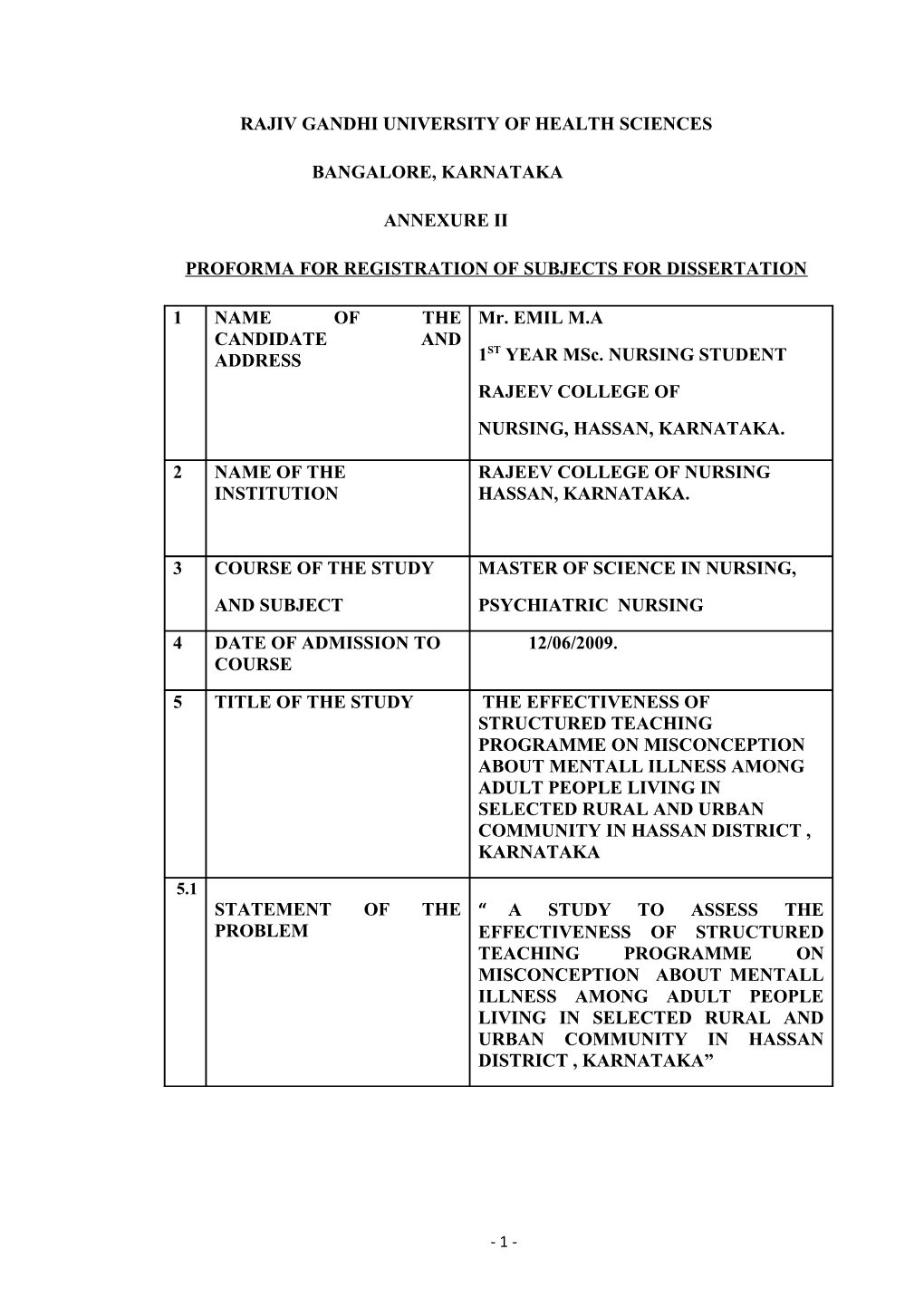
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES
BANGALORE, KARNATAKA
ANNEXURE II
PROFORMA FOR REGISTRATION OF SUBJECTS FOR DISSERTATION
1 NAME OF THE Mr. EMIL M.A CANDIDATE AND ST ADDRESS 1 YEAR MSc. NURSING STUDENT RAJEEV COLLEGE OF NURSING, HASSAN, KARNATAKA.
