Tropical Gastroenterology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Part 05.Indd
PART MISCELLANEOUS 5 TOPICS Awards and Honours Y NATIONAL AWARDS NATIONAL COMMUNAL Mohd. Hanif Khan Shastri and the HARMONY AWARDS 2009 Center for Human Rights and Social (announced in January 2010) Welfare, Rajasthan MOORTI DEVI AWARD Union law Minister Verrappa Moily KOYA NATIONAL JOURNALISM A G Noorani and NDTV Group AWARD 2009 Editor Barkha Dutt. LAL BAHADUR SHASTRI Sunil Mittal AWARD 2009 KALINGA PRIZE (UNESCO’S) Renowned scientist Yash Pal jointly with Prof Trinh Xuan Thuan of Vietnam RAJIV GANDHI NATIONAL GAIL (India) for the large scale QUALITY AWARD manufacturing industries category OLOF PLAME PRIZE 2009 Carsten Jensen NAYUDAMMA AWARD 2009 V. K. Saraswat MALCOLM ADISESHIAH Dr C.P. Chandrasekhar of Centre AWARD 2009 for Economic Studies and Planning, School of Social Sciences, Jawaharlal Nehru University, New Delhi. INDU SHARMA KATHA SAMMAN Mr Mohan Rana and Mr Bhagwan AWARD 2009 Dass Morwal PHALKE RATAN AWARD 2009 Actor Manoj Kumar SHANTI SWARUP BHATNAGAR Charusita Chakravarti – IIT Delhi, AWARDS 2008-2009 Santosh G. Honavar – L.V. Prasad Eye Institute; S.K. Satheesh –Indian Institute of Science; Amitabh Joshi and Bhaskar Shah – Biological Science; Giridhar Madras and Jayant Ramaswamy Harsita – Eengineering Science; R. Gopakumar and A. Dhar- Physical Science; Narayanswamy Jayraman – Chemical Science, and Verapally Suresh – Mathematical Science. NATIONAL MINORITY RIGHTS MM Tirmizi, advocate – Gujarat AWARD 2009 High Court 55th Filmfare Awards Best Actor (Male) Amitabh Bachchan–Paa; (Female) Vidya Balan–Paa Best Film 3 Idiots; Best Director Rajkumar Hirani–3 Idiots; Best Story Abhijat Joshi, Rajkumar Hirani–3 Idiots Best Actor in a Supporting Role (Male) Boman Irani–3 Idiots; (Female) Kalki Koechlin–Dev D Best Screenplay Rajkumar Hirani, Vidhu Vinod Chopra, Abhijat Joshi–3 Idiots; Best Choreography Bosco-Caesar–Chor Bazaari Love Aaj Kal Best Dialogue Rajkumar Hirani, Vidhu Vinod Chopra–3 idiots Best Cinematography Rajeev Rai–Dev D Life- time Achievement Award Shashi Kapoor–Khayyam R D Burman Music Award Amit Tivedi. -
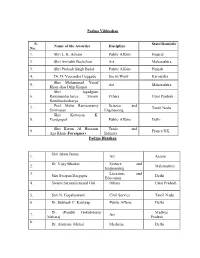
Padma Vibhushan S. No. Name of the Awardee Discipline State/Domicile
Padma Vibhushan S. State/Domicile Name of the Awardee Discipline No. 1. Shri L. K. Advani Public Affairs Gujarat 2. Shri Amitabh Bachchan Art Maharashtra 3. Shri Prakash Singh Badal Public Affairs Punjab 4. Dr. D. Veerendra Heggade Social Work Karnataka Shri Mohammad Yusuf 5. Art Maharashtra Khan alias Dilip Kumar Shri Jagadguru 6. Ramanandacharya Swami Others Uttar Pradesh Rambhadracharya Prof. Malur Ramaswamy Science and 7. Tamil Nadu Srinivasan Engineering Shri Kottayan K. 8. Venugopal Public Affairs Delhi Shri Karim Al Hussaini Trade and 9. France/UK Aga Khan ( Foreigner) Industry Padma Bhushan Shri Jahnu Barua 1. Art Assam Dr. Vijay Bhatkar Science and 2. Maharashtra Engineering 3. Literature and Shri Swapan Dasgupta Delhi Education 4. Swami Satyamitranand Giri Others Uttar Pradesh 5. Shri N. Gopalaswami Civil Service Tamil