Midline As a Landmark for the Position of the Superior Sagittal Sinus on the Cranial Vault: an Anatomical and Imaging Study Cassius Vinicius C
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

CHAPTER 8 Face, Scalp, Skull, Cranial Cavity, and Orbit
228 CHAPTER 8 Face, Scalp, Skull, Cranial Cavity, and Orbit MUSCLES OF FACIAL EXPRESSION Dural Venous Sinuses Not in the Subendocranial Occipitofrontalis Space More About the Epicranial Aponeurosis and the Cerebral Veins Subcutaneous Layer of the Scalp Emissary Veins Orbicularis Oculi CLINICAL SIGNIFICANCE OF EMISSARY VEINS Zygomaticus Major CAVERNOUS SINUS THROMBOSIS Orbicularis Oris Cranial Arachnoid and Pia Mentalis Vertebral Artery Within the Cranial Cavity Buccinator Internal Carotid Artery Within the Cranial Cavity Platysma Circle of Willis The Absence of Veins Accompanying the PAROTID GLAND Intracranial Parts of the Vertebral and Internal Carotid Arteries FACIAL ARTERY THE INTRACRANIAL PORTION OF THE TRANSVERSE FACIAL ARTERY TRIGEMINAL NERVE ( C.N. V) AND FACIAL VEIN MECKEL’S CAVE (CAVUM TRIGEMINALE) FACIAL NERVE ORBITAL CAVITY AND EYE EYELIDS Bony Orbit Conjunctival Sac Extraocular Fat and Fascia Eyelashes Anulus Tendineus and Compartmentalization of The Fibrous "Skeleton" of an Eyelid -- Composed the Superior Orbital Fissure of a Tarsus and an Orbital Septum Periorbita THE SKULL Muscles of the Oculomotor, Trochlear, and Development of the Neurocranium Abducens Somitomeres Cartilaginous Portion of the Neurocranium--the The Lateral, Superior, Inferior, and Medial Recti Cranial Base of the Eye Membranous Portion of the Neurocranium--Sides Superior Oblique and Top of the Braincase Levator Palpebrae Superioris SUTURAL FUSION, BOTH NORMAL AND OTHERWISE Inferior Oblique Development of the Face Actions and Functions of Extraocular Muscles Growth of Two Special Skull Structures--the Levator Palpebrae Superioris Mastoid Process and the Tympanic Bone Movements of the Eyeball Functions of the Recti and Obliques TEETH Ophthalmic Artery Ophthalmic Veins CRANIAL CAVITY Oculomotor Nerve – C.N. III Posterior Cranial Fossa CLINICAL CONSIDERATIONS Middle Cranial Fossa Trochlear Nerve – C.N. -

Torcular Herophili)Ÿ W
Neuroanatomy, 2002, Volume1, Page 14. Letter to the Editor Published online November 7, 2002 © neuroanatomy.org R. Shane Tubbs We would like to clarify a commonly misunderstood term (torcular Herophili)Ÿ W. Jerry Oakes that has infiltrated all fields associated with neuroanatomy e.g. neurosurgery, neurology, neurosciences. The term torcular (wine press) is an incorrect version of the original Greek word (a canal or gutter) [1]. Herophili is after the celebrated Greek physician/anatomist Herophilus (335 B.C.-280 B.C.) born in Chalcedon which is now Kadikoy, Turkey. Herophilus is known as the father of anatomy because he was the first to base his conclusions on dissection of the human body. Herophilus studied the brain, recognizing it as the center Pediatric Neurosurgery, Children’s Hospital, Birmingham, Alabama 35233 USA of the nervous system. The original term was meant to describe the concavity on the internal aspect of the occipital bone that housed the confluence of sinuses. However, over time this term has been used incorrectly as an interchangable term with the confluence of sinuses. Almost every textbook of anatomy with few exceptions, that we reviewed, interchange these terms with no distinction [e.g. 2-4]. True these two entities are intimately related Correspondence Address but clearly represent different anatomical structures. Just as other venous sinuses erode the inner table of the skull producing same named sulci or R. Shane Tubbs, Pediatric Neurosurgery ACC 400, 1600 7th Ave grooves e.g. the transverse sinus sulcus, the confluence of sinuses (formed by South, Birmingham, Alabama 35233 USA the superior sagittal, straight, occipital, and transverse sinuses) erode the Phone: 205-939-9914 Fax: 205-939-9972 occipital bone where the major venous sinus tributaries congregate thus forming E-mail: [email protected] the torcular Herophili. -

