus Lateral Rectus Superior Rectus Superior Oblique Inferior Oblique
These muscles are attached to the eye in such a way that they each have a primary function in moving the eye where it wants to go. See the diagrams here showing the muscles on the eye:
The rectus muscles primarily move the eye side to side and vertically (up and down.) Therefore they are responsible for left, right, up, and down gazes. The Oblique muscles primarialy move the eye in a torsional way (when you tilt your head to one side your eyes will “tort” themselves or rotate in the opposite way.)
1 www.Eye-Courses.com When a muscle contracts it pulls on the eye at its point of insertion on the eyeball. If the Medial rectus muscle contracts it will pull on the eye to move it in toward the nose. If the Lateral recuts muscle contracts it will pull on the eye to move it out away from the nose. See the diagram below:
The superior rectus muscle will turn the eye up if it contracts and the inferior rectus will turn the eye down if it contracts. See the following diagram:
2 www.Eye-Courses.com Ortho:
If a person’s muscles are all working properly then their eyes will be straight. We call this “Ortho”. Therefore a person with no motility problems is considered to be Ortho. Ortho is written like this: Ø A person who is ortho would look like this:
Eso:
If a person’s muscles are not working properly and they cause an eye to turn inward then we say the person has an Eso deviation. An eso deviation might look like this:
Exo:
If a person’s muscles are not working properly and they cause an eye to turn outward then we say the person has an Exo deviation. An exo deviation might look like this:
Hyper/ hypo:
If a person’s muscles are not working properly and they cause one eye to be higher than the other then we say the person has a hyper deviation (one eye being higher than the other). They would also have a hypo deviation (one eye being lower than the other). A hyper/hypo deviation might look like this (note that the right eye is higher than the left eye)
3 www.Eye-Courses.com
Tropia versus Phoria:
What is a tropia or a phoria??? Simply put, a Tropia is a deviation (eye turning) that you are able to see when the patient has both eyes open. We call this a manifest deviation because it manifests itself (in general) all the time. They may look like one of the pictures shown above, where one eye is turning with both eyes open and uncovered. A Phoria is a deviation (eye turning) that only shows up when an eye is covered, so you will never notice a phoria while the patient is sitting with both eyes open and uncovered. In a phoria the patient looks ortho with both eyes open and uncovered, but if you cover one eye (either eye) that eye will drift in, out, up, or down. If you uncover that eye it will go back to being straight. If you cover the other eye, that eye will drift in the same direction as the other eye did.
The prefixes described on the previous page (eso, exo, hyper, hypo) are combined with the suffixes -tropia or -phoria to describe what type of deviation the patient has. For example: Esotropia means that the patient has an eye that turns in even when both eyes are open.
Exotropia means that the patient has an eye that turns outward even when both eyes are open.
Hypertropia means that the patient has an eye that is higher than the other even when both eyes are open.
Esophoria means that the patient’s eyes will turn in when that eye is covered.
Exophoria means that the patient’s eyes will turn out when that eye is covered.
Units of Measure:
When we measure a deviation or turning of an eye (both a phoria and a tropia) we use a unitl of measure called the prism diopter (also called a diopter). We hold prisms up in front of the eyes to measure how far they turn and then notate it by the correct prism diopter amount that “fixes” the deviation. A diopter of prism will move the image the eye sees so that with the correct amount of prism diopters the eyes will become straight.
Ways to Measure:
There are several ways to measure how much an eye deviates. We will describe the methods here and give some pictures for examples.
Hircshberg method: This method uses only a pen light to measure the deviation. A patient is instructed to look directly at the pen light which you will hold up in front of them at about 1/3 of a meter away. You will then look at the corneal light reflexes in both eyes and compare them.
4 www.Eye-Courses.com If both reflexes are approximately centered in the pupil space the patient is said to be Ortho at near by Hirschberg (documented like this: Ø’ Hirschberg
If an eye is turned out (exo deviation) then the corneal light reflex in that eye will be IN compared to the other eye. See the diagram below:
If an eye is higher than the other (hyper deviation) then the corneal light reflex in that eye will be lower compared to the other eye:
To estimate the amount of prism diopters of deviation with Hirschberg you simply use the pupil and iris margins as a guide. See the diagram below with the corneal light reflexes demonstrating where the 30 diopter, 60 diopter, and 90 diopter marks would be. Note that the small triangle after each number is the mark indicating diopters.