Nadu 6. Dr. Subhash C. Kashyap Public Affairs Delhi Dr. (Pandit) Gokulotsavji Madhya 7. Art Maharaj Pradesh 8. Dr. Ambrish Mithal Medicine Delhi 9. Smt. Sudha Ragunathan Art Tamil Nadu 10. Shri Harish Salve Public Affairs Delhi 11. Dr. Ashok Seth Medicine Delhi 12. Literature and Shri Rajat Sharma Delhi Education 13. Shri Satpal Sports Delhi 14. Shri Shivakumara Swami Others Karnataka Science and 15. Dr. Kharag Singh Valdiya Karnataka Engineering Prof. Manjul Bhargava Science and 16. USA (NRI/PIO) Engineering 17. Shri David Frawley Others USA (Vamadeva) (Foreigner) 18. Shri Bill Gates Social Work USA (Foreigner) 19. Ms. Melinda Gates Social Work USA (Foreigner) 20. Shri Saichiro Misumi Others Japan (Foreigner) Padma Shri 1. Dr. Manjula Anagani Medicine Telangana Science and 2. Shri S. Arunan Karnataka Engineering 3. Ms. Kanyakumari Avasarala Art Tamil Nadu Literature and Jammu and 4. -

We Had Vide HO Circular 443/2015 Dated 07.09.2015 Communicated
1 CIRCULAR NO.: 513/2015 HUMAN RESOURCES WING I N D E X : STF : 23 INDUSTRIAL RELATIONS SECTION HEAD OFFICE : BANGALORE-560 002 D A T E : 21.10.2015 A H O N SUB: IBA MEDICAL INSURANCE SCHEME FOR RETIRED OFFICERS/ EMPLOYEES. ******* We had vide HO Circular 443/2015 dated 07.09.2015 communicated the salient features of IBA Medical Insurance Scheme for the Retired Officers/ Employees and called for the option from the eligible retirees. Further, the last date for submission of options was extended upto 20.10.2015 vide HO Circular 471/2015 dated 01.10.2015. The option received from the eligible retired employees with mode of exit as Superannuation, VRS, SVRS, at various HRM Sections of Circles have been consolidated and published in the Annexure. We request the eligible retired officers/ employees to check for their name if they have submitted the option in the list appended. In case their name is missing we request such retirees to take up with us by 26.10.2015 by sending a scan copy of such application to the following email ID : [email protected] Further, they can contact us on 080 22116923 for further information. We also observe that many retirees have not provided their email, mobile number. In this regard we request that since, the Insurance Company may require the contact details for future communication with the retirees, the said details have to be provided. In case the retirees are not having personal mobile number or email ID, they have to at least provide the mobile number or email IDs of their near relatives through whom they can receive the message/ communication. -
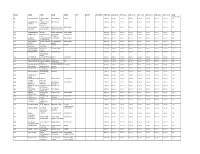
Folio Name Add1 Add2 Add3 City State Country Pincode Div 08-09 Div 09-10 Div 10-11 Div 11-12 Div 12-13 Div 13-14 Div 14-15 Shr- 31.10.2017
FOLIO NAME ADD1 ADD2 ADD3 CITY STATE COUNTRY PINCODE DIV 08-09 DIV 09-10 DIV 10-11 DIV 11-12 DIV 12-13 DIV 13-14 DIV 14-15 SHR- 31.10.2017 83 RAJEEV BHASIN 1267 PAHARI JAMA MASJID DELHI 110006 100.00 100.00 150.00 100.00 100.00 100.00 100.00 100 IMLI 93 JAWAHAR LAL PHASE III 1/5 NEW DELHI 110015 100.00 100.00 150.00 100.00 100.00 100.00 100.00 100 JAISWAL NEW MOTI NAGAR 95 SUNIL KUMAR C/O NARENDRA SERVICE P LTD L 7 NEW DELHI 110016 200.00 200.00 300.00 200.00 200.00 200.00 200.00 200 SHARMA SHARMA MAS GREEN PARK EXT 107 RAJESH MEHRA H NO 27 K BLOCK KALKAJI NEW DELHI 110019 100.00 100.00 150.00 100.00 100.00 100.00 100.00 100 136 SUBEK SINGH QUARTER NO R K PURAM NEW DELHI 110022 100.00 100.00 150.00 100.00 100.00 100.00 100.00 100 1482 SECTOR 5 168 KRISHNA 19 LAJ BHAWAN PAHARGANJ NEW DELHI 110055 100.00 100.00 150.00 100.00 100.00 100.00 100.00 100 KACHROO CHUNA MANDI 172 ANIL KUMAR 14/287 SECTOR DR AMBEDKAR NEW DELHI 110062 200.00 200.00 300.00 200.00 200.00 200.00 200.00 200 SINGH 5 NAGAR 191 NAND LAL D-11/81 ROHINI DELHI 110085 100.00 100.00 150.00 100.00 100.00 100.00 100.00 100 DHURIYA SECTOR-8 215 VINOD KUMAR DA-50 SIHI BALLAB GARH 121004 200.00 200.00 300.00 200.00 200.00 200.00 200.00 200 MANCHANDA GATE 220 KEWAL SINGH PLOT NO 167 CHANDIGARH 160001 200.00 200.00 300.00 200.00 200.00 200.00 200.00 200 INDUSTRIAL AREA I 228 A K SHARMA 1009 SECTOR 37 NOIDA GAZIABAD 201301 200.00 200.00 300.00 200.00 200.00 200.00 200.00 200 230 JHAMMAN SINGH F-27 SECTOR 20 NOIDA U P 201301 100.00 100.00 150.00 100.00 100.00 100.00 100.00 100 237 UDAY -

Awards & Honours
1st January to 15 th January AWARDS & HONOURS The Hollywood Foreign Press Association (HFPA) presented the 72nd Annual Golden Globe Awards. The winners are:- BEST MOTION PICTURE DRAMA - Boyhood (IFC Films) BEST PERFORMANCE BY AN ACTRESS IN A MOTION PICTURE – DRAMA - Julianne Moore – Still Alice BEST PERFORMANCE BY AN ACTOR IN A MOTION PICTURE DRAMA - Eddie Redmayne – The Theory of Everything BEST MOTION PICTURE COMEDY OR MUSICAL - The Grand Budapest Hotel (Fox Searchlight) BEST PERFORMANCE BY AN ACTRESS IN A MOTION PICTURE – COMEDY OR MUSICAL - Amy Adams – Big Eyes BEST PERFORMANCE BY AN ACTOR IN A MOTION PICTURE – COMEDY OR MUSICAL- Michael Keaton – Birdman BEST ANIMATED FEATURE FILM - How to Train a Dragon 2 (DreamWorks Animation) BEST FOREIGN LANGUAGE FILM - Leviathan – Russia (Sony Pictures Classics) Prime Minister Narendra Modi released commemorative coins to honour Tata Group founder Jamsetji Nusserwanji Tata. PM released coins in the denomination of 100 and five rupee to mark Jamsetji Tata’s 175th birth anniversary. Thus, Jamsetji will be the first industrialist in India to be felicitated by the government in such a manner. So far government has minted coins in honour of artists, freedom fighters, scientists, institutions and organisations. Reserve Bank of India's (RBI) Raghuram Rajan has been awarded as the Governor of the Year in the Central Banking Awards for 2015, while the Reserve Bank of New Zealand (RBNZ) scooped the prize for Central Bank of the Year. Last year, Rajan was also conferred with the Best Central Bank Governor award for 2014 by the Euromoney magazine for his tough monetary stance to combat the 'ravaging deficit-ridden economy' and battling vested interests "to arouse a sleepy financial system for over one billion people.” French economist Thomas Piketty, who rose to international fame after the publication of his book, “Capital in the Twenty-First Century,” in 2013, turned down Legion D'Honneur -- France’s highest distinction. -