2 NAME OF THE RAJEEV COLLEGE OF NURSING INSTITUTION HASSAN, KARNATAKA.
3 COURSE OF THE STUDY MASTER OF SCIENCE IN NURSING, AND SUBJECT PSYCHIATRIC NURSING
4 DATE OF ADMISSION TO 12/06/2009. COURSE
5 TITLE OF THE STUDY THE EFFECTIVENESS OF STRUCTURED TEACHING PROGRAMME ON MISCONCEPTION ABOUT MENTALL ILLNESS AMONG ADULT PEOPLE LIVING IN SELECTED RURAL AND URBAN COMMUNITY IN HASSAN DISTRICT , KARNATAKA
5.1 STATEMENT OF THE “ A STUDY TO ASSESS THE PROBLEM EFFECTIVENESS OF STRUCTURED TEACHING PROGRAMME ON MISCONCEPTION ABOUT MENTALL ILLNESS AMONG ADULT PEOPLE LIVING IN SELECTED RURAL AND URBAN COMMUNITY IN HASSAN DISTRICT , KARNATAKA”
- 1 - 6. BRIEF RESUME OF THE INTENDED STUDY:
6.1) INTRODUCTION
“We are all born mad. Some remain so”. –Samuel Beckett
In most societies mental illness carries a substantial stigma, or mark of shame. The mentally ill are often blamed for bringing on their own illnesses, and others may see them as victims of bad fate, religious and moral transgression, or witchcraft. Such stigma may keep families from acknowledging that a family member is ill. Some families may hide or overprotect a member with mental illness keeping the person from receiving potentially effective care or they may reject the person from the family. When magnified from individuals to a whole society, such attitudes lead to under funding of mental health services and terribly inadequate care. In much of the world, even today, the mentally ill are chained, caged, or hospitalized in filthy, brutal institutions. Yet attitudes toward mental illness have improved in many areas, especially owing to health education and advocacy for the mentally ill.
Many mentally ill people are the victims of stigma and misconceptions, which leads to additional suffering and humiliation. Negative stereotypes and prejudicial attitudes against them are often reinforced by their media representation as unpredictable, violent and dangerous. Hence the importance of the study of these misconceptions helps in the management of the mentally ill in our societies.1
Stigma places obstructions to social success for patients. In addition, the attitudes of the public toward them is often internalized and results in lowered self-esteem, hopelessness and despair for sufferers. Misconceptions about mental illness are pervasive, and the lack of understanding can have serious consequences for millions of people who have a psychiatric illness.
In our society especially in rural communities the persons with psychiatric illness often perceived as unwanted elements, and societal stigma prevents them from seeking help and treatment. In recent years the awareness about mental illness has been changed a lot, even if the misconceptions about mental illness still present in society. Many studies done by WHO and other agencies points the need of awareness programmes in the society for eradicating stigma. Recently the
- 2 - Erwadi incident in Tamilnadu points the need of proper mental health awareness in communities. The Indian mental health act, 1987, is an amendment of the Indian lunacy act, 1912.The present act recognizes the crucial role of treatment and care of mentally ill persons. 2 .But still in some part of our country mental illnesses are considered as sins and witchcraft, and these believes prevent them from seeking medical help. Mental health professionals can play a major role in prevention of misconception among communities.
6.2) NEED FOR THE STUDY:
“ They don’t want mental problems in the family to be exposed. They want to hide it to preserve the family image and status.”
World Health Organization estimates that 10% of the world's population has some form of mental disability and 1% suffers from severe incapacitating mental disorders. Community-based surveys conducted during the past two decades in India showed that the total prevalence of psychiatric disorder was around 5.8%. Mental Health Act 1987 provides safeguards against stigmatization and discrimination for patients suffering from mental illness.3
Mental illness often generates misunderstanding, prejudice, confusion and fear. Some people with mental illness report that the stigma can at times be worse than the illness itself. People may be less willing to offer support and empathy if someone is experiencing a mental illness rather than a physical health problem. Those with a history of mental illness may find that others become uncomfortable or distrustful around them and that they lose contact with family and friends. People who are known to have had mental illness may find it more difficult to find employment or get a promotion, even if they are well at the time.
Another misconception is that a mental illness represents a lifelong disorder, with little chance of recovery. In fact, many people experience only one episode of a mental illness - such as depression or a psychotic disorder - and then recover. Some people have an illness which recurs during their life, but many are well much of the time and the illness can often be managed successfully.
