Big Red Rash
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

HIV and the SKIN • Sudden Acute Exacerbations • Treatment Failure DR
2018/08/13 KEY FEATURES • Atypical presentation of common disorders • Severe or exaggerated presentations HIV AND THE SKIN • Sudden acute exacerbations • Treatment failure DR. FREDAH MALEKA DERMATOLOGY UNIVERSITY OF PRETORIA:KALAFONG VIRAL INFECTIONS EXANTHEM OF PRIMARY HIV INFECTION • Exanthem of primary HIV infection • Acute retroviral syndrome • Herpes simplex virus (HSV) • Morbilliform rash (exanthem) : 2-4 weeks after HIV exposure • Varicella Zoster virus (VZV) • Typically generalised • Molluscum contagiosum (Poxvirus) • Pronounced on face and trunk, sparing distal extremities • Human papillomavirus (HPV) • Associated : fever, lymphadenopathy, pharyngitis • Epstein Barr virus (EBV) • DDX: drug reaction • Cytomegalovirus (CMV) • other viral infections – EBV, Enteroviruses, Hepatitis B virus 1 2018/08/13 HERPES SIMPLEX VIRUS(HSV) • Vesicular eruption due to HSV 1&2 • Primary lesion: painful, grouped vesicles on an erythematous base • HIV: attacks are more frequent and severe • : chronic, non-healing, deep ulcers, with scarring and tissue destruction • CLUE: severe pain and recurrences • DDX: syphilis, chancroid, lymphogranuloma venereum • Tzanck smear, Histology, Viral culture HSV • Treatment: Acyclovir 400mg tds 7-10 days • Alternatives: Valacyclovir and Famciclovir • In setting of treatment failure, viral isolates tested for resistance against acyclovir • Alternative drugs: Foscarnet, Cidofovir • Chronic suppressive therapy ( >8 attacks per year) 2 2018/08/13 VARICELLA • Chickenpox • Presents with erythematous papules and umbilicated -

Experience with Molluscum Contagiosum and Associated Inflammatory Reactions in a Pediatric Dermatology Practice the Bump That Rashes
STUDY ONLINE FIRST Experience With Molluscum Contagiosum and Associated Inflammatory Reactions in a Pediatric Dermatology Practice The Bump That Rashes Emily M. Berger, MD; Seth J. Orlow, MD, PhD; Rishi R. Patel, MD; Julie V. Schaffer, MD Objective: To investigate the frequency, epidemiol- (50.6% vs 31.8%; PϽ.001). In patients with molluscum ogy, clinical features, and prognostic significance of in- dermatitis, numbers of MC lesions increased during the flamed molluscum contagiosum (MC) lesions, mollus- next 3 months in 23.4% of those treated with a topical cum dermatitis, reactive papular eruptions resembling corticosteroid and 33.3% of those not treated with a topi- Gianotti-Crosti syndrome, and atopic dermatitis in pa- cal corticosteroid, compared with 16.8% of patients with- tients with MC. out dermatitis. Patients with inflamed MC lesions were less likely to have an increased number of MC lesions Design: Retrospective medical chart review. over the next 3 months than patients without inflamed MC lesions or dermatitis (5.2% vs 18.4%; PϽ.03). The Setting: University-based pediatric dermatology practice. GCLRs were associated with inflamed MC lesion (PϽ.001), favored the elbows and knees, tended to be Patients: A total of 696 patients (mean age, 5.5 years) pruritic, and often heralded resolution of MC. Two pa- with molluscum. tients developed unilateral laterothoracic exanthem– like eruptions. Main Outcome Measures: Frequencies, characteris- tics, and associated features of inflammatory reactions Conclusions: Inflammatory reactions to MC, including to MC in patients with and without atopic dermatitis. the previously underrecognized GCLR, are common. Treat- ment of molluscum dermatitis can reduce spread of MC Results: Molluscum dermatitis, inflamed MC lesions, and via autoinoculation from scratching, whereas inflamed MC Gianotti-Crosti syndrome–like reactions (GCLRs) oc- lesions and GCLRs reflect cell-mediated immune re- curred in 270 (38.8%), 155 (22.3%), and 34 (4.9%) of sponses that may lead to viral clearance. -

Bronchiolitis Obliterans • Mycoplasma Induced Asthma/Wheezing • Resistant Mycoplasma Infection
CROSS CANADA ROUNDS - Long Case Mandeep Walia Clinical Fellow BC Children’s Hospital 21 June, 2018 Long Case History • 10 Y, Boy Feb 8th • Fever- low-moderate grade, rhinorrhea, cough (dry), mild sore throat • Nausea, non bilious vomiting Day 5- worsening cough -dry, sleep disturbance. • Walk in clinic- no wheeze. Prescribed ventolin. Minimal improvement Day 8- redness eyes, purulent discharge, blisters on lips, ulcers on tongue & buccal mucosa. Difficulty to swallow solids. History- cont • No headache, abnormal movements, visual or hearing loss • No chest pain/stridor/ • No diarrhoea. Vomiting stopped after D3 • No hematuria/dysuria. Feb 17 (D10)- BCCH ED : • concerns for extensive oral mucositis, new onset skin rash. Past Hx • Healthy pregnancy. No complications. • Born by SVD, no neonatal resuscitation/NICU stay. • Recurrent OM- evaluated by ENT-not required myringotomy tubes. • Mild eczema. Development - milestones normal Immunization- upto date Allergies- no known Treatment Hx- Tylenol/benadryl/Ventolin. No antibiotics/NSAIDS FHx- Caucasian descent. unremarkable. Social Hx- active in sports. No exposure to pets/smoke Physical exam • Weight- 37.9kg(77centile) Skin- • HR-96/min, RR-30/min , • pink papules, 2-3mm, central • SPO2 94% RA, T-39.2ᵒc, BP115/64 erosion, about 15-20 on trunk, • HEENT- upper & lower extremities. Sparing palms & soles. • B/L conjunctival injection, • purulent discharge MSK-no arthritis • • Lips, buccal mucosa , soft & hard Perianal skin, glans- normal palate-scattered vesicles & superficial erosions. No crusting (serous/hemorrhagic) • B/L ears-normal • No clubbing/lymphadenopathy Systemic Examination • Respiratory - tachyapnea. No retractions/indrawing. B/L air entry decreased. No wheeze/crackles. • CVS-S1 S2 normal. no murmur • PA- no HSM • Neurological - conscious. -

Fundamentals of Dermatology Describing Rashes and Lesions
Dermatology for the Non-Dermatologist May 30 – June 3, 2018 - 1 - Fundamentals of Dermatology Describing Rashes and Lesions History remains ESSENTIAL to establish diagnosis – duration, treatments, prior history of skin conditions, drug use, systemic illness, etc., etc. Historical characteristics of lesions and rashes are also key elements of the description. Painful vs. painless? Pruritic? Burning sensation? Key descriptive elements – 1- definition and morphology of the lesion, 2- location and the extent of the disease. DEFINITIONS: Atrophy: Thinning of the epidermis and/or dermis causing a shiny appearance or fine wrinkling and/or depression of the skin (common causes: steroids, sudden weight gain, “stretch marks”) Bulla: Circumscribed superficial collection of fluid below or within the epidermis > 5mm (if <5mm vesicle), may be formed by the coalescence of vesicles (blister) Burrow: A linear, “threadlike” elevation of the skin, typically a few millimeters long. (scabies) Comedo: A plugged sebaceous follicle, such as closed (whitehead) & open comedones (blackhead) in acne Crust: Dried residue of serum, blood or pus (scab) Cyst: A circumscribed, usually slightly compressible, round, walled lesion, below the epidermis, may be filled with fluid or semi-solid material (sebaceous cyst, cystic acne) Dermatitis: nonspecific term for inflammation of the skin (many possible causes); may be a specific condition, e.g. atopic dermatitis Eczema: a generic term for acute or chronic inflammatory conditions of the skin. Typically appears erythematous, -

Viral Exanthem
Robert E. Kalb, M.D. Buffalo Medical Group, P.C. Phone: (716) 630-1102 Fax: (716) 633-6507 Department of Dermatology 325 Essjay Road Williamsville, New York 14221 Viral Exanthem What is a viral exanthem? An exanthem is a doctor’s word for a rash caused by an infectious organism. In this case, a viral exanthem is a rash caused by a virus. You may be familiar with some viral exanthems and you undoubtedly have had some yourself. One familiar viral exanthem is chickenpox. Other viral exanthems include measles and rubella, for which most people have been immunized against. While measles and rubella may sound unpleasant, the vast majority of the hundreds of other viral exanthems are harmless, yet they may cause short-term discomfort. Just as adults may get colds and experience uncomfortable, yet tolerable symptoms like a runny nose, sore throat, and coughing, viral exanthem’s symptoms include itching and redness and are also uncomfortable, but usually short-lived. They very rarely have emotional, developmental, or physical aftereffects. What are the symptoms of a viral exanthem? The most obvious symptom is the widespread rash, which may be anywhere over the body’s surface. Some viral exanthems have particular patterns that help us with diagnosing their cause. Other rashes may appear random. The rash may itch or it may not. Other symptoms may occur prior to or with the rash; fever, a tired achy feeling, irritability, loss of appetite, headache, and abdominal pain. What is the treatment for a viral exanthem? The treatment is symptom control and patience. You may benefit from an oral or topical antihistamine, or another topical anti-itch medication, as determined by the nature and extent of your problem. -