Muscle Insertion Line As a Simple Landmark to Identify The
Original Article Muscle Insertion Line as a Simple Landmark To Identify the Transverse Sinus When Neuronavigation Is Unavailable Juri Kivelev1, Riku Kivisaari2, Mika Niemela¨ 2, Juha Hernesniemi2 - OBJECTIVE: Skull opening in occipital and suboccipital venous outflow disturbances, and increased intracranial pressure. regions might be associated with risk of damage to the When operating in a sitting position, inadvertent sinus opening transverse venous sinus and the confluence of sinuses. We causes air embolism. Modern frameless neuronavigation systems analyze the value of magnetic resonance (MR) imaging in are useful in localizing venous sinuses before craniotomy, but they localizing the venous sinuses in relation to the superior are not yet widely available due to high price. Furthermore, when surgery is performed in a sitting or prone position, some diffi- muscle insertion line (MIL) on the occipital bone. culties with neuronavigation may occur. Many studies have been - METHODS: We retrospectively analyzed head MR im- conducted regarding the role of external skull bony landmarks in ages of 100 consecutive patients imaged for any reason localization of posterior venous sinuses. Our study is the first to from 1 January 2013. All MR images were interpreted by a analyze a simple and effective way to localize the venous sinuses in radiologist (R.K.). The superior MIL was identified at the relation to the superior muscle insertion line (MIL) on occipital bone. In this region, a surgical view after skin incision includes midline and on both midpupillar lines, which represent the (from cephalad to caudal) the occipital bone surface, MIL, and most frequent sites of skin incision and craniotomy (me- muscles covered by the superficial layer of cervical fascia. -

Dural Venous Sinuses Dr Nawal AL-Shannan Dural Venous Sinuses ( DVS )
Dural venous sinuses Dr Nawal AL-Shannan Dural venous sinuses ( DVS ) - Spaces between the endosteal and meningeal layers of the dura Features: 1. Lined by endothelium 2. No musculare tissue in the walls of the sinuses 3. Valueless 4.Connected to diploic veins and scalp veins by emmissary veins .Function: receive blood from the brain via cerebral veins and CSF through arachnoid villi Classification: 15 venous sinuses Paried venous sinuses Unpaired venous sinuses ( lateral in position) • * superior sagittal sinus • * cavernous sinuses • * inferior sagittal sinus • * superior petrosal sinuses • * occipital sinus • * inferior petrosal sinuses • * anterior intercavernous • * transverse sinuses • sinus * sigmoid sinuses • * posterior intercavernous • * spheno-parietal sinuses • sinus • * middle meningeal veins • * basilar plexuses of vein SUPERIOR SAGITTAL SINUS • Begins in front at the frontal crest • ends behind at the internal occipital protuberance diliated to form confluence of sinuses and venous lacunae • • The superior sagittal sinus receives the following : • 1- Superior cerebral veins • 2- dipolic veins • 3- Emissary veins • 4- arachnoid granulation • 5- meningeal veins Clinical significance • Infection from scalp, nasal cavity & diploic tissue • septic thrombosis • CSF absorption intra cranial thrombosis (ICT) • Inferior sagittal sinus - small channel occupy • lower free magin of falx cerebri ( post 2/3) - runs backward and • joins great cerebral vein at free margin of tentorium cerebelli to form straight sinus. • - receives cerebral -