Misconceptions about mental illness are pervasive, and the lack of understanding can have serious consequences for millions of people who have a
- 3 - psychiatric illness, Misconceptions about mental illness contribute to the stigma, which leads many people to be ashamed and prevents them from seeking help. A number of research studies found that the majority of the public still have difficulty accepting mentally ill people as employees, tenants, spouses or neighbors. The misconception that most mentally ill people are dangerous is clearly one of the sources of these attitudes. A recent survey of the Pennsylvania's County Behavioral Health Directors also identified stigma as one of the biggest obstacles preventing the severely mentally ill from achieving the best quality of life possible for them. 3
As a Postgraduate Psychiatric nursing student investigator find there is an ample misconception still present in Indian communities regarding the mental illness. Most of the time the psychiatric nursing care will focus only to patients, and neglect the community that which the patient lives. Psychiatric illness also had a very high prevalence rate in community as same as of medical conditions like DM and Cancer. Every time I read disconcerting psychiatric news, like the Erwadi incident in Tamilnadu, the proper knowledge about mental illness among general population will help to change the attitude about mentally ill persons in the society and helps the mentally ill persons in society.
6.3) STATEMENT OF THE PROBLEM
“A STUDY TO ASSESS THE EFFECTIVENESS OF STRUCTURED TEACHING PROGRAMME ON MISCONCEPTION ABOUT MENTALL ILLNESS AMONG ADULT PEOPLE LIVING IN SELECTED RUREL AND URBAN COMMUNITY IN HASSAN DISTRICT , KARNATAKA”
6.4) OBJECTIVES OF THE STUDY ARE:
1 To assess the knowledge and attitude of the urban and rural persons regarding misconceptions about mental illness through pretest. 2 To asses the effectiveness of STP regarding misconceptions about mental illness in urban and rural community. 3 To evaluate the knowledge misconceptions about mental illness of urban and rural persons through post test
- 4 - 4 To associate the knowledge and attitude changes of urban and rural community through pretest and posttest scores.
6.5) HYPOTHESIS
S1: There is a significant difference in knowledge and attitudes of mental illness among urban and rural communities.
S2: There is a significant difference of knowledge and attitude score before and after the implementation of structured teaching programme on misconception about mental illness among urban and rural communities.
6.6) ASSUMPTION
This study assumed that: -
1. There is a significant widespread misconception about mental illness among urban and rural communities of India. 2. There is more level of misconceptions about mental illness among rural communities than that of urban community. 3. Structured teaching programme will improve the knowledge and attitude about mental illness among urban and rural communities. .
6.7) OPERATIONAL DEFINITION
1 Assess: - It refers to determine the knowledge and attitude of urban and rural community regarding the misconception about mental illness.
2. Effectiveness: - It refers to the extent to which the knowledge level is improved.
3 Structured Teaching Programme: - It refers to systematically planned teaching programme designed to provide information regarding factors influencing the misconceptions about mental illness.
- 5 - 4 Mental illness: - The term that refers collectively to all mental disorders, mental disorders are health conditions that are characterized by alteration in thinking mood or behavior associate with distress or impaired functioning.
5 Middle adult: - It refers to a person living in urban and rural area of Hassan and in between the age group of 25-50 years of age.
6 Rural: - It refers the place where people live with minimum living standards and far from the town and cities.
7 Urban: -It refers the place where high population density and people living with more sophisticated living standards, and have good educational status.
6.8) CRITERIA FOR SELECTION OF SAMPLE
INCLUSION CRITERIA
1. Adults who all are willing to participate in the study. 2. Adults, between the age group of 25-50 years of age.
3. Adults who are free from mental illness.
4. Adults who can read and write Kannada.
.
EXCLUSION CRITERIA
1. Adults who all are not willing to participate in the study. 2. Adults who have psychiatric illness. 3. Adults who cant read and write Kannada
6.9) DELIMITATION
This study is limited to: -
- 6 - 1) This study is limited to the adult people living in urban and rural communities of Hassan District.
2) This study is limited to the period of 4 to 6 weeks
6.10) SIGNIFICANCE OF STUDY
This study will: -
1) Promote knowledge regarding the cause of psychiatric illness.
2) Helps to promote the positive attitude of peoples towards mentally ill patients.
6.11) CONCEPTUAL FRAME WORK
This study is based on “General system theory”.
6.12) REVIEW OF LITERATURE.