Wisconsin Childhood Communicable Diseases Wall Chart
WISCONSIN CHILDHOOD COMMUNICABLE DISEASES Disease Name Incubation Period Time Period When Person is Spread by Signs and Symptoms Criteria for Exclusion from School or Group Onsite Control and Prevention Measures Time from exposure to Contagious (AKA, causative agent) symptoms Cold sores Direct contact with open sores Fever, irritability, blisters in mouth, on gums, lips, 2-7 weeks after symptoms appear, virus Exclude until fever-free, child able to control drooling, (Herpes simplex virus) or saliva 2 days to 2 weeks conjunctivitis, keratitis shedding possible without symptoms blisters resolved Mononucleosis Person to person contact with Many months after infection; excretion None, unless illness prevents participation; no contact saliva 30-50 days Fever, sore throat, swollen lymph nodes, fatigue of virus can occur intermittently for life sports until spleen no longer enlarged (Mono, Epstein-Barr virus) For all diseases: Good handwashing and hygiene; avoid Mumps R/V Inhalation of respiratory Fever, swelling and tenderness of parotid glands, Exclude for 5 days after swelling onset (day of swelling kissing, sharing drinks, or utensils, use proper disinfection droplets, direct contact with 12-25 days; headache, earache, painful swollen testicles, From 2 days before to 5 days after onset is day zero); exclude susceptible* contacts from of surfaces and toys (Mumps virus) saliva of infected person usually 16-18 days abdominal pain with swollen ovaries swelling day 12 through day 25 after exposure Mumps: Provide immunization records for exposed -

Oral Manifestations of Systemic Diseases: Overview, Gastrointestinal Diseases, Nutritional Disease 12/09/16, 11:27
Oral Manifestations of Systemic Diseases: Overview, Gastrointestinal Diseases, Nutritional Disease 12/09/16, 11:27 Oral Manifestations of Systemic Diseases Author: Heather C Rosengard, MPH; Chief Editor: Dirk M Elston, MD more... Updated: Jul 27, 2016 Overview The oral cavity plays a critical role in numerous physiologic processes, including digestion, respiration, and speech. It is also unique for the presence of teeth and mucosa. The mouth is frequently involved in conditions that affect the skin, but it is also affected by many systemic diseases. Oral involvement may precede or follow the appearance of findings at other locations. This article is intended as a general overview of conditions with oral manifestations of systemic diseases. It is not intended to provide details about the diagnosis and management of these conditions. Many of these conditions have excellent full- length Medscape Drugs & Diseases articles, which are linked herein. Gastrointestinal Diseases The oral cavity is the portal of entry to the GI tract and is lined with stratified squamous epithelium. The oral cavity is often involved in conditions that affect the GI tract. Both ulcerative colitis (UC) and Crohn disease are classified as inflammatory bowel disease (IBD). While Crohn disease can affect any part of the GI tract (from the oral cavity to the anus), inflammation in UC is generally restricted to the colon and is specifically limited to the mucosa and submucosa. Ulcerative colitis UC is characterized by periods of exacerbation and remission, and, generally, oral lesions coincide with exacerbations of the colonic disease. Lesions in the colon consist of areas of hemorrhage and ulceration, along with abscesses. -

