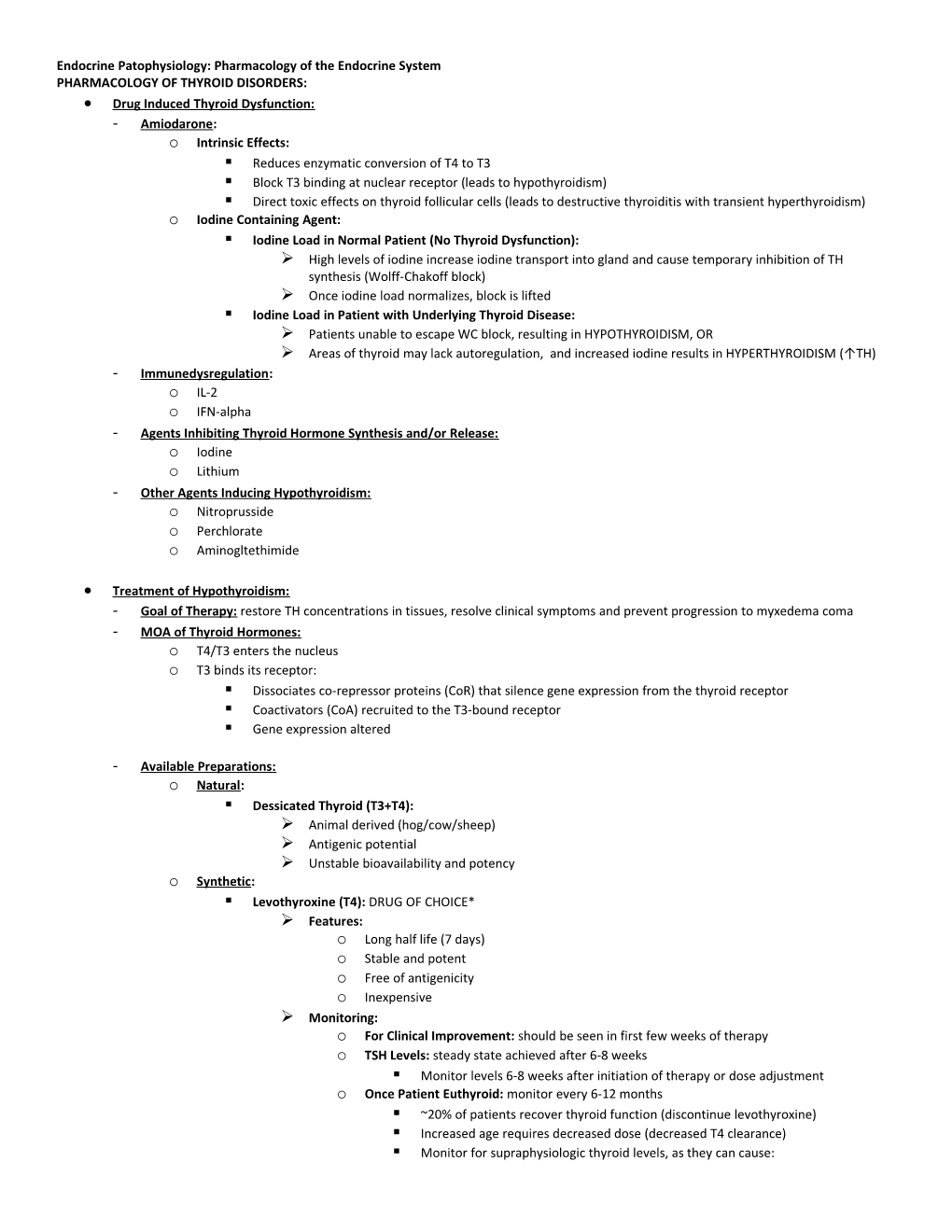
Endocrine Patophysiology: Pharmacology of the Endocrine System PHARMACOLOGY OF THYROID DISORDERS: Drug Induced Thyroid Dysfunction: - Amiodarone: o Intrinsic Effects: . Reduces enzymatic conversion of T4 to T3 . Block T3 binding at nuclear receptor (leads to hypothyroidism) . Direct toxic effects on thyroid follicular cells (leads to destructive thyroiditis with transient hyperthyroidism) o Iodine Containing Agent: . Iodine Load in Normal Patient (No Thyroid Dysfunction): High levels of iodine increase iodine transport into gland and cause temporary inhibition of TH synthesis (Wolff-Chakoff block) Once iodine load normalizes, block is lifted . Iodine Load in Patient with Underlying Thyroid Disease: Patients unable to escape WC block, resulting in HYPOTHYROIDISM, OR Areas of thyroid may lack autoregulation, and increased iodine results in HYPERTHYROIDISM (↑TH) - Immunedysregulation: o IL-2 o IFN-alpha - Agents Inhibiting Thyroid Hormone Synthesis and/or Release: o Iodine o Lithium - Other Agents Inducing Hypothyroidism: o Nitroprusside o Perchlorate o Aminogltethimide
Treatment of Hypothyroidism: - Goal of Therapy: restore TH concentrations in tissues, resolve clinical symptoms and prevent progression to myxedema coma - MOA of Thyroid Hormones: o T4/T3 enters the nucleus o T3 binds its receptor: . Dissociates co-repressor proteins (CoR) that silence gene expression from the thyroid receptor . Coactivators (CoA) recruited to the T3-bound receptor . Gene expression altered
- Available Preparations: o Natural: . Dessicated Thyroid (T3+T4): Animal derived (hog/cow/sheep) Antigenic potential Unstable bioavailability and potency o Synthetic: . Levothyroxine (T4): DRUG OF CHOICE* Features: o Long half life (7 days) o Stable and potent o Free of antigenicity o Inexpensive Monitoring: o For Clinical Improvement: should be seen in first few weeks of therapy o TSH Levels: steady state achieved after 6-8 weeks . Monitor levels 6-8 weeks after initiation of therapy or dose adjustment o Once Patient Euthyroid: monitor every 6-12 months . ~20% of patients recover thyroid function (discontinue levothyroxine) . Increased age requires decreased dose (decreased T4 clearance) . Monitor for supraphysiologic thyroid levels, as they can cause: Osteoporosis Cardiac toxicity, tachycardia, atrial arrhythmias Decreased exercise performance Increased risk of cardiac mortality Inability to Achieve Euthyroid State: o Compliance: be sure to check adherence o Dose Adjustment: may be required in some conditions . Pregnancy, malabsorption syndromes o Drug Interactions: assess for the presence of possible DDIs . Resin binders (cholestyramine, colestipol) . Aluminum containing preparations (AlOH3, sucralfate) . Enzyme inducers (phenytoin, phenobarbital, rifampin, carbamazepine) . Increased thyroid binding globulin (estrogen, raloxifene) Patient Counseling: o Take at the same time of the day every day o Take on an empty stomach (ie. in the morning before eating) o Do not take any of the following at the same time: . Iron products (ie. multivitamins, iron sulfate) . Calcium products (ie. dairy products, multivitamins, calcium carbonate . Liothyronine (T3): Short half life (1.5 days) Cardiac adverse effects High cost . Liotrix (T4 + T3): Expensive Lack of clinical rationale for use - Bioequivalence of Thyroxine Products: o Basics: FDA approved generics may differ from brands by up to 33% o Issue: narrow therapeutic index drug; slight dose alterations can lead to sub/supratherapeutic effects o Recommendations: . Maintain patients on the same levothyroxine product if possible . If it needs to be changed, check TSH in 6-8 weeks - Special Considerations in Hypothyroidism: o Subclinical Hypothyroidism: . Presentation: increased TSH and normal free T4 (asymptomatic) . Prevalence: 4.3% (progresses to overt hypothyroidism at a rate of 2-5% annually) . Therapy Considerations: No studies have shown that treatment decreases morbidity or mortality May result in development of subclinical HYPERthyroidism May result in symptomatic/laboratory improvements . Treatment: Serum TSH 5.4-10mIU/L: therapy not recommended unless patient is symptomatic o Monitor TFTs every 6-12 months in these patients Serum TSH >10mIU/L: levothyroxine therapy is reasonable o Myxedema Coma: end-stage of long-standing UNCORRECTED hypothyroidism . Mortality: 60-70% . Treatment: IV bolus of thyroxine (with maintenance doses until stabilized) IV hydrocortisone (until adrenal suppression ruled out) Supportive therapy (ventilation, restore euglycemia, BP, temperature) . Monitoring: Vital signs (should normalize within 24 hours) Consciousness TSH levels