An Anatomico-Radiological Study of the Grooves for Occipital Sinus in the Posterior Cranial Fossa
Bratisl Lek Listy 2008; 109 (11) 520524 COMPARATIVE ANATOMY An anatomico-radiological study of the grooves for occipital sinus in the posterior cranial fossa Srijit Das1, Azian Abd Latiff1, Farihah Haji Suhaimi1, Faizah Bt Othman1, Mohd F Yahaya1, Fairus Ahmad1, Hamzaini Abdul Hamid2 Department of Anatomy, Universiti Kebangsaan Malaysia, Jalan Raja Muda Abdul Aziz, Kuala Lumpur, Malaysia. [email protected] Abstract: Background: The occipital sinus (OS) lies in the attached margin of the falx cerebelli in the internal occipital crest of the occipital bone. The OS extends from the foramen magnum to the confluence of sinuses. Standard textbooks and research reports do not describe in detail any variation in the groove for the occipital sinus. Methods: In the present study, we examined a total of 50 human dried skulls for the groove of OS and its possible variations. We also performed an osteological study supplemented with digital X ray and CT scan. Results: Out of 50 skull specimens, a single case with two grooves for OS was observed (2 %). The two grooves for OS traversed as two limbs from the foramen magnum to join the other at the internal occipital protuberance. An accessory faint groove was also found at the lateral aspect of the left limb. Interestingly, in the same specimen, the superior sagittal sinus instead of continuing as right transverse sinus, continued as left transverse sinus. The X ray and CT scan of the anomalous bone specimen were compared to those of the normal bone specimen. Discussion: To the best of our knowledge, this is the first anatomico-radiological study of multiple OS groove with associated anomalies. -

Concussion and OMT Sports Medicine: Screening and Treating
Concussion and OMT Sports Medicine: Screening and Treating Sheldon C. Yao, D.O. March 14, 2019 Objectives • Define and discuss concussion diagnosis and screening. • Discuss how osteopathic manipulative medicine can be applied help address concussion injuries. • Discuss the application of osteopathic manipulation through the autonomic nervous, lymphatic, and musculoskeletal systems. • Review Fulford’s shock release, dural release, and venous sinus drainage and how it can help concussion symptoms. Concussion • Form of mild traumatic brain injury following a biomechanical force • Results in the rapid onset of short-lived impairment of neurologic function • LOC not necessary and does not correlate with severity • Centers for Disease Control and Prevention estimate that as many as 3.8 million sport- related traumatic brain injuries occur annually Pathophysiology • Concussion results from a rapid rotational acceleration of the brain which causes a shear strain which then induces immediate changes in brain neurochemistry : – Neuronal depolarization – Local lactic acid accumulation – Decreased cerebral blood flow with mismatch of cerebral glucose supply and demand Evaluation - History • Mechanism • Symptoms • Prior concussion • LOC • Change in mental status • Seizures Common Symptoms Evaluation: Sideline Assessment • Sideline eval: – ABC’s, C-spine evaluation – Neurologic exam – SPORT CONCUSSION ASSESSMENT TOOL (SCAT-5) – Balance Errors Scoring System (BESS) – King-Devick test • Suspected concussion = remove from play • Serial exams on sideline -

The Cranial Dura Mater: a Review of Its History, Embryology, and Anatomy
Childs Nerv Syst (2012) 28:827–837 DOI 10.1007/s00381-012-1744-6 REVIEW PAPER The cranial dura mater: a review of its history, embryology, and anatomy Nimer Adeeb & Martin M. Mortazavi & R. Shane Tubbs & Aaron A. Cohen-Gadol Received: 14 February 2012 /Accepted: 23 March 2012 /Published online: 15 April 2012 # Springer-Verlag 2012 Abstract mother) and umm al-raqiqah (thin mother). These terms were Introduction The dura mater is important to the clinician as then literally translated into Latin by the twelfth century Italian a barrier to the internal environment of the brain, and surgi- monk Stephen of Antioch, as the dura (hard) mater (Fig. 1), and cally, its anatomy should be well known to the neurosurgeon the pia (pious) mater. The term pia was a misnomer and should and clinician who interpret imaging. have been replaced by tenue (from tennus meaning thin), but Methods The medical literature was reviewed in regard to the term pia has persisted. The first introduction of the word the morphology and embryology of specifically, the intra- arachnoid (spider-like) mater was by Herophilus in the third cranial dura mater. A historic review of this meningeal layer century B.C., who also described its relation to the ventricles. It is also provided. was later described by the Dutch anatomist Frederik Ruysch in Conclusions Knowledge of the cranial dura mater has a rich the seventeenth century. The term mater is derived from ma- history. The embryology is complex, and the surgical anat- (from matru meaning mother) and the suffix -ter indicating a omy of this layer and its specializations are important to the state of being [41, 53]. -
27. Veins of the Head and Neck
GUIDELINES Students’ independent work during preparation to practical lesson Academic discipline HUMAN ANATOMY Topic VEINS OF THE HEAD AND NECK 1. The relevance of the topic: Knowledge of the anatomy of the veins of head and neck is a base of clinical thinking and differential diagnosis for the doctor of any specialty, but, above all, dentists, neurologists and surgeons who operate in areas of the neck or head. 2. Specific objectives - demonstrate superior vena cava, right and left brachiocephalic, subclavian, internal and external jugular, anterior jugular veins and venous angles. - demonstrate dural sinuses, veins of the brain. - demonstrate pterygoid plexus, retromandibular, facial veins and other tributaries of extracranial part of internal jugular vein. - demonstrate external jugular vein. - identify and demonstrate anastomoses on the head and neck. 3. Basic level of preparation Student should know and be able to: 1. To demonstrate the structural features of the cervical vertebrae. 2. To demonstrate the anatomical lesions of external and internal base of the skull. 3. To demonstrate the muscles of the head and neck. 4. To demonstrate the divisions of the brain. 4. Tasks for independent work during preparation for practical lessons 4.1. A list of the main terms, parameters, characteristics that need to be learned by student during the preparation for the lesson Term Definition JUGULAR VEINS Veins that take deoxygenated blood from the head to the heart via the superior vena cava. INTERNAL JUGULAR VEIN Starts from the sigmoid sinus of the dura mater and receives the blood from common facial vein. The internal jugular vein runs with the common carotid artery and vagus nerve inside the carotid sheath. -