Management of Varicella Zoster Virus (Vzv) Infections
MANAGEMENT OF VARICELLA ZOSTER VIRUS (VZV) INFECTIONS Federal Bureau of Prisons Clinical Guidance DECEMBER 2016 Federal Bureau of Prisons (BOP) Clinical Guidance is made available to the public for informational purposes only. The BOP does not warrant this guidance for any other purpose, and assumes no responsibility for any injury or damage resulting from the reliance thereof. Proper medical practice necessitates that all cases are evaluated on an individual basis and that treatment decisions are patient- specific. Consult the BOP Health Management Resources Web page to determine the date of the most recent update to this document: http://www.bop.gov/resources/health_care_mngmt.jsp Federal Bureau of Prisons Management of VZV Infections Clinical Guidance December 2016 WHAT’S NEW IN THIS DOCUMENT? What is new in the December 2016 version of this document? • Duplication of information is minimized. • Varicella IgM testing is not recommended for either suspected varicella cases or contacts, because of low sensitivity and specificity (see Appendix 1, Varicella Testing). • Procedures for contact investigation have been simplified and clarified (see Appendix 3, Varicella Contact Investigation Checklist). • VariZIG for post-exposure prophylaxis is now commercially available. What was new in the December 2011 version of this document? • A digital Varicella Timeline Calculator (for determining the exposure and infectious periods of an index case and the incubation period of exposed contacts) was added to the BOP website (http://www.bop.gov/resources/health_care_mngmt.jsp). • Treatment of post-herpetic neuralgia associated with herpes zoster was clarified (see Treatment of Herpes Zoster/Shingles in Section 6, Treatment). • It was emphasized that inmates with herpes zoster (shingles) should be housed in a single cell if the secretions from the lesions cannot be easily contained (see Housing Inmates with Varicella or Herpes Zoster in Section 7, Control Measures). -
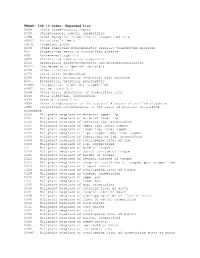
ICD 10 Codes
TNAGD- ICD 10 Codes- Expanded List A408 Other streptococcal sepsis A409 Streptococcal sepsis, unspecified A498 Other bacterial infections of unspecified site A5052 Hutchinson's teeth A5131 Condyloma latum A638 Other specified predominantly sexually transmitted diseases A64 Unspecified sexually transmitted disease A65 Nonvenereal syphilis A690 Necrotizing ulcerative stomatitis B002 Herpesviral gingivostomatitis and pharyngotonsillitis B0222 Postherpetic trigeminal neuralgia B078 Other viral warts B079 Viral wart, unspecified B084 Enteroviral vesicular stomatitis with exanthem B085 Enteroviral vesicular pharyngitis B0860 Parapoxvirus infection, unspecified B0861 Bovine stomatitis B348 Other viral infections of unspecified site B349 Viral infection, unspecified B370 Candidal stomatitis B954 Other streptococcus as the cause of diseases classified elsewhere B955 Unspecified streptococcus as the cause of diseases classified elsewhere C000 Malignant neoplasm of external upper lip C001 Malignant neoplasm of external lower lip C002 Malignant neoplasm of external lip, unspecified C003 Malignant neoplasm of upper lip, inner aspect C004 Malignant neoplasm of lower lip, inner aspect C005 Malignant neoplasm of lip, unspecified, inner aspect C006 Malignant neoplasm of commissure of lip, unspecified C008 Malignant neoplasm of overlapping sites of lip C009 Malignant neoplasm of lip, unspecified C01 Malignant neoplasm of base of tongue C020 Malignant neoplasm of dorsal surface of tongue C021 Malignant neoplasm of border of tongue C022 Malignant neoplasm -

RASH in INFECTIOUS DISEASES of CHILDREN Andrew Bonwit, M.D
RASH IN INFECTIOUS DISEASES OF CHILDREN Andrew Bonwit, M.D. Infectious Diseases Department of Pediatrics OBJECTIVES • Develop skills in observing and describing rashes • Recognize associations between rashes and serious diseases • Recognize rashes associated with benign conditions • Learn associations between rashes and contagious disease Descriptions • Rash • Petechiae • Exanthem • Purpura • Vesicle • Erythroderma • Bulla • Erythema • Macule • Enanthem • Papule • Eruption Period of infectivity in relation to presence of rash • VZV incubates 10 – 21 days (to 28 d if VZIG is given • Contagious from 24 - 48° before rash to crusting of all lesions • Fifth disease (parvovirus B19 infection): clinical illness & contagiousness pre-rash • Rash follows appearance of IgG; no longer contagious when rash appears • Measles incubates 7 – 10 days • Contagious from 7 – 10 days post exposure, or 1 – 2 d pre-Sx, 3 – 5 d pre- rash; to 4th day after onset of rash Associated changes in integument • Enanthems • Measles, varicella, group A streptoccus • Mucosal hyperemia • Toxin-mediated bacterial infections • Conjunctivitis/conjunctival injection • Measles, adenovirus, Kawasaki disease, SJS, toxin-mediated bacterial disease Pathophysiology of rash: epidermal disruption • Vesicles: epidermal, clear fluid, < 5 mm • Varicella • HSV • Contact dermatitis • Bullae: epidermal, serous/seropurulent, > 5 mm • Bullous impetigo • Neonatal HSV • Bullous pemphigoid • Burns • Contact dermatitis • Stevens Johnson syndrome, Toxic Epidermal Necrolysis Bacterial causes of rash -

