Is It More Than Copd? 2019; 24(3):227-237
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Bronchopulmonary Hygiene Protocol
BRONCHOPULMONARY HYGIENE PROTOCOL MD order for Bronchopulmonary Hygiene Protocol Evaluate Indications: 9 Difficulty with secretion clearence with sputum production > 25 ml/day 9 Evidence of retained secretions 9 Mucus plug induced atelectasis 9 Foreign body in airway 9 Diagnosis of cystic fibrosis, bronchiectasis, or cavitating lung disease Yes Does contraindication or potential hazard exist? No Address any immediate need and contact MD/RN Select method based on: 9 Patient preference/comfort/pain avoidance 9 Observation of effectiveness with trial 9 History with documented effectiveness Method may include: 9 Manual chest percussion and positioning 9 External chest wall vibration 9 Intrapulmonary percussion Adminster therapy no less than QID and PRN, supplemented by suctioning for all patients with artificial airways Re-evaluate pt every 24 hours, and 24 hours after discontinued Assess Outcomes: Goals achieved? 9 Optimal hydration with sputum production < 25 ml/day 9 Breath sounds from diminished to adventitious with ronchi cleared by cough 9 Patient subjective impression of less retention and improved clearance 9 Resolution/Improvement in chest X-ray 9 Improvement in vital signs and measures of gas exchange 9 If on ventilator, reduced resistance and improved compliance Care Plan Considerations: Discontinue therapy if improvement is observed and sustained over a 24-hour period. Patients with chronic pulmonary disease who maintain secretion clearance in their home environment should remain on treatment no less than their home frequency. Hyperinflation Protocol should be considered for patients who are at high risk for pulmonary complications as listed in the indications for Hyperinflation Protocol. 5/5/03 (Jan Phillips-Clar, Rick Ford, Judy Tietsort, Jay Peters, David Vines) AARC References for Bronchopulmonary Algorithm 1. -

Teaching Cases of the Month
Teaching Cases of the Month A 60-Year Old Man Presenting With Yellow Nail Syndrome Ariel Modrykamien MD and Omar Minai MD Introduction Blood total protein was 5.2 g/dL, and lactate dehydroge- nase was 350 U/L. His FEV1 was 64% of predicted, forced Yellow nail syndrome is a rare disorder of unclear eti- vital capacity was 60% of predicted, the ratio of FEV1 to ology. Since its original description by Samman and White,1 forced vital capacity was 0.81, and his diffusion capacity many other reports and associations have been described. for carbon monoxide was 97% of predicted. Current evidence suggests that its pathologic mechanism Echocardiogram revealed normal cavities and valve is based on lymphatic dysfunction, which is thought to be function. Left-side thoracentesis obtained a cloudy pleural acquired rather than congenital. However, our understand- fluid with total protein 3.9 g/dL, lactate dehydrogenase ing of its pathogenesis is still speculative, as it relies on 144 U/L, glucose 100 mg/dL, and pH 7.6, with 79% lym- anecdotal observations. We report a case of a man who phocytes. Pleural fluid cultures for bacterial, fungal, and presented with dry cough, shortness of breath, bilateral acid-fast bacilli were negative. Cytology was negative for lower-extremity edema, and pleural effusion. Yellow nail malignant cells. Flow cytometry was negative for chronic syndrome was diagnosed. lymphoproliferative disorders. Tuberculosis skin test was also negative. Case Summary Radiology Findings A 60-year-old man presented with 2 months of persis- tent dry cough. He noticed dyspnea with moderate effort, Chest radiograph revealed a left-side pleural effusion such as walking 2–3 blocks, and bilateral lower-extremity (Fig. -