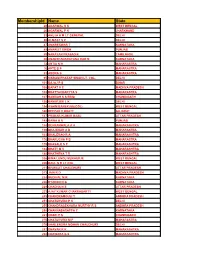
Alphabetical List of Persons for Whom Recommendations Were Received for Padma Awards - 2015
Alphabetical List of Persons for whom recommendations were received for Padma Awards - 2015 Sl. No. Name 1. Shri Aashish 2. Shri P. Abraham 3. Ms. Sonali Acharjee 4. Ms. Triveni Acharya 5. Guru Shashadhar Acharya 6. Shri Gautam Navnitlal Adhikari 7. Dr. Sunkara Venkata Adinarayana Rao 8. Shri Pankaj Advani 9. Shri Lal Krishna Advani 10. Dr. Devendra Kumar Agarwal 11. Shri Madan Mohan Agarwal 12. Dr. Nand Kishore Agarwal 13. Dr. Vinay Kumar Agarwal 14. Dr. Shekhar Agarwal 15. Dr. Sanjay Agarwala 16. Smt. Raj Kumari Aggarwal 17. Ms. Preety Aggarwal 18. Dr. S.P. Aggarwal 19. Dr. (Miss) Usha Aggarwal 20. Shri Vinod Aggarwal 21. Shri Jaikishan Aggarwal 22. Dr. Pratap Narayan Agrawal 23. Shri Badriprasad Agrawal 24. Dr. Sudhir Agrawal 25. Shri Vishnu Kumar Agrawal 26. Prof. (Dr.) Sujan Agrawal 27. Dr. Piyush C. Agrawal 28. Shri Subhash Chandra Agrawal 29. Dr. Sarojini Agrawal 30. Shri Sushiel Kumar Agrawal 31. Shri Anand Behari Agrawal 32. Dr. Varsha Agrawal 33. Dr. Ram Autar Agrawal 34. Shri Gopal Prahladrai Agrawal 35. Shri Anant Agrawal 36. Prof. Afroz Ahmad 37. Prof. Afzal Ahmad 38. Shri Habib Ahmed 39. Dr. Siddeek Ahmed Haji Panamtharayil 40. Dr. Ranjan Kumar Akhaury 41. Ms. Uzma Akhtar 42. Shri Eshan Akhtar 43. Shri Vishnu Akulwar 44. Shri Bruce Alberts 45. Captain Abbas Ali 46. Dr. Mohammed Ali 47. Dr. Govardhan Aliseri 48. Dr. Umar Alisha 49. Dr. M. Mohan Alva 50. Shri Mohammed Amar 51. Shri Gangai Amaren 52. Smt. Sindhutai Ramchandra Ambike 53. Mata Amritanandamayi 54. Dr. Manjula Anagani 55. Shri Anil Kumar Anand 56. -

Agenda - B Reporting Matters
78th IMA Central Council Meeting, December 27-28, 2017, Mumbai, Maharashtra AGENDA - B REPORTING MATTERS 1. Minutes of 137th Ordinary meeting of the Central Council of IMA.............................................................. 21 2. Minutes of the 217th meeting of the Central Working Committee held at Kolkata on April 15&16, 2017 and Action Taken thereon .............................................................................................. 21 3. Minutes of the 218th meeting of the Central Working Committee held at New Delhi on September 2324, 2017 ................................................................................................................................. 40 Reports by National Vice Presidents of IMA 4. Activity report of Dr Roy Abraham Kallivayalil, Senior National Vice President ....................................... 49 5. Activity report of Dr K Prakasam, National Vice President ............................................................................. 6. Activity report of Dr Mahendra Choudhury, National Vice President ......................................................... 52 7. Activity Report of Dr Parmanand Prasad Pal, National Vice President, IMA ................................................. Report by Honorary Secretary General, IMA, Dr R N Tandon 8. Glimpses of activities of Team Digital IMA Dr K K Aggarwal, National President, IMA and Dr R N Tandon, Honorary Secretary General, IMA ..............................................................Agenda Book No. 8 9. Minutes of meeting -