Treatment of Hyperthyroidism: - Goal of Therapy: decrease excess thyroid hormone, minimize symptoms and decrease risk of thyroid storm - Anti-Thyroid Medications: o Thionamides: . Agents: Propylthiouracil (PTU) o Shorter half life o 60-80% protein bound o Hepatic metabolism Methimazole (MMI) o Longer half life o Not protein bound o Hepatic metabolism . Treatment of Choice for: Children and adolescents Grave’s disease (in uncomplicated young adults) Pregnancy Adjunctive therapy in severe cases or pre-operatively . MOA: Inhibits thyroid peroxidase Inhibits coupling of iodotyrosines Inhibits peripheral conversion of T4 to T3 (PTU only) . Duration of Treatment: 1-2 years Results in permanent remission in some cases (40-50%) Frequent relapses are common and may require a different treatment . Adverse Effects: Maculopapular Rash: o Variable onset o Resolves spontaneously o May treat symptomatically with antihistamines or prednisone (for severe cases) o May use alternate thionamide GI Intolerance: o Nausea Arthrlagis and Lupus Like Syndrome: o Seen after 6 MONTHS of treatment (later in treatment) Hepatotoxicity: o Seen within 3 MONTHS of starting treatment o Present with RUQ pain, anorexia, jaundice, hepatic necrosis and hepatitis o CANNOT switch to a different thionamide (cross-reactivity) Agranulocytosis: o Granulocytes <250/mm3 o Seen within 3 MONTHS of starting treatment (sudden onset) o Unexplained fever, malaise, sore throat, stomatitis and unusual bleeding or bruising . STOP THERAPY! o CANNOT switch to a differen thionamide (cross-reactivity) Benign Transient Leukopenia: o WBC <4,000 o Continue therapy and monitor WBC count - Radioactive Iodine: o Treatment of Choice for: . Toxic autonomous nodules . Multinodular goiters . Thionamide failure or adverse effects . Elderly patients . Patients with cardiac disease . Poor surgical candidates or patients who failed on surgery o Contraindications: . Pregnancy/breast feeding . Children o Preparations: . Sodium Iodide 131 Oral Solution: colorless and tasteless Easy administration, low cost, painless Effective (60% of patients euthryoid in 6 months; 2nd treatment at 6 months if results not achieved) o MOA: . Disrupts TH synthesis . Cellular necrosis and follicular breakdown . Edema and fibrosis of tissue o Adverse Effects: . Hypothyroidism . Transient increase in thyroid hormone levels (RAI causes initial release of stored TH) . Thyroid tenderness . Dysphagia o Monitoring: . TFTs every 3 months for the first year after RAI and then annually after that . Monitor for presence of hypothyroid symptoms o Patient Counseling: . Pregnancy is CONTRAINDICATED within 6-12 months post therapy o Pretreatment: . Beta Blockers: ALL patients (symptomatic relief, do not interfere with RAI) . Thionamides: used in select patients (withdraw 4-6 days before RAI) Patients with severe or long standing hyperthyroidism Elderly patients Patients with cardiac disease o Post-RAI Treatment: . May need to reinstate thionamide (4 days post RAI) . May use beta blockers . May use iodides - Surgery: o Treatment of Choice for: . Malignancy . Large thyroid gland (>80g) . Severe opthalmopathy . Lack of remission on thionamide treatment or contraindication to thionamide use . Pressure/obstructive/cosmetic symptoms o Outcomes: . Morbidity: 2.7% . Persistent Hyperthyroid: up to 17.9% o Adverse Effects: . Hypothyroidism . Hypoparathyroidism . Vocal cord abnormalities o Pretreatment: . Thionamides: use until patient is euthyroid (6-8 weeks) . Iodide Therapy: 10-14 days before surgery (decreases size and vascularity of thyroid gland) . Propanolol: several weeks pre-operatively o Post-Surgery Treatment: . Propanolol for 7-10 days post-operatively, OR . Propanolol + iodide for 10-14 days postoperatively - Adjunct Therapy: o Potassium Iodide: . Use: Preparation for surgery Severe thyrotoxicity with cardiac decompensation Psot-radiactive iodine treatment Patients exposed to radiological nuclear events (KI administered to bind the thyroid gland and prevent radioactive iodine from binding) . MOA: Acutely blocks thyroid hormone release Inhibits thyroid hormone synthesis Decreases size and vascularity of the gland . Preparations: Saturated solution (SSKI) Lugol’s solution . Adverse Effects: Hypersensitivity Swelling of salivary gland Iodism (metallic tasted, burning throat, sore teeth/gums) Gynecomastia o Adrenergic Antagonists: . Use: symptomatic treatment* Thyroiditis In combination with antithyroid medication In combination with RAI In preparation for surgery Thyroid storm . Agents Use: Beta Blockers: PROPANOLOL is the DOC o Controls symptoms (palpitations, tremor, anxiety, heat intolerance) o Inhibits peripheral conversion of T4 to T3 (small effect) Other Agents: used if BBs contraindicated o CCBs: verapamil, diltiazem o Centrally Acting Sympathomimetics: clonidine - Special Considerations in Hyperthyroidism: o Subclinical Hyperthyroidism: . Presentation: decreased TSH and normal free T4 (asymptomatic) . Cause: most often caused by levothyroxine therapy o Thyroid Storm: . Basics: severe thyrotoxicosis (medical emergency- mortality rate 100% without intervention) . Presentation: Fever, tachycardia, tachypnea, N/V/D, dehydration, delirium, coma . Precipitating Factors: Infection Trauma Surgery RAI treatment Antithyroid drug withdrawal . Treatment: decreases mortality to <7% Support vital functions (sedation, oxygenation, fluid/electrolytes, antipyretics, Abx, steroids) Block synthesis and release of THs (PTU, iodides) Inhibit metabolic effects (propanolol) Eliminate/correct precipitating factors Remove circulating hormones (dialysis, plasmapheresis)
FEMALE GONADAL PHARMACOLOGY: Estrogens: - Structure: 18-carbon backbone and contain a phenolic A ring (required for high affinity binding to estrogen receptor) - Naturally Occurring Estrogens: o 17-B Estradiol (E2): most potent, most abundant o Estrone (E1): 10x less biologically active than estradiol o Estriol (E3): synthesized by the placenta (present in high concentrations during pregnancy) - Synthesis of Estrogens: steroid hormone with cholesterol backbone o Premenopausal Women: ovarian aromatase converts androstenedione to estrogen (in follicular cells) o Postmenopausal Women: adrenal DHEA converted to estrogen by aromatase in adipocytes o Men: aromatase converts androstenedione to estrogens in adipose tissue; testes produce a small amount o Pregnancy: placenta produces a large amount of estriol - Pharmacology of Estradiol: o Tissue Distribtution: lipophilic and distributes rapidly to tissues o Bioavailability: readily absorbed in via the GI tract, skin and mucus membranes o Rapid Hepatic Metabolism: short half life when taken orally due to first pass effect . Hepatic metabolites renally eliminated or may undergo enterohepatic recirculation . Micronized estradiol allows for better bioavailability - Estrogen Derivatives (Synthetic): o Agents: . Ethinyl estrogen . Mestranol (demethylated in the liver to ethinyl estrogen) o Pharmacokinetics: . Bypass First Pass Effect: C17 modification inhibits first pass effect . Circulation: not bound to SHBG (free in circulation) . Release: slowly released from adipose tissue - Adverse Effects of Estrogen: o Postmenopausal bleeding (minimize dose, co-administer progestin) o Nausea o Breast tenderness o Hyperpigmentation o Migraine headaches o Cholestasis o Hypertension - Estrogen Risks: o Endometrial cancer o Breast cancer o CV outcomes (possible increased risk for primary CHD events, stroke/TIA, DVT) - Estrogen Benefits: o Decrease risk of hip or other fracture o Decrease risk of colorectal cancer - Estrogen Contraindications: o Estrogen dependent neoplasm o Undiagnosed genital bleeding (must first determine cause) o Hepatic disease (risk for cholestasis) o History of thromboembolic disorder (increased risk fo clots) o Pregnancy (category X) Progestins: - Synthesis of Progesterone: o Synthesized/secreted from corpus luteum during luteal phase of menstrual cycle (in response to LH surge) o If pregnancy/implantation occurs: . Initially, trophoblast secretes hCG to sustain corpus luteum and progesterone levels . After 8 weeks, placenta secretes estrogen and progesterone (no longer requires corpus luteum) - Synthetic Progestin: o Northeindrone o Medroxyprotesterone - Progestin Pharmacology: o Development of secretory endometrium during secretory phase of menstrual cycle o Secretion just prior to ovulation leads to 1 degree rise in body temperature o Maintenance of pregnancy (suppresses menstruation and uterine contractility) o Proliferation of mammary gland acini during pregnancy - Pharmacokinetics: o Rapidly absorbed orally o Large first pass effect (similar to estrogen) o Synthetic derivatives and micronized progesterone allow for better oral bioavailability Therapeutic Uses of Estrogen and Progesterone: - Hormone replacement therapy - Primary hypogonadism (stimulate secondary sex characteristics) - Dysmenorrhea - Endometriosis - Endometrial cancer - Prostate cancer - Contraception - PCOS Hormone Replacement Therapy: - Basics: o Estrogen used alone if NO uterus present (ie. hysterectomy) o Estrogen + progesterone if uterus present (due to increased risk for endometrial hyperplasia) - Use: o Relieve moderate to severe menopausal symptoms (hot flashes, sweating, atrophic vaginitis, sexual dysfunction) o Reduce bone resorption/osteoporosis prevention (only used for osteoporosis if also treating menopausal symtpoms) . Does NOT restore bone loss (only preventative) . May be considered in patients with high risk of osteoporosis (smokers, thin, Caucasian, sedentary, family Hx) - Drug Interactions: o Drugs Interfering with HRT: decreased efficacy of HRT . Rifampin . Anticonvulsants . Some antibiotics o HRT Interferes with Efficacy of Other Drugs: decreased efficacy of other drugs . Warfarine . Benzodiazepines . Thyroid agents . Metformin Polycystic Ovary Syndrome: - Basics: treatment revolves around symptoms and patient goals o Reduce androgenic symptoms o Weight loss (for obese patients) o Reduction of insulin levels o Address fertility goals - Goal of Therapy: early diagnosis and treatment may reverse some of the risks associated with PCOS - Lifestyle Modification: o Weight Loss . Regular aerobic exercise . Controlled eating patterns (carbohydrate, fat and calorie reduction) . Pharmacologic agents (ie. Orlistat) o Avoid Tobacco - Therapy for Androgen Excess: o Hair Removal (Hirsutism): . Mechanical hair removal . Eflornithine cream (inhibits ornithine decarboxylase to RETARD hair growth) o Oral Contraceptives: estrogen and progestin combination therapy . Estrogen: Decreases LH decreased androgen production Increases SHBG less free androgens . Progestin: need to use derivatives with the LEAST androgenic effects (norgestimate, desogestrel, drospirenone) . Benefits of OCP Use: Improve hirsutism and acne Protection against unopposed estrogen in the endometrium Induces withdrawal bleed . Concerns Regarding OCP Use: Insulin resistance Glucose intolerance Vascular reactivity and coagulability o Spironolactone: . MOA: inhibits androgen biosynthesis AND competitive inhibitor of the androgen receptor (large doses) . Use: synergistic effects with oral contraceptives Use if hirsutism or acne uncontrolled despite OCP therapy . Adverse Effects: Vaginal bleeding Hyperkalemia (K sparing diuretic) o Other Agents: . Flutamide: androgen receptor antagonist (limited use in PCOS) . Glucocorticoids: HPA axis suppression to decrease ACTH and androgen production (limited use due to SEs) . Finasteride: inhibition of type 2 5α-reductase enzyme (limited use in PCOS) - Endometrial Protection: o Why is it required? . Patients with PCOS suffer from CHRONIC ANOVULATION Increases risk for endometrial hyperplasia Increases risk of dysfunctional uterine bleeding Possible increase risk for endometrial cancer o Combined OCPs: . Progestin antagonizes endometrial proliferation (estrogen effect) . Requires a documented NEGATIVE pregnancy test before starting on OCP . If patient does not have menstrual period for >6 weeks: Give medroxyprogesterone daily for 10 days to induce withdrawal bleeding Minimizes breakthrough bleeding when starting OCP o Medroxyprogesterone Acetate: . Used when OCPs are contraindicated or patient does not want to go on them . Given every day for 7-10 days every 1-2 months Induces withdrawal bleed, offering endometrial protection . Does NOT reduce acne or hirsutism . Does NOT provide contraception o Metformin: . Restores menstrual cyclicity . Protective effects on endometrium not well established - Therapy for Induction of Ovulation: o Weight Loss: decreases serum testosterone, allowing for reduction of ovulation and pregnancy o Metformin: alone or in combo with clomiphene o Clomiphene: increases FSH and LH; 80% of PCOS women