Touching Lives and Advancing Patient Care Through Education PASSY
PASSY-MUIR® TRACHEOSTOMY & VENTILATOR SWALLOWING AND SPEAKING VALVES INSTRUCTION BOOKLET Passy-Muir® Tracheostomy & Ventilator Passy-Muir® Tracheostomy & Ventilator Swallowing and Speaking Valve Swallowing and Speaking Valve PMV® 005 (white) PMV® 007 (Aqua Color™) 15mm l.D./23mm O.D. 15mm l.D./22mm O.D. Dual Taper Passy-Muir® Low Profile Tracheostomy & Passy-Muir® Low Profile Tracheostomy & Ventilator Swallowing and Speaking Valve Ventilator Swallowing and Speaking Valve PMV® 2000 (clear) PMV® 2001 (Purple Color™) 15mm l.D./23mm O.D. 15mm l.D./23mm O.D. For technical questions regarding utilization of the Passy-Muir Valves, please contact our respiratory and speech clinical specialists. Touching Lives and Advancing Patient Care Through Education CONTENTS OF PMV® PATIENT CARE KIT: This package contains one of the following Passy-Muir® Tracheostomy & Ventilator Swallowing and Speaking Valves (PMVs): PMV 005 (white), PMV 007 (Aqua Color™), PMV 2000 (clear), or PMV 2001 (Purple Color™) and Instruction Booklet, Patient Handbook, PMV Storage Container, Patient Parameters Chart Label, and Warning Labels for use on the trach tube pilot line, chart and at bedside. A PMV Secure-It® is also included in the PMV 2000 (clear) and PMV 2001 (Purple Color) Patient Care Kit. The PMV 005 (white), PMV 007 (Aqua Color), PMV 2000 (clear) and PMV 2001 (Purple Color) are not made with natural rubber latex. Contents of PMV Patient Care Kit are non-sterile. READ ALL WARNINGS, PRECAUTIONS AND INSTRUCTIONS CAREFULLY PRIOR TO USE: INSTRUCTIONS FOR USE The following instructions are applicable to the PMV 005 (white), PMV 007 (Aqua Color), PMV 2000 (clear) and PMV 2001 (Purple Color) unless otherwise indicated. -

Clinical and Team Management in the COVID-ICU: Successful Strategies from the First Weeks
Emory Critical Care Center Emory ECMO Center Clinical and team management in the COVID-ICU: Successful strategies from the first weeks Grand Rounds University of Rochester SMD, Dept of Pediatrics Mark Caridi-Scheible, MD Emory Critical Care Center, Atlanta, GA Emory Critical Care Center Emory ECMO Center 2009 Emory Critical Care Center Emory ECMO Center Introduction • URSMD Grad • Critical Care and Cardiothoracic Anesthesia, Emory University Hospital • Large academic hospital system with high acuity • Initial team of four physicians on-service in 3 different units (luck of the draw), now 7 units • Helped coordinate best practices efforts since • Co-credit to my starting comrades, Dr. Sara Auld, Dr. Will Bender and Dr. Lisa Daniel, and numerous others for their efforts since Emory Critical Care Center Emory ECMO Center Objectives and Caveats • Aimed for those directly providing care to critically ill patients • Extrapolate points for floor care • Adult population only • Practical, observable, common sense and within standards of care • Not going to rehash freely available reports • Observations not rigorously validated • Outcomes likely to vary based on patient mix, location and resources available • Have to go fast, more information on slides than can discuss • More than anything: there is hope and things we can do better Emory Critical Care Center Emory ECMO Center Our starting points 1. The best practice critical care with maximum delivery 2. No luxury of time, get them better FAST for: • Sake of patient’s chance of recovery • Sake of -

Knowledge on Pulmonary Hygiene and Sociodemographic Factors Affecting It Among Health Professionals Working in Two Government Hospitals, North East Ethiopia
IOSR Journal of Nursing and Health Science (IOSR-JNHS) e-ISSN: 2320–1959.p- ISSN: 2320–1940 Volume 6, Issue 5 Ver. IV. (Sep. -Oct .2017), PP 78-81 www.iosrjournals.org Knowledge on Pulmonary Hygiene and Sociodemographic Factors affecting it among Health Professionals working in Two Government Hospitals, North East Ethiopia Prema Kumara,1 Yemiamrew Getachew,2 Wondwossen Yimam3 1Assistant Professor, Department of Comprehensive Nursing, College of Medicine and Health Sciences 2Head, Department of Comprehensive Nursing, College of Medicine and Health Sciences 3Dean, School of Nursing and Midwifery, College of Medicine and Health Sciences Wollo University, Ethiopia Introduction: