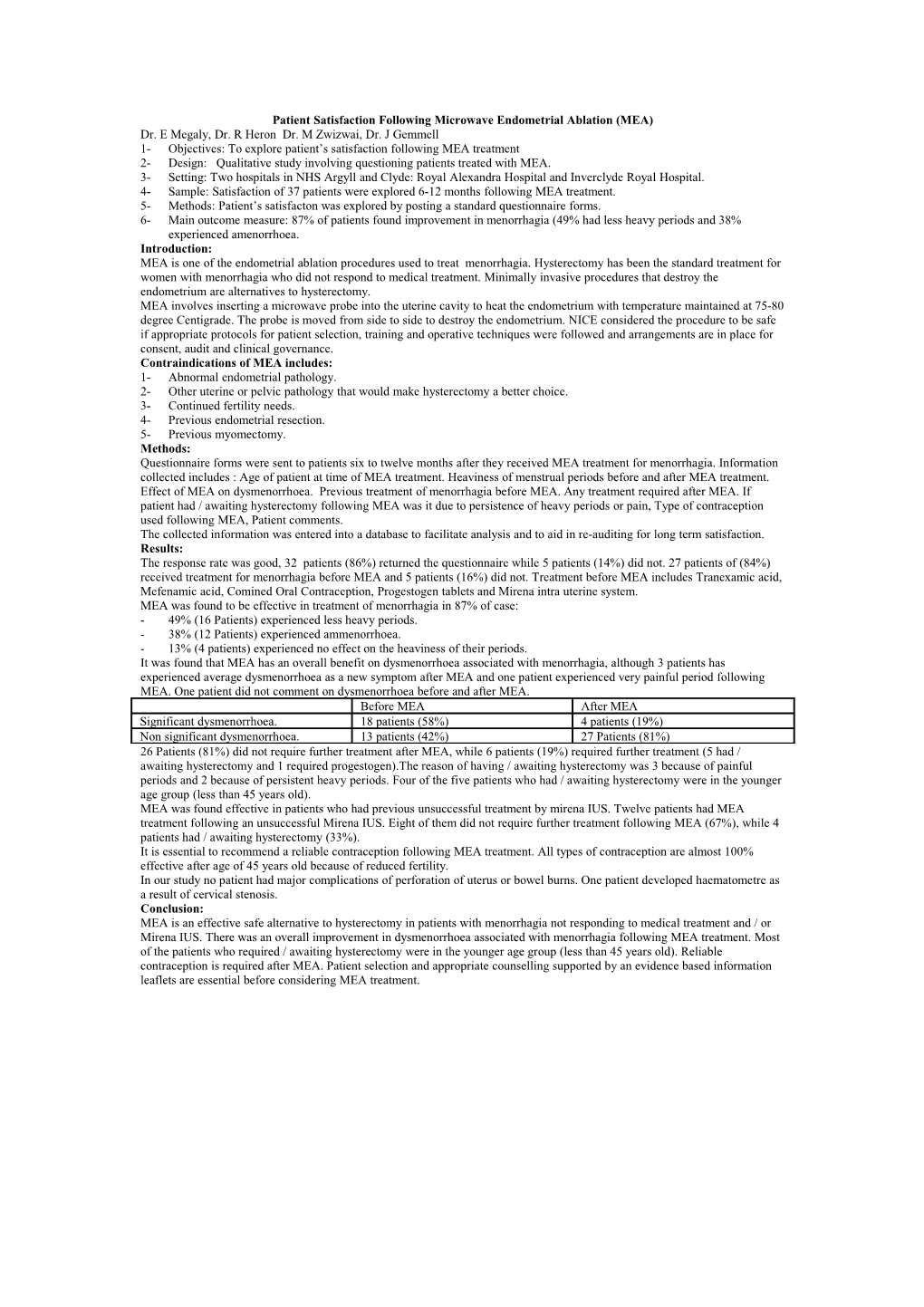
Patient Satisfaction Following Microwave Endometrial Ablation (MEA) Dr. E Megaly, Dr. R Heron Dr. M Zwizwai, Dr. J Gemmell 1- Objectives: To explore patient’s satisfaction following MEA treatment 2- Design: Qualitative study involving questioning patients treated with MEA. 3- Setting: Two hospitals in NHS Argyll and Clyde: Royal Alexandra Hospital and Inverclyde Royal Hospital. 4- Sample: Satisfaction of 37 patients were explored 6-12 months following MEA treatment. 5- Methods: Patient’s satisfacton was explored by posting a standard questionnaire forms. 6- Main outcome measure: 87% of patients found improvement in menorrhagia (49% had less heavy periods and 38% experienced amenorrhoea. Introduction: MEA is one of the endometrial ablation procedures used to treat menorrhagia. Hysterectomy has been the standard treatment for women with menorrhagia who did not respond to medical treatment. Minimally invasive procedures that destroy the endometrium are alternatives to hysterectomy. MEA involves inserting a microwave probe into the uterine cavity to heat the endometrium with temperature maintained at 75-80 degree Centigrade. The probe is moved from side to side to destroy the endometrium. NICE considered the procedure to be safe if appropriate protocols for patient selection, training and operative techniques were followed and arrangements are in place for consent, audit and clinical governance. Contraindications of MEA includes: 1- Abnormal endometrial pathology. 2- Other uterine or pelvic pathology that would make hysterectomy a better choice. 3- Continued fertility needs. 4- Previous endometrial resection. 5- Previous myomectomy. Methods: Questionnaire forms were sent to patients six to twelve months after they received MEA treatment for menorrhagia. Information collected includes : Age of patient at time of MEA treatment. Heaviness of menstrual periods before and after MEA treatment. Effect of MEA on dysmenorrhoea. Previous treatment of menorrhagia before MEA. Any treatment required after MEA. If patient had / awaiting hysterectomy following MEA was it due to persistence of heavy periods or pain, Type of contraception used following MEA, Patient comments. The collected information was entered into a database to facilitate analysis and to aid in re-auditing for long term satisfaction. Results: The response rate was good, 32 patients (86%) returned the questionnaire while 5 patients (14%) did not. 27 patients of (84%) received treatment for menorrhagia before MEA and 5 patients (16%) did