ovulate in response o Thiazolidinediones: rosiglitazone +/- clomiphene o Gonadotropin therapy - Therapy for Insulin Resistance: o Weight Loss: reduces insulin levels o Metformin: MAINSTAY OF THERAPY* . MOA: improves hepatic insulin sensitivity Decrease hepatic glucose output Decrease circulating insulin Decreased androgen production in the theca cells . Additional Benefits: Weight loss Decreased BP and LDL Improved ovulation Decreased rates of spontaneous miscarriage Decreased gestational diabetes o Thiazolidinediones: . Agents: rosiglitazone, pioglitazone . MOA: improves insulin sensitivity in adipose tissue, skeletal muscle and liver Improved glucose uptake Decreased circulating insulin Decreased androgen production in theca cells - AACE PCOS Recommendations: o Early recognition of the syndrome o Lifestyle modification o Measurement of glucose +/- insulin (consider OGTT) o Detect and treat lipid abnormalities o Monitor and treat BP if necessary o Measure atherogenic markers o Initial treatment with metformin (especially if overweight/obese) o Nonandrogenic OCPs for androgenic symptoms o TZDs for impaired glucose tolerance (IGT) or T2DM Fertility Pharmacology: - Goals: o Ovulation induction (to induce an anovulatory female to ovulate 1 follicle) o Superovulation (to induce multiple ova to mature and ovulate in a normally ovulating female, ↑ the chance of pregnancy) - Clomiphene Citrate: o MOA: competitive antagonist of the estrogen receptors in the hypothalamus . Hypothalamus detects hypoestrogen state and increase GnRH release . Pituitary stimulated to release 50-60% more FSH (results in follicular development) . Only effective in women with adequate estrogen levels o Administration: . Administered for 5 days early in the follicular phase (days 3-7 or 5-9) . Administered at this time because it is before the follicle dominance occurs, increasing the change of multiple follicle recruitment and maturation (increased FSH increased follicles) o Adverse Effects: . Antiestrogen effects (hot flashes, inhibition of endometrial proliferation) . Risk for multiple gestation . Ovarian cancer (controversial association) - Aromatase Inhibitors: o MOA: block conversion of androgen to estrogen . Decreases estrogen negative feedback to hypothalamus, increasing GnRH and FSH o Features: . Similar dosing regimen to clomiphene . No anti-estrogenic effect at the endometrium . More commonly used for estrogen-sensitivty malignancies - Gonadotropins: o Basics: injectable FSH and LH o FSH: administered once daily subQ for duration of follicular phase . May inhibit normal LH surge, resulting in need to exogenously produce LH surge . Derived from purified menopausal urine OR recombinant FSH o Mimic LH Surge with Injectable HCG: . Has a longer half life than exogenous LH . Stimulates ovulation and final maturation of ova (becomes fertilzable) Ovulation typically occurs 34-36 hours after hCG administration . Derived from pregnant women’s urine OR recombinant hCG o Effects: 8-15% chance of conception with each cycle . 20%, 5% triplets, risk for quadruplets or more o Monitoring: . Trans vaginal ultrasound (assess number of mature follicles) If too many, stop FSH and do NOT give hCG (cancel cycle) . Serum estradiol o Complications: . Ovarian Hyperstimulation Syndrome (OHSS): Seen in women given ovulation induction or superovulatory drugs Excess vasoactive substances released during follicle leutinization (esp. VEGF) o Increases capillary permeability (ascites, hypovolemia, hemooncentration) Occurs 5-10 days after ovulation trigger DIABETES MELLITUS PHARMACOLOGY: Sulfonylureas: - MOA: increase insulin secretion from beta cell (binds sulfonylurea receptor on islet cell, blocking the K+-ATP channel) o Blockage of K+ channel leads to depolarization and influx of Ca++ release of vesicles containing insulin - Use: o Relative insulinopenia (need to be able to make insulin) o Lean patients (may cause weight gain) - Onset of Action: full effects seen in 7-10 days (titrate dose after 1-2 weeks) - Efficacy: o Decrease HbA1c by 1-2% o Decrease blood glucose by 70mg/dl o Primary (never works) and secondary (diminished efficacy) failure both possible - Adverse Effects: o Hypoglycemia o Weight gain o GI effects o Hepatotoxicity o Hematologic effects o Skin rash (sulfa group- hypersensitivity) - Agents: o First Generation: . Chlorpropamide . Tolbutamide . Tolazamide o Second Generation: . Glipizide: 80-85% renally excreted, but excretion is of an INACTIVE metabolite Therefore, SAFE to use in renal insufficiency . Glyburide: 50% renally excreted, but excretion is of an ACTIVE metabolite Therefore, CANNOT use in renal insufficiency (increased risk for hypoglycemia) o Third Generation: . Glimepride - Drugs that INCREASE SU Effects: increased risk for hypoglycemia o Cimetidine o Alcohol o Warfarin o NSAIDs o Salicylates - Drugs the DECREASE SU Effects: o Rifampin o Diuertics o Beta blockers o Estrogens o Corticosteroids Biguanides (Metformin): - MOA: decreases hepatic gluconeogenesis AND reduces peripheral insulin resistance - Use: o Obesity + insulin resistance o Hypoglycemia due to SUs o PCOS - Onset of Action: see effect within days (titrate dose after 1-2 weeks) - Efficacy: o Decrease HbA1c by 1-2% o Decrease blood glucose by 60-80mg/dl - Other Benefits: o Decrease TG and LDL o Increase HDL - Adverse Effects: o GI effects (N/V/D, abdominal bloating) . Reason for dose titration o Lactic acidosis - Contraindications: due to risk for lactic acidosis o Renal impairment (SCr >1.5 in males or >1.4 in females) o Hepatic disease o CHF (increased production of lactic acid already due to hypoperfusion) o Alcohol use o Contrast media - Drug Interactions: o Drugs that INCREASE metformin effect (inhibit renal tubular secretion) . Furosemide . Cimetidine . Digoxin
Thiazolidinediones (TZDs): - MOA: decrease peripheral insulin resistance (binds to PPARγ to increase GLUT4 expression) - Use: o Insulin resistance o PCOS - Onset: effects in 2 weeks with maximum effects in 6-8 weeks (titrate dose after 6-12 weeks) o Longer onset than the other 2 classes discussed so far - Efficacy: o Decrease HbA1c by 0.5-1.5% o Decrease blood glucose by 50mg/dl - Adverse Effects: o Increase LFTs (contraindicated in patients with hepatic disease) o Edema o CHF exacerbation o Weight gain o Anemia o Avoluation o Myocardial ischemic events (black box warning) o Fracture - Agents: o Rosiglitazone o Pioglutazone: use more often Meglitinides: - MOA: increase insulin secretion when glucose exceeds threshold level o Do NOT release insulin in fasting state (glucose-dependent) o Otherwise, similar mechanism to sulfonylureas (but bind to different receptor) - Agents: o Repaglinide o Nateglinide (more raid and short-lived effects) - Use: o Relative insulinopenia (requires that patient can still make insulin endogenously) - Onset: effects are rapid (titrate dose after 1 week) - Efficacy: o Decrease HbA1c by 1-1.5% - Adverse Effects: o Hypoglycemia (less than sulfonylureas since glucose dependent) o Headache - Patient Counseling: must be taken with meals Alpha-Glucosidase Inhibitors: - MOA: slows the breakdown of complex CHO in the GI tract (slows absorption) - Agents: o Acarbose o Miglitol - Use: o Postprandial hyperglycemia o Patients with severe hypoglycemia from small doses of SUs - Onset: start with lose dose and titrate after 4-8 weeks - Efficacy: o Decrease HbA1c by 0.5-0.8% o Reduce postprandial glucose o Minimal effect on fasting plasma glucose - Adverse Effects: limit usefulness o GI effects o Flatulence - Patient Counseling: o Take with meals o Use glucose tablets for hypoglycemia (cannot digest complex carbohydrates) Other Agents: - Pramlintide: synthetic amylin analog o MOA: . Liver: regulates postprandial glucose . Alpha cells: decreases postprandial glucagon secretion . Stomach: slows gastric emptying . CNS: promotes satiety and reduces appetite o Use: T1DM or T2DM patients currently on insulin therapy (inject immediately before meals) o Efficacy: . Decreases HbA1c by 0.5-1% . 1-1.5kg weight loss o Adverse Effects: . Nausea . Hypoglycemia (especially in T1DM); need to reduce mealtime insulin by 50%* - Incretin Mimetics: o Agents: . Exenatide (BID or weekly injections) . Liraglutide (daily injections) o MOA mimic GLP-1 . Beta Cells: increase glucose dependant insulin secretion May also increase beta cell mass and proliferation (use early to slow progression?) . Alpha Cells: decrease glucose dependant glucagon secretion . Stomach: slows gastric emptying time . CNS: promotes satiety and reduces appetite o Use: T2DM, in combination with SU, metformin or TZD . Requires empiric SU dose reduction o Efficacy: . Decreases HbA1c by 0.5-1% . 