5 www.Eye-Courses.com You would estimate the deviation amount based on the placement of the corneal light reflexes when the patient is looking straight ahead at your light. Notice that you will use the hash mark for near after your measurement as you are doing this measurement at near (1/3 meter). Note that this method is the least accurate of all methods but may be the only method you will be able to use on a very young child/baby. This method will not detect or measure a phoria, only a tropia can be measured by Hirschberg.
Krimsky Method: The Krimsky method is done in the same manner as the Hirschberg method using a pen light at near. The only difference in this method from the Hirschberg method is that to measure the deviation you will use actual prisms to center the deviated corneal light reflex. Most technicians doing this method will do Hirschberg first to estimate the amount of prism to start with. Once you pick a starting point you will hold that prism amount over one eye. Prisms are held so that the apex of the prism (the skinny end opposite the thickest end) is pointing in the direction of the deviation, (therefore if the patient has an eso deviation the apex of the prism will point nasally or in, just as the deviation is.) Instruct the patient to continue looking at your light. Look at the corneal reflexes, are they centered in both eyes? If not you will need to choose another prism. Which prism you choose next depends on whether or not your corneal light reflex is still deviated in the same direction as it initially was or if it now has changed and is deviated in the opposite direction. If you still have some deviation in the same direction as the initial direction you will need to go up in prism amounts until the reflexes both look centered while the patient is looking straight ahead at your light. If you hold up a prism that causes the corneal light reflex to deviate now in the opposite direction than you initially had, then you have too large of a prism and need to reduce the amount of prism you are holding up until the corneal light reflexes look centered in both eyes while the patient is looking straight ahead at your light. Note that this method is more accurate than the Hirschberg method but does require that the patient be able to fixate on your light and allow you to hold a prism in front of his/her eye, also this method only will measure a tropia, but does not detect or measure a phoria.
Cover Uncover / Cross cover: This method of measurement is the most accurate and will also allow you to detect and measure a phoria as well as a tropia. When measuring you will have the patient look at a line on the wall chart that you know they can see with each eye individually (but not a line so big that they may easily gloss over their eyes in a stare and still be able to see it easily) For example if the patient is 20/20 in each eye, I would suggest doing cover uncover / Cross cover with the 20/40 line. Then follow these simple steps: Cover Uncover: Instruct the patient to look at the line with both eyes open Look at both eyes to see if they appear straight or if one is obviously crossed in or out- note if there is crossing present initially and in which direction it is. Cover OD; look at OS while you cover OD. Does OS move? o If so, does it move in (from being out) – this would signal an exotropia (the left eye was turned out to start with and when you covered the right eye, the left eye had to move in to see the fixation target.) o Does it move out (from being in)- this would signal an esotropia (the left eye was turned in to start with and when you covered the right eye, the left eye had to move out to see the fixation target.) o If it does not move at all then it was straight to begin with. Uncover OD and watch OD while you uncover it, does it move?
6 www.Eye-Courses.com o If so, does it move in (from being out) – this would signal one of the following: . Exophoria: (OD drifted out under the cover but straightens up when the cover is removed.) You would not have noticed any movement of OS when OD was initially covered in this case. . Exotropia: If you also saw OS move in when you initially covered OD and then saw OD move in when you uncovered it you would have an exotropia. In this case the patient initially would have been fixating with OD, then moved to fixate with OS upon cover of OD, then moved again to fixate with OD upon uncovering OD. o Does it move out (from being in)- this would signal one of the following: . Esophoria: (OD drifted in under the cover but straightens up when the cover is removed.) You would not see movement of OS upon initial cover of OD. . Esotropia: If you also saw OS move out when you initially covered OD and then saw OD move out when you uncovered it you would have an esotropia. In this case the patient initially would have been fixating with OD, then moved to fixate with OS upon cover of OD, then moved again to fixate with OD upon uncovering OD. o If it does not move at all then it was either: . straight to begin with and stayed straight while covered (no phoria present) . it was crossed to begin with and is still crossed. Now cover OS and watch OD while you cover OS. Does OD move? o If it moves in (from being out) this signals an exotropia (you probably would not have seen any movement of OD when you covered and then uncovered it in the first step if there is an exotropia present, but you may or may not have seen OS move in when you covered OD in the first step.) o If it moves out (from being in) this signals an esotropia (you probably would not have seen any movement of OD when you covered and then uncovered it in the first step if there is an esotropia present, but