not. Treatment before MEA includes Tranexamic acid, Mefenamic acid, Comined Oral Contraception, Progestogen tablets and Mirena intra uterine system. MEA was found to be effective in treatment of menorrhagia in 87% of case: - 49% (16 Patients) experienced less heavy periods. - 38% (12 Patients) experienced ammenorrhoea. - 13% (4 patients) experienced no effect on the heaviness of their periods. It was found that MEA has an overall benefit on dysmenorrhoea associated with menorrhagia, although 3 patients has experienced average dysmenorrhoea as a new symptom after MEA and one patient experienced very painful period following MEA. One patient did not comment on dysmenorrhoea before and after MEA. Before MEA After MEA Significant dysmenorrhoea. 18 patients (58%) 4 patients (19%) Non significant dysmenorrhoea. 13 patients (42%) 27 Patients (81%) 26 Patients (81%) did not require further treatment after MEA, while 6 patients (19%) required further treatment (5 had / awaiting hysterectomy and 1 required progestogen).The reason of having / awaiting hysterectomy was 3 because of painful periods and 2 because of persistent heavy periods. Four of the five patients who had / awaiting hysterectomy were in the younger age group (less than 45 years old). MEA was found effective in patients who had previous unsuccessful treatment by mirena IUS. Twelve patients had MEA treatment following an unsuccessful Mirena IUS. Eight of them did not require further treatment following MEA (67%), while 4 patients had / awaiting hysterectomy (33%). It is essential to recommend a reliable contraception following MEA treatment. All types of contraception are almost 100% effective after age of 45 years old because of reduced fertility. In our study no patient had major complications of perforation of uterus or bowel burns. One patient developed haematometre as a result of cervical stenosis. Conclusion: MEA is an effective safe alternative to hysterectomy in patients with menorrhagia not responding to medical treatment and / or Mirena IUS. There was an overall improvement in dysmenorrhoea associated with menorrhagia following MEA treatment. Most of the patients who required / awaiting hysterectomy were in the younger age group (less than 45 years old). Reliable contraception is required after MEA. Patient selection and appropriate counselling supported by an evidence based information leaflets are essential before considering MEA treatment.
Patient Satisfaction Following Microwave Endometrial Ablation
Total Page:16
File Type:pdf, Size:1020Kb
Recommended publications