The study was conducted by Aghanwa HS in 2004 on Attitude toward and knowledge about mental illness in Fiji islands. This study aimed to explore information on the extent of knowledge about mental illness and attitudes toward the mentally ill in Fiji, and also to determine the factors influencing them. The interview schedule used elicited socio-demographic characteristics, knowledge of, and attitudes toward, mental illness. A majority of the subjects attributed the cause of mental illness to substance abuse, believed in the diversity of mental illness, considered hospital as an important source of help and acknowledged the effectiveness of medication. Less than one-fifth of the subjects were willing to marry or employ mentally ill persons. About 42% of the sample would have shame on seeking help. Educational attainment was correlated with knowledge about mental illness, except with knowledge about early mental symptoms. Prestigious occupation, single marital status, female gender, younger age and urban dwelling were associated with positive disposition toward the mentally ill. Race was not significantly influential on almost all attitudinal variables. The study recommends health education and awareness programme in communities of Fiji islands4.
The study was conducted by Jans M ,University of Queensland in 2004 mental health literacy in rural Queensland; Australia The aim of this study
- 7 - was to assess the awareness of, and attitudes to, mental health issues in rural dwelling Queensland residents. A secondary objective was to provide baseline data of mental health literacy prior to the implementation of Australian Integrated Mental Health Initiative. While a higher proportion of respondents (81%) correctly identified and labeled the problem in the vignette as depression than previously reported in Australian community surveys, the majority of respondents (66%) underestimated the prevalence of mental health problems in the community. The mental health literacy in rural Queensland appears to be comparable to other Australian regions, several gaps in knowledge were identified in the study, and recommends there is a continuing need for mental health education in rural Queensland5.
The study was conducted by Oye Gureje, PhD, DSc etal in 2004 on Community study of knowledge of and attitude to mental illness in Nigeria. With the Objectives to determine the knowledge and attitudes of a representative community sample in Nigeria. Clustered sample of household respondents was studied in three states in the Yoruba-speaking parts of Nigeria (representing 22% of the national population). Poor knowledge of causation was common. Negative views of mental illness were widespread, with as many as 96.5% believing that people with mental illness are dangerous because of their violent behavior. Most would not tolerate even basic social contacts with a mentally ill person: 82.7% would be afraid to have a conversation with a mentally ill person and only 16.9% would consider marrying one. Socio-demographic predictors of both poor knowledge and intolerant attitude were generally very few. There is widespread stigmatization of mental illness in the Nigerian community. Negative attitudes to mental illness may be fuelled by notions of causation that suggest that affected people are in some way responsible for their illness, and by fear, the researcher recommends wider community awareness programmes on mental illness. 6
The study was conducted by Jason Luty etal in 2007 on Effectiveness of Changing Minds campaign fact sheets in reducing stigmatized attitudes towards mental illness. To assess the effect of fact sheets from the Royal College of Psychiatrists’ Changing Minds campaign on stigmatized attitudes of members of the general public towards those with mental illness. Participants were recruited at random from a panel of over 1200 members of the general population and presented
- 8 - with questionnaires containing single-page fact sheets adapted from the Changing Minds campaign describing schizophrenia or substance use disorders. The Attitudes to Mental Illness Questionnaire (AMIQ) was used to measure the effect on stigmatized attitudes. The AMIQ scores for the alcoholism and schizophrenia vignettes did not differ between experimental and control groups. Suggest that a better strategy to reduce the stigma associated with mental disorders would be to present positive images.7
The study was conducted by M. C. Angermeyer and S. Dietrich in 2005 on Public beliefs about and attitudes towards people with mental illness: a review of population studies to provide a review of population-based attitude research in psychiatry during the past 15 years. An electronic search using PubMed, Medline, and Academic Search Premier plus a hand search of the literature was carried out for studies on public beliefs about mental illness and attitudes towards the mentally ill published between 1990 and 2004. Thirty-three national studies and 29 local and regional studies were identified, mostly from Europe. Although the majorities are of descriptive nature, more recent publications include studies testing theory-based models of the stigmatization of mentally ill people. There is still much to be done to provide an empirical basis for evidence-based interventions to reduce misconceptions about mental illness and improve attitudes towards persons with mental illness8.