Consensus Statement of Padma Awardee Doctors' Forum Regarding
CONSENSUS STATEMENT (Padma Awardee Doctors' Forum) Indian Journal of Clinical Practice, Vol. 30, No. 4, September 2019 Consensus Statement of Padma Awardee Doctors’ Forum Regarding Exclusion of Medical Professionals from the Consumer Protection Act India International Centre (IIC), New Delhi | August 28, 2019 KK AGGARWAL, AK BHALLA, AK GROVER, ANOOP MISRA, ARVIND LAL, AS SOIN, ASHOK SETH, BN SAHI, DS GAMBHIR, GANESH MANI, GK KHATRI, HARSH MAHAJAN, KALYAN BANERJEE, KK SETHI, KK TALWAR, M KHALILULLAH, M WALI, MADAN MOHAN, MAHESH VERMA, MALVIKA SABHARWAL, NEELAM KLER, NIKHIL TANDON, NITISH NAIK, NK PANDEY, NM SHROFF, NP GUPTA, P LAL, P VENUGOPAL, RAMAN KAPOOR, RANDHIR SUD, RK GROVER, SANJEEV BAGAI, SAUMITRA RAWAT, SC MANCHANDA, TS KLER, UPENDRA KAUL, YASH GULATI he Consumer Protection Bill, 1986 was passed by CONSUMER PROTECTION ACT, 2019 both the Houses of Parliament and it received the assent of the President on 24th December 1986. The Consumer Protection Bill, 2019 has been passed T by both Houses of Parliament i.e. Lok Sabha (30th It came on the Statutes Book as The Consumer Protection Act, 1986 (68 of 1986). The Legislature while July 2019) and Rajya Sabha (6th August 2019). Thus, drafting the Bill, 1986 had specifically not included the a new law on consumer protection has been enacted services provided by the medical professionals in the i.e. the Consumer Protection Act, 2019. The new term of services. Also, there is no mention of medical act does not include services rendered by medical professionals, doctors, etc., anyplace in the Consumer professionals. Protection Act, 1986. Earlier, when amendments to the Consumer Protection The fact that there is a distinction between a profession Act were introduced in 2015, there was no mention and an occupation was the main reason for not of “health care” in the list of examples of as to including the medical professionals under the purview what constitutes “service”. -

Unpaid-Dividend-31St
Statement of unpaid Dividend as on 05.09.2017, declared at the AGM of the Company held on 31st July, 2017 ( As per the provision of the U/s. 124(2) of the Companies Act, 2013) Unpaid FOLIO/DP ID/ CL ID Name of Shareholder Dividend Address Amount (```) 0000007 MR BHARAT KUMAR AGGARWAL 97.50 C/O ORIENT GENERAL IND. LTD,11 INDUSTRIAL ESTATE,SECTOR - 6,FARIDABAD,121006 0000009 MR ASHWANI CHOUDHRY 292.50 A-3/85 JANAKPURI,,,NEW DELHI,110058 0000010 MRS KANTA CHAUDHRY 292.50 A-3/85 JANAKPURI,,,NEW DELHI,110058 0000011 MR SHIVINDER SINGH 292.50 A-3/85 JANAKPURI,,,NEW DELHI,110058 0000029 MR AMRIT PAUL SINGH 585.00 C1A/39C JANAKPURI NEW DELHI,,,,110058 0000080 MR SHRENIK S BHANDARI 390.00 C/O MR SHRAD S BHANDARI,E-7 GREEN PARK EXTENSION,IIND FLOOR,NEW DELHI,110016 0000108 MR