1.5-3kg weight loss o Adverse Effects: . Nausea . Hypoglycemia . Pancreatitis o Contraindications: . Severe kidney disease . Gastroparesis . History of pancreatitis . Thyroid cancer or endocrine tumors - DPP-4 Inhibitors: o Agents: . Sitagliptin . Saxagliptin o MOA: inhibits DPP4 enzyme, prolonging GLP-1 action by inhibiting it’s inactivation o Uses: T2DM (either as monotherapy OR in combination with metformin or TZD) o Efficacy: decrease HbA1c by 0.7-1% o Adverse Effects: . URI/nasopharyngitis . Headache . Uritcaria . SJS (rare) o Important Points: . Dose adjust for renal function . Empiric SU dose reduction Insulin Therapy: - MOA: o Replaces defective insulin secretion o Suppresses hepatic glucose production o Increases glucose uptake by tissues - Indications: o T1DM o T2DM in certain scenarios . Acute stress, infections or surgery . Pregnancy . Renal or hepatic disease . Allergy to or failure of oral agents - Analog Insulins: modifications made to human insulin molecule to alter the pharmacokinetic profile o Peakless/Long Acting: last 20-24 hours . Glargine . Detemir o Rapid Acting Insulin: last 4-6 hours . Aspart . Lispro . Glulisine o Short Acting: last 6-10 hours . Regular insulin o Intermediate Acting: lasts 12-20 hours . NPH insulin - Basal/Bolus Therapy Regimen: best therapy because it mimics physiologic insulin release o Basal insulin administered before bed to provide peakless basal insulin levels throughout the day o Bolus insulin (rapid acting) injected before each meal to prevent postprandial spike - Factors Affecting Insulin Pharmacokinetics: o Site of injection o Depth of injection o Insulin concentration o Insulin dose o Insulin mixing o Exercise o Local heat or massage - Adverse Effects: o Hypoglycemia o Local skin reactions o Hypersensitivity o Lipodystrophy o Weight gain o Hyperinsulinemia Summary of Take Home Points: - T2DM: o Renal Insufficiency: . Metformin: contraindicated due to increased risk for lactic acidosis . Glyburide: contraindicated due to increase risk for hypoglycemia o CHF: . Metformin: contraindicated due to increased risk for lactic acidosis . TZDs: contraindicated due to increased edema and exacerbation of CHF o History of Hypoglycemia: use medications less likely to cause hypoglycemia . Metformin: does not increase insulin release . TZDs: do not increase insulin release - T1DM: o Insulin therapy is required (basal/bolus regimen the most effective)
MALE GONADAL PHARMACOLOGY: Uses of Androgens: - Hypogonadism - Male sexual dysfunction - Catabolic states - Athletic performance - Erythropoiesis stimulation Androgen Formulations: - 17α-Hydroxyl Group Esters: o Esterification makes the more lipophilic (oil preparations) o Hydrolyzed to testosterone in circulation o Administered IM every 1-2 weeks o Adverse Effects: . Cough (unclear mechanism) . Pain at injection site . Fluctuations in serum testosterone and symptoms - 17α-Alkylated Testosterone (Methyltestosterone): o Alkyl group retards hepatic metabolism, allowing for oral use o Less androgenic than testosterone o Associated with liver toxicity (not recommended for use) o Also difficult to monitor therapy (not easily detectable via immunoassay) - Transdermal Delivery: o Patch: applied to back, abdomen, upper arms or thighs . 2.5 or 5mg patches . Some adverse site reactions (rotate site or use hydrocortisone cream) o Gel: administer 5 gm of gel once daily . Allow gel to dry and cover with clothing . Do not come into contact with women/children . Better skin tolerability than patch - Buccal Testosterone (Striant): o Small tablet that adheres to the gums (becomes moistened and molds to it) o Testosterone absorbed through the gums into the bloodstream (bypasses liver metabolism) o Adverse effects include taste changes - Testosterone Pellets: o 3-6 pellets implanted subcutaneously (lasts up to 6 months) o Pellets may extrude spontaneously Monitoring Testosterone Therapy: - Serum Testosterone Levels: o Goal: 3-6 months after the initiation of therapy, testosterone should be in the middle of the normal range o Checking Serum Testosterone Levels: . Injectable: check midway between injections . Patch: check 3-12 hours after application . Buccal: check immediately before or after application . Gels: check anytime after the first week of therapy . Pellets: check at the end of the dosing interval (adjust the number of pellets/next dosing interval accordingly) - Hematocrit: o Check: . Baseline level . Levels at 3-6 months . Levels annually after that o Importance: discontinue if hematocrit >54% (reintroduce at a lower dose when it normalizes) - Bone Mineral Density: check after 1-2 years OR if osteoporosis or fracture occurs - Prostate Screening: o Baseline: PSA/DRE (for men >40 years old with PSA >0.6ng/ml) o Follow Up: at 3-6 months after initiating therapy, and then per cancer screening guidelines after that - Symptom Improvement: in 3-6 months and then annually o Sign/Symptom Improvement: . Increased libido . Improved erectile dysfunction . Improved fertility . Improved weakness, fatigue . Improved depression, loss of motivation, irritability . Increased body hair . Increased muscle ass . Increased size of prostate/testes . Reduction in gynecomastia . Improvement of osteoporosis . Improvement of anemia - Adverse Drug Reactions: in 3-6 months and then annually Contraindications to Testosterone Therapy: - Metastatic prostate cancer - Breast cancer - Unevaluated prostate nodule or induration - Elevated PSA >4ng/ml (or 3ng/ml is high risk- AA, first degree relative) - Hct >50% - Severe lower urinary tract symptoms with BPH - Uncontrolled CHF Adverse Effects of Testosterone Therapy: - Erythrocytosis (esp. if predisposed- COPD, chronic hypoxia) - Acne/oily skin (androgenic stimulation of sebaceous glands) - Detection of subclinical prostate cancer - Reduced sperm production/fertility (feedback inhibition of LH/FSH) - Induction/worsening of obstructive sleep apnea - Virilization in women and children (facial hair, hirsutism) - Initial growth spurt in children without epiphyseal closure, followed by premature closure and stunted growth - Aromatization of androgens to estrogen (gynecomastia) Anabolic Steroids: - Oxandrolone, Stanozol: o Only oxandrolone available in the US . HIV/AIDs wasting . Post-burn patients who have lost muscle mass o Greatest ratio of protein anabolic effects (ie. increase muscle mass) compared to virilizing effects - Androstenedione: o Weak natural androgen (synthesized by adrenal glands) o Converted to testosterone in tissues by 17-dehydrogenase o May aromatize to estrogen - Tetrahyrogestrinone (THG): o Newer anabolic that is metabolized quickly and more difficult to detect o ~20% of the potency to DHT o Toxicity profile is unknown - Danazol: o Derivative of 17α-ethinyl testosterone o Weak progestin and androgen activity o Used in the treatment of endometriosis (suppresses ovarian function- inhibits midcycle LH surge and FSH) - Side Effects of Anabolic Steroids: o No serious side effects with short term use o Long term use associated with several side effects . CV risk factors (decreased HDL, increased TG) . Hepatotoxicity (with oral anabolics) . Behavioral effects (increased aggressiveness, irritability) . Infertility Anti-Androgens: - Uses of Antiandrogens: o Female virilization o Alopecia o Precocious puberty o Prostate cancer o BPH o Paraphilia - GnRH Receptor Agonists: o Agents: . Leuprolide . Goserelin . Triptorelin (long acting, considered for use in paraphilia) o MOA: continuous stimulation of GnRH receptor causes downregulation . Because of mechanism, initially results in surge of testosterone - GnRH Receptor Antagonists: o Centrorelix: IVF protocols, inhibit premature LH surge (allows doctors to retrieve eggs before ovulation) o Ganirelix: IVF protocols, inhibit premature LH surge o Degarelix: prostate cancer o Abarelix: palliative care in prostate cancer (not available in the US) - Non Steroidal Androgen Receptor Antagonists: o Flutamide: used in prostate cancer . High incidence of hepatotoxicity . Associated with gynecomastia . Requires dosing every 8 hours o Bicalutamide: used in prostate cancer . Lower incidence of hepatotoxicity . Dosed once daily - 5α-Reductase Inhibitors: o Agents: . Finasteride . Dutasteride o MOA: block conversion of testosterone to DHT o Indications: . BPH (both agents) . Androgenic alopecia/male pattern baldness (finasteride only) o Adverse Effects: . Induces genital abnormalities in male fetus (avoid in pregnancy) . Decreased libido and sexual dysfunction - Other Antiandrogen Agents: o Ketoconazole: . Antifungal agent that inhibits glucocorticoids and androgen synthesis in the adrenal gland o Spironolactone: . Competitive androgen receptor angtagonist and K sparing diuretic . Used to treat hirsutism and PCOS