you may or may not have seen OS move out when you covered OD in the first step.) o If it does not move then it is straight (note this does not necessarily mean the patient is ortho, just that at that time OD is straight. Now uncover OS and watch it while you uncover it. Does it move? o If it moves in (from being out) this signals one of the following: . Exophoria (if there was no movement of OD when you covered OS and you noticed that OD moved in when it was uncovered in the earlier step) . Exotropia: If you also noticed that OD moved out while OS is moving in (OS would be moving to pick up fixation and OD would be crossing out) and that OD moved in when OS was initially covered (OD moved in to pick up fixation). o If it moves out (from being in) this signals one of the following: . Esophoria (if there was no movement of OD when you covered OS and you noticed that OD moved out when it was uncovered in the earlier step) . Esotropia: If you also noticed that OD moved in while OS is moving out (OS would be moving to pick up fixation and OD would be crossing in) and that OD moved out when OS was initially covered (OD moved out to pick up fixation). o If it does not move this signals:
7 www.Eye-Courses.com . Ortho: If you saw no movement of any eye when covered, or uncovered; or when the other eye was covered or uncovered. . Esotropia: If OD moved out when OS was covered (it moved out to pick up fixation while OS is covered.) (NOTE: that OS is now turned in and is just staying turned in when the cover is removed.) . Exotropia: If OD moved in when OS was covered (it moved in to pick up fixation while OS is covered.) (NOTE: that OS is now turned out and is just staying turned out when the cover is removed.) Please note that the cover uncover test seems much more complicated than it is. You are actually looking at what each eye does when covered and when the fellow eye is covered to find out what it was doing before you covered an eye. You may need to cover uncover each eye several times before you discern what is going on, don’t be discouraged by that, it takes time to learn. Look over the following examples of cover uncover testing: Note that the cover will be shown such that you are able to see through it in these examples so that you are also able to see what happens to the covered eye.
8 www.Eye-Courses.com
Here is another example:
9 www.Eye-Courses.com
10 www.Eye-Courses.com And another example:
See the next example too:
11 www.Eye-Courses.com
Cross cover test The cross cover test is done after the cover uncover test has told you if the patient has a phoria or tropia. If you detect a phoria or tropia then you will want to measure it with the cross cover test and prisms. The test is performed using the same visual acuity line that you used to do the cover uncover test. Once you have determined if the patient has an eso, exo, or hyper deviation and whether it is a phoria or tropia you will start holding up prisms over an eye (either eye is fine) and move the cover from one eye to the next so that the eyes are not allowed to refuse by both being uncovered simultaneously. To estimate which power prism to start with you can perform the Krimsky or Hirschberg test first. Once you are proficient at motility you will have a good feel of what power prism to start with by seeing how much the eyes move on cover uncover testing. You will know that you have reached the correct
12 www.Eye-Courses.com measurement of the patient’s deviation when their eyes no longer move with the prism up on cross cover testing. If you do not have enough prism the eyes will still move in (for an exo deviation), out (for an eso deviation), or up and down (for a hyper deviation). If that is the case choose a larger prism and try again. If the eyes have switched the movement such that they were moving in but now are moving out, this tells you that you have to large of a prism power and you will need to reduce the power of the prism. If you do not see any movement on cross cover with a prism up, then that would be the measurement of the deviation. Prism placement: The way you hold the prisms is determined by the type of deviation present. The apex of the prism (the skinnier part) points in the direction of the deviation. The base of the prism the fatter part) points in the direction you want to move the eye to fix the deviation. Eso deviation: For an eso deviation you will point the apex of the prism toward the nose (or in since the eye is deviated in) Exo deviation: For an exo deviation you will point the apex of the prism out toward the ear (since the eye is deviated out). NOTE : for an eso or exo deviation you may hold the prism over either eye as long as you make sure that you are pointing it in the proper direction. Hyper deviation: For a hyper deviation you must make sure you hold the prism in the proper direction for the eye you are holding it over. When a patient has a hyper deviation one eye is higher(hyper) and the other is lower(hypo); (as opposed to an eso or exo deviation where the eyes both will go in or out respectively.) If holding the prism over the o Hyper eye: (or the higher eye) you will point the apex of the prism up (since the eye deviates up or is higher.) o Hypo eye: (or lower eye) you will point the apex of the prism down (since the eye deviates down or is lower.) Motility measurements should be taken with the patient looking at distance and near with the patient’s appropriate spectacle prescription on for each. Motility measurements should be noted in the chart like this:
This is the end of the Motility Made Easy course. For more in-depth information on checking motility please see our Motility Basics Simulation course.
13