Cerebral Venous Malformation As a Cause of Neonatal Intra-Ventricular
ogy: iol Cu ys r h re P n t & R y e s Anatomy & Physiology: Current m e o a t r a c n h A Research Talbert, Anat Physiol 2016, 6:2 ISSN: 2161-0940 DOI: 10.4172/2161-0940.1000202 Review Article Open Access Cerebral Venous Malformation as a Cause of Neonatal Intra-Ventricular Haemorrhage and Unexplained Infant Subdural Haemorrhage David Talbert* Imperial College, London, United Kingdom *Corresponding author: David Talbert, Imperial College, Institute of Reproductive and Developmental Biology, Imperial College School of Medicine, Queen Charlotte’s Hospital, London W12 ONN, U.K., E-mail: [email protected] Rec date: Feb 01, 2016; Acc date: Feb 16, 2016; Pub date: Feb 19, 2016 Copyright: © 2016 Talbert D. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract An Intra-ventricular Haemorrhage (IVH) is a bleeding into the brain’s ventricular system. Most intra-ventricular haemorrhages occur in the first 72 hours after birth. They originate in a layer of tissue (Germinal Matrix), under the lining of the ventricles (Ependymal), while it is in the process of manufacturing neurons and glia. This has normally regressed by term but may still be active in premature infants. Pathological investigations have found accumulations of peri-venous plasma and blood suggesting that excessive cerebral venous pressure has disrupted vessels, initiating the intra-ventricular bleeding observed. This has led to unsuccessful searches for evidence of A-V shunts within the developing cerebrum, or loss of auto regulation in arterioles, producing excessive cerebral venous hypertension. -