Blanching Rashes
BLANCHING RASHES Facilitators Guide Author Aoife Fox (Edits by the DFTB Team) [email protected] Author Aoife Fox Duration 1-2h Facilitator level Senior trainee/ANP and above Learner level Junior trainee/Staff nurse and Senior trainee/ANP Equipment required None OUTLINE ● Pre-reading for learners ● Basics ● Case 1: Chicken Pox (15 min) ● Case 2: Roseola (15 min) ● Case 3: Scarlet fever (20 min) ● Case 4: Kawasaki disease (including advanced discussion) (25 min) ● Game ● Quiz ● 5 take home learning points PRE-READING FOR LEARNERS BMJ Best Practice - Evaluation of rash in children PEDS Cases - Viral Rashes in Children RCEM Learning - Common Childhood Exanthems American Academy of Dermatology - Viral exanthems 2 Infectious Non-infectious Blanching Blanching Staphylococcus scalded skin syndrome Sunburn Impetigo Eczema Bullous impetigo Urticaria Eczema hepeticum Atopic dermatitis Measles Acne vulgaris Glandular fever/infectious mononucleosis Ichthyosis vulgaris keratosis pilaris Hand foot and mouth disease Salmon patch Erythema infectiosum/Fifth disease Melasma Chickenpox (varicella zoster) Napkin rash Scabies Seborrhoea Tinea corporis Epidermolysis bullosa Tinea capitis Kawasaki disease Molluscum contagiosum Steven-Johnson syndrome Scarlet fever Steven-Johnson syndrome/toxic epi- Lyme disease dermal necrolysis Congenital syphilis Erythema multiforme Congenital rubella Erythema nodosum Herpes simplex Roseola (sixth disease) Non-blanching Epstein-Barr virus Port-wine stain Pityriasis rosea Henoch-Schoenlein purpura Idiopathic thrombocytopenia Acute leukaemia Haemolytic uremic syndrome Trauma Non-blanching Mechanical (e.g. coughing, vomiting – in Meningococcal rash distribution of superior vena cava) 3 BASE Key learning points Image: used with gratitude from Wikipedia.org Definitions/rash description: ● Macule: a flat area of colour change <1 cm in size (e.g., viral exanthem [such as measles and rubella], morbilliform drug eruption). -

Differential Diagnosis of Viral Exanthemas
The Open Vaccine Journal, 2010, 3, 65-68 65 Open Access Differential Diagnosis of Viral Exanthemas Juan José Garcia Garcia* Paediatric Service, Sant Joan de Déu Hospital, University of Barcelona Abstract: This article describes the differential diagnosis of maculopapular rashes, which can be divided into three large groups: classic rashes, nonspecific rashes and paraviral eruptions, the last two of which can be grouped together as atypical rashes. The differential diagnosis of maculopapular rash depends on the setting and the percentage of the population vaccinated. The diagnosis is broad and includes infectious processes and other etiologies. A correct diagnostic orientation requires the availability of the relevant epidemiological data which will aid the suspicion of a specific etiology. Keywords: Measles, Rubella, Scarlet fever, Roseola, Infectious mononucleosis, Erythema infectiosum, Paraviral eruption. INTRODUCTION with any of the classic rashes identified the causal agent in 76 (68%) cases, with the most-frequent causes being viruses Maculopapular rashes can be divided into three large (28.6%) and drugs (22.3%) [3]. In macular or maculopapular groups: classic rashes, nonspecific rashes and paraviral rashes, the type of rash most-frequently found (66.1%), the eruptions, the last two of which can be grouped together as main causes were drugs (18.7%) and viruses (17%). atypical rashes. With respect to measles and rubella, the differential diag- The six classic rashes are measles, rubella, scarlet fever, nosis should be made with other infectious exanthematic exanthem subitum, erythema infectiosum and varicella. All, diseases, drug reactions and Kawasaki disease. except varicella, are maculopapular and can thus be consid- ered within the same differential diagnosis.