RAJ KUMAR GUPTA 195.00 B 2/70 PHASE II,ASHOK VIHAR,,DELHI,110052 0000111 MRS SUDERSHAN CHAWLA 97.50 H NO 546 B WARD NO 15,NR JAGDISH PARK,JAGDISH COLONY,ROHTAK HARYANA,124001 0000115 MR HUKAM SINGH KAPRWAN 877.50 C-011 PRAGATI VIAHAR,LODHI ROAD P O NEW DELHI,,,110003 0000134 MISS MEENA SIRCAR 97.50 19A, CHOPRA HOUSE,GOBIND PURI,KANKARKHERA,MEERUT CANTT, 0000153 MRS SUDERSHAN 292.50 9/85 RAMESH NAGAR (SINGLE STOREY),NEW DELHI,,,110015 0000168 MRS MEENA GARG 292.50 B-76 GULMOHAR PARK,NEW DELHI,,,110049 0000198 MISS INDU SETHI 292.50 WZ-481 SHIV NAGAR,NEW DELHI,,,110058 0000258 MR DAYAL PARSHAD 97.50 S-349 GREATER KAILASH-I,NEW DELHI,,,110048 0000276 MR ANIL KUAMR SONI 325.00 6 ARJUN NAGAR P O SAFDAR JUNG,ENCLAVE,NEW DELHI,,110029 0000292 MISS SHALU BANSAL 97.50 C-76 ASHOK VIHAR -

DEPARTMENT NAME FATHER NAME EMAIL ID MOBILE CASTE GENDER ELECTRICAL BIPUL BORUAH ATUL BORUAH [email protected] 9085539878 OBC
LIST OF APPLICANTS SHORTLISTED FOR WRITTEN TEST TO THE POST OF GETs / MTs AGAINST ADVERTISEMENT NO. APL/HRM/Con/Adv-53(Pt-II)/169 Dated 07.05.2018 DEPARTMENT NAME FATHER NAME EMAIL_ID MOBILE CASTE GENDER ELECTRICAL BIPUL BORUAH ATUL BORUAH [email protected] 9085539878 OBC/MOBC Male ELECTRICAL SAOUHRIDYA PRAN KASHYAP PRANAV PRAN GOSWAMI [email protected] 9999999999 General Male ELECTRICAL PARTHA MITRA TAPAN KUMAR MITRA [email protected] 8234033597 General Male ELECTRICAL RAJAM BARUAH LATE DR. MUKUL KUMAR BARUAH [email protected] 8876339478 General Male ELECTRICAL TONMOYEE NATH TAPAN NATH [email protected] 9435529470 General Male ELECTRICAL SUMANJIT DEKA SARAT CH DEKA [email protected] 7002035430 General Male ELECTRICAL SUDIPTA SAIKIA GAJEN SAIKIA [email protected] 9706808418 OBC/MOBC Female ELECTRICAL MANASH PRATIM RAJBANGSHI ANNADA KUMAR DEKA [email protected] 9706707846 OBC/MOBC Male ELECTRICAL BISWAJIT GOGOI JITEN GOGOI [email protected] 9706754180 OBC/MOBC Male ELECTRICAL BIDYUT DEKA BHABESH DEKA [email protected] 8486316381 OBC/MOBC Male ELECTRICAL RAVI KANT SHANKHWAR BHEEM BABU SHANKHWAR [email protected] 9936649353 SC Male ELECTRICAL BHARGAB HAZARIKA RUDRA MOHAN HAZARIKA [email protected] 8254914496 General Male ELECTRICAL arun jyoti dutta bani dev dutta [email protected] 8403818084 General Male ELECTRICAL alpona kalita jogen kalita [email protected] 8638198633 General Female ELECTRICAL JYOTIPRAKASH LENKA ADWAITA KUMAR LENKA [email protected] 9439757642 General Male ELECTRICAL KRISHNA KANTA KAKATI DHARANIDHAR KAKATI [email protected] 9707118100 General Male ELECTRICAL GAUTAM DHIRAJLAL HINGRAJIYA DHIRAJLAL V. HINGRAJIYA [email protected] 9586035263 General Male ELECTRICAL LUHIT PHUKAN MADHAB CHANDRA PHUKAN [email protected] 8876371414 OBC/MOBC Male ELECTRICAL BISWAJIT DUTTA AKHIL DUTTA [email protected] 7576018187 General Male ELECTRICAL SAURABH RANJAN SHARMA SURESH SHARMA [email protected] 8747878111 OBC/MOBC Male ELECTRICAL VIKASH GOPAL CHAUBEY GOAPL R. -

Our Padma Honorees Dean AA 2019 DU Ach 76 Padmas to DU Alumni File 130 8 Padma Vibhushans , 25 Padma Bhushans and 43 Padma Shris …