The study was conducted by Sucrets Jadhav etal in 2007 on Stigmatization of severe mental illness in India Against the simple industrialization hypothesis with the objective to test the hypothesis that there are fewer stigmatizing attitudes towards the mentally ill amongst rural compared to urban community dwellers in India. An ethnographically derived and vignette-based stigmatization scale was administered to a general community sample comprising two rural and one urban site in India Rural Indians showed significantly higher stigma scores, especially those with a manual occupation. The overall pattern of differences between rural and urban samples suggests that the former deploy a punitive model towards the severely mentally ill, while the urban group expressed a liberal view of severe mental illness. Urban Indians showed a strong link between stigma and not wishing to work with a mentally ill individual, whereas no such link existed for rural Indians. And the study
- 9 - recommends further more studies regarding the community perceptions about mentally ill persons and stigma prevention campaigns9.
The study was conducted by D, Vimala etal in Oct 2003 on assess the knowledge, attitude and practices of family members of clients with mental illness in, Vellore. The objectives was to assess the knowledge, attitudes and practices of family members of clients regarding mental illness, to identify the pathway to care for the clients with mental illness and to assess the relationship between the knowledge attitude and practice and selected sociodemographic characteristics. The subjects were confidentially interviewed by the investigator. Study shows the family members had an adequate level of knowledge regarding mental illness. All subjects were able to state at least one symptom or sign of mental illness and 78% were able to identify a cause or factor precipitating the onset of illness. Almost all (97%) stated that mental illness is curable with medication. Much less than half the family members (40%) have expressed the misconceptions regarding mental illness. Study recommends educational interventions are necessary to improve the general knowledge of family members regarding mental illness10.
The study was conducted by Kermode M etal.on 2009 Community beliefs about causes and risks for mental disorders: A mental health literacy survey in a rural area of Maharashtra, India. This study aimed to assess local knowledge and understanding of causes and risks for mental disorders in a rural area of Maharashtra, and to assess the prevalence of possible common mental disorders. A questionnaire was administered to 240 systematically sampled community members and 60 village health workers. Study indicated that 27% had a possible common mental disorder and that the elderly were at increased risk, community perceptions enhancing mental health literacy of both Village health visitors and community members using approaches that are sensitive to local conceptualizations of mental health and illness will contribute to improved treatment and care for people with mental disorders. Further investigation of mental health among the elderly in this community is indicated.11
The study was conducted by S Ganesh Kumar etal in 2008 on Prevalence and pattern of mental disability using Indian disability evaluation assessment scale in a rural community of Udupi, Karnataka with the Objectives to
- 10 - assess the prevalence and pattern of mental disability. The study was conducted by making house-to-house visits, interviewing, and examining all the individuals in the families selected with pre-designed and pretested questionnaire. The prevalence of mental disability was found to be 2.3%. The prevalence was higher among females (3.1%) than among males (1.5%). The prevalence was higher among the elderly age group and illiterates. There is ample scope for community-based rehabilitation of the mentally disabled and the need for awareness campaigns. 12
The study was conducted by GourieDevi M etal on Prevalence of neurological disorders in Bangalore, India: a community-based study with a comparison between urban and rural areas, A population-based neuroepidemiological survey of 102,557 individuals in urban and rural Bangalore in Southern India was studied to determine the prevalence and pattern of neurological disorders respectively. The study shows prevalence of neurological disorders among women (3,617) is higher compared with men (2,657). The prevalence rate in urban and rural populations was 2,190 and 4,070/1, 00,000 respectively, implying that neurological disorders were twice as frequent in rural areas as in urban areas. The study recommends the larger community based surveys for Prevalence of neurological disorders and prevention of misconceptions about mental illness.13
The study was conducted by Dr. Raguram etal in 2004 in schizophrenia and cultural epidemiology of stigma in Bangalore. Studied the Schizophrenia and the cultural epidemiology of stigma by interviewing caretakers of 60 Schizophrenic patients using 13 stigma queries positive and negative symptom scale. The study finds features of Schizophrenia related stigma in India, and recommends further comparative cultural studies and community awareness programs in India.14
7. MATERIAL AND METHDS OF STUDY
SOURCE OF DATA -; Data will be collected from the rural and urban middle adults.
METHODS OF COLLECTING DATA-:
- 11 - 1) Research design: -The research design used True-experimental (Solomon four group pre-test post-test designs).
Schematic plan of the study
80 Adult persons Pre test Intervention Post test
Er O1 X O2
RURAL
Cr O1 _ O2
URBAN Eu O1 X O2
Cr O1 _ O2
KEY WORDS
Eu- Experimental group urban
ER- Experimental group rural
Cr-Control group rural
Cr-Control group urban
01- Pre test
02- Post test
X- Structured Teaching Programme. (Intervention)
- 12 - 2) Research setting: - The study will be conducted in the rural and urban communities of Hassan District.