Study of Posterior Condylar Foramen in Dry Human Skulls
Original Research Article DOI: 10.18231/2394-2126.2017.0011 Study of posterior condylar foramen in dry human skulls Manoj Borkute1,*, K. Shyam Kishore2 1Assistant Professor, 2Additional Professor, Dept. of Anatomy, Seth Medical College & KEM Hospital, Parel, Mumbai *Corresponding Author: Email: [email protected] Abstract Introduction: Posterior condylar foramen is the most constantly present emissary foramen in human skull. It is also considered as largest emissary foramen present in humans. Of the two large emissary veins of posterior cranial fossa, one of them i.e. posterior condylar vein passes through posterior condylar foramen. Condylar veins are also important channels of venous drainage for posterior cranial fossa region. Emissary veins are important in equalising intracranial pressure. They can act as safety valves in cerebral congestion. Method: Material for this study consists of 100 dry adult skulls obtained from two teaching institutes in Maharashtra state. These skulls were carefully observed for posterior condylar foramen. Whether foramen was present unilaterally or bilaterally or was absent on both sides was noted. Result: Posterior condylar foramen was present on both sides (bilaterally) in 58 skulls. In 15 skulls it was present only on right side where as in 10 skulls it was present only on left side. Foramen was found to be absent on both sides in 17 skulls. When present unilaterally it was more common on right side than left. Conclusion: Posterior condylar foramen was not only important from anthropological point of view but also important for clinicians and surgeons who deal with posterior cranial fossa region. Condylar vein (posterior) and posterior condylar foramen (canal) both are important surgical landmarks for different skull base approaches described. -
Powerpoint Handout: Lab 1, Part B: Dural Folds, Dural Sinuses, and Arterial Supply to Head and Neck
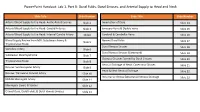
PowerPoint Handout: Lab 1, Part B: Dural Folds, Dural Sinuses, and Arterial Supply to Head and Neck Slide Title Slide Number Slide Title Slide Number Arterial Blood Supply to the Head: Aortic Arch Branches Slide 2 Innervation of Dura Slide 14 Arterial Blood Supply to the Head: Carotid Arteries Slide 3 Emissary Veins & Diploic Veins Slide 15 Arterial Blood Supply to the Head: Internal Carotid Artery Slide4 Cerebral & Cerebellar Veins Slide 16 Blood Supply Review from MSI: Subclavian Artery & Named Dural Folds Slide 5 Slide 17 Thyrocervical Trunk Dural Venous Sinuses Slide 18 Vertebral Artery Slide 6 Dural Venous Sinuses (Continued) Slide 19 Subclavian Steal Syndrome Slide 7 Osseous Grooves formed by Dural Sinuses Slide 20 Thyrocervical Trunk Slide 8 Venous Drainage of Head: Cavernous Sinuses Slide 21 Review: Suprascapular Artery Slide 9 Head & Neck Venous Drainage Slide 22 Review: Transverse Cervical Artery Slide 10 Intracranial Versus EXtracranial Venous Drainage Slide 23 Middle Meningeal Artery Slide 11 Meningeal Layers & Spaces Slide 12 Cranial Dura, Dural Folds, & Dural Venous Sinuses Slide 13 Arterial Blood Supply to the Head: Aortic Arch Branches The head and neck receive their blood supply from https://3d4medic.al/PXGmbxEt branches of the right and left common carotid and right and left subclavian arteries. • On the right side, the subclavian and common carotid arteries arise from the brachiocephalic trunk. • On the left side, these two arteries originate from the arch of the aorta. Arterial Blood Supply to the Head: Carotid Arteries On each side of the neck, the common carotid arteries ascend in the neck to the upper border of the thyroid cartilage (vertebral level C3/C4) where they divide into eXternal and internal carotid arteries at the carotid bifurcation. -

A Peculiar Case of Dural Venous Sinuses with Resulting Atypical Bony Markings in Posterior Cranial Fossa
International Journal of Research in Medical Sciences Khorwal G et al. Int J Res Med Sci. 2017 Jun;5(6):2830-2832 www.msjonline.org pISSN 2320-6071 | eISSN 2320-6012 DOI: http://dx.doi.org/10.18203/2320-6012.ijrms20172500 Case Report A peculiar case of dural venous sinuses with resulting atypical bony markings in posterior cranial fossa Gitanjali Khorwal*, Sunita Kalra Department of Anatomy, University College of Medical Sciences, Delhi, India Received: 20 March 2017 Accepted: 19 April 2017 *Correspondence: Dr. Gitanjali Khorwal, E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT A paramedian or midline suboccipital approach for craniotomies and craniectomies is commonly employed for decompression or tumour resections from posterior cranial fossa. The reference for midline is taken as the line joining the nasion and inion on the surface of the skull which is the estimated position of superior sagittal sinus. In the interior, the internal occipital protuberance is the site of confluence of sinuses which presents a spectrum of variations. An unusual pattern of drainage of dural venous sinuses was observed at the site of customary confluence during routine dissection of head region for undergraduate medical students in a sixty-year-old female cadaver. The superior sagittal sinus continued as right transverse sinus as usual but it was connected to the left transverse sinus through a venous channel.