alft 080 Our Padma Honorees Dean AA 2019 DU Ach 76 Padmas to DU alumni File 130 8 Padma Vibhushans , 25 Padma Bhushans and 43 Padma Shris … 1965 2001 Captain M S Kohli Padma Bhushan Uma Sharma Padma Bhushan Rahul Bajaj Padma Bhushan 1984 Aamir Raza Husain Padma Shri Dr Vera Hingorani Padma Shri 2002 1991 Nirmal Verma Padma Bhushan Passed Away 2005 Dr Shelja Mehra Padma Shri Jaspal Rana Padma Shri Shadi Lal Dhawan Padma Shri Kiran Martin Padma Shri 1992 2003 Sunita Kohli Padma Shri Prabhu Dayal Chawla Padma Bhushan Manoj Kumar Padma Shri 2004 1994 Dr CH Hanumantha Rao Padma Bhushan Dr Sneh Bhargava Padma Shri Dr Gopi Chand Narang Padma Bhushan 1998 2005 Dr Hem Lata Gupta Padma Bhushan Dr Karan Singh Padma Vibhushan J N Dixit Padma Vibhushan Passed away 2005 1999 Andre Beteille Padma Bhushan Shobha Deepak Singh Padma Shri Chitra Narain Padma Shri 2000 2006 Sikander Bakht Padma Vibhushan S Ramadorai Padma Bhushan Passed away 2004 Shekhar Kapur Padma Shri Anjolie Ela Menon Padma Shri 2007 2011 Khushwant Singh Padma Vibhushan Montek Singh Ahluwalia Padma Vibhushan Passed away 2007 Dr Meenakshi Gopinath Padma Shri Dr Kapila Vatsyayan Padma Vibhushan Dr Ananda Shankar Jayant Padma Shri Analjit Singh Padma Bhushan Naina Lal Kidwai Padma Shri Urvashi Butalia Padma Shri Dr Leela Omchery Padma Shri 2008 Professor Prithvi Nath Dhar Padma Vibhushan 2012 Passed away 2012 Dr Kaushik Basu Padma Shri Mira Nair Padma Bhushan Dr Bina Agarwal Padma Shri Dr Uma Tuli Padma Shri Barkha Dutt Padma Shri Irwin Allan Sealy Padma Shri Madan Mohan Sabharwal Padma -
Unregistered/Unreachable Members List
MembershipId Name State 20 AGARWAL S K WEST BENGAL 26 AGARWAL P K JHARKHAND 33 AHUJA A M LT GENERAL DELHI 39 ALMAST S C DELHI 47 AMARESWAR T KARNATAKA 48 AMARJIT SINGH PUNJAB 59 NARAYAN PRASAD K TAMILNADU 60 ANANTHANARAYANA RAO N KARNATAKA 72 ANTIA N H MAHARASTRA 76 APTE B P MAHARASTRA 83 ARORA S MAHARASTRA 95 VIKRAM PRATAP SINGH LT. COL. DELHI 101 BAJAJ P S BIHAR 108 BAPAT V C MADHYA PRADESH 109 BHATTACHARYYA S MAHARASTRA 127 BAMRAH N S BRIG CHANDIGARH 130 BANERJEE L K DELHI 134 ASHIM BANERJEE(COL) WEST BENGAL 140 DEEPAK V BHATT GUJARAT 147 PRANAB KUMAR BASU UTTAR PRADESH 149 BAWA H S PUNJAB 154 BEHRANWALA A A MAHARASHTRA 159 BHAJEKAR A B MAHARASTRA 163 BHALERAO R A MAHARASHTRA 176 BHARUCHA P B MAHARASTRA 179 BHASALE S P MAHARASHTRA 184 BHATT M V MAHARASHTRA 188 BHATHENA T R MAHARASHTRA 206 BIMA LENDU MUKHERJE WEST BENGAL 209 BAUL N R LT COL WEST BENGAL 211 BISWAJIT CHAUDHURI UTTAR PRADESH 213 JAIN R D MADHYA PRADESH 224 BUDIHAL M R KARNATAKA 226 BYAKOD N G KARNATAKA 229 CHADHA N S UTTAR PRADESH 233 AJAY KUMAR CHAKRABARTY WEST BENGAL 249 CHANDRAMOULI Y ANDHRA PRADESH 251 CHATURVEDI P K DELHI 255 CHANDRASEKHARA MURTHY R S ANDHRA PRADESH 258 CHANNABASAPPA C KARNATAKA 261 CHARI P S CHANDIGARH 275 CHATURVEDI M P MAHARASTRA 279 SHAILENDRA MOHAN CHAUDHURI DELHI 287 CHAVAN R K MAHARASHTRA 288 CHAWARA G S MAHARASHTRA 301 CHINNASWAMI C TAMIL NADU 309 YOG D K UTTAR PRADESH 324 PRAKASH RAO S R K TELANGANA 325 DAS M M WEST BENGAL 326 DAS P B ANDHRA PRADESH 339 DATTA A P WEST BENGAL 342 DAULAT RAM J MAHARASTRA 343 SHERE P M MAHARASTRA 345 DAVER B