3) Population: - Middle adults living in urban and rural communities of Hassan district.
4) Sample: - Middle adult persons fulfill the inclusive criteria are the samples.
5) Sample Size: - Sample comprised 80 middle adults, in which 40 urban and 40 Rural.
6) Sample Technique:- Non Probability sample Convenience sampling method will be used 7) Collection of Data: - Collection of data is done by using self-administered questionnaires.
8) VARIABLES: -
Independent variable: - STP on misconception about mental illness.
Dependent variable: - Knowledge and attitude of middle adult persons regarding mental illness.
9) PLAN FOR DATA ANALYSIS: -
Descriptive statistics: -The descriptive statistical analysis includes frequencies, percentages, means, and Standard deviation for the middle adult persons regarding the knowledge and attitude about mental illness.
Inferential statistics: - pretest and post test difference in knowledge and attitude about mental illness score will be analyzed by using student paired t-test, Mc Nemar chi-square test, and an association between demographical variables and level of knowledge on factors of misconceptions about mental illness and its prevention will be analyzed using Pearson chi-square test/ Yates corrected chi- square test.
- 13 - 10) PILOT STUDY:
The pilot study is planned with 10% of the population, which will be conducted during the time of study.
11) ETHICAL CONSIDERATION: -
1. Does the study require any interventions to be conducted on samples?
------Yes. Informed consent will be obtained from respondents.
2. Has ethical clearance being obtained from your institution?
------Yes. Ethical clearance has been obtained from the institution.
3. Has the consent being taken from the local authorities?
-----Yes. Consent has been taken from the local authorities.
12) LISTS OF REFERENCES
1. Rohan Ganguly, Understand the weak link between mental illness and violent behavior.2000 Mar. www.msn.com/discussion/psychiatry. 2. Bimala Kapoor, Text Book Of Psychiatric Nursing, Kumar Publishers ,New Delhi,2005.Vol.2 ,2 Edn,445-46. 3. Prince PN. Prince CR. Perceived stigma and community integration among clients of assertive community treatment. Psychiatric Rehabilitation Journal.2002 ;25(4):323-31 4. Aghanwa HS Attitude toward and knowledge about mental illness in Fiji islands.2004;Apr; 24(4): 364-9. 5. Jans M, mental health literacy in rural Queensland; Australia University of Queensland Australian and New Zealand Journal of Psychiatry.2006: Vol40 ( 9) 783-89. 6. Oye Gureje, Victor O,Lasebikan, Olusola Ephraim Oluwanuga Community study of knowledge of and attitude to mental illness in Nigeria.2004.
- 14 - 7. Jason Luty etal, Effectiveness of Changing Minds campaign fact sheets in reducing stigmatized attitudes towards mental illness, Psychiatric Bulletin.2007;31: 377-381. 8. M. C. Angermeyer and S. Dietrich on Public beliefs about and attitudes towards people with mental illness: a review of population studies to provide a review of population-based attitude research in psychiatry during the past 15 years using electronic search. 2005. http://eliminatethestigma.wordpress.com/understandingmental-illness/ 9. Sushrut Jadhav etal Stigmatization of severe mental illness in India: Against the simple industrialization hypothesis, Indian journal of psychiatry,2007,49(3): 189-94. 10. Vimala D, Rajan, Annantha Kumari, Siva, Rajeswari, Braganza, Deepa,A study to assess the knowledge, attitude and prctices of family members of clients with mental illness Nursing Journal of India. 2003; 1(3):16-8. 11. Kermode M, Bowen K, Arole S, Joag K, Jorm AF, Community beliefs about causes and risks for mental disorders: A mental health literacy survey in a rural area of Maharashtra, India International Journal Social Psychiatry. 2009 ;Sep: 12(8)23-8. 12. Ganesh Kumar etal. Prevalence and pattern of mental disability using Indian disability evaluation assessment scale in a rural community of Karnataka, Indian journal of psychiatry,2008:50(1),21-23. 13. Gourie Devi M etal. Prevalence of neurological disorders in Bangalore, India: a community-based study with a comparison between urban and rural areas. Neuroepidemiology. 2004. 23(6):261-8. 14. Raguram etal schizophrenia and cultural epidemiology of stigma in Bangalore, The Journal of Nervous and Mental Disease: 2004; Nov ;192 ( 11): 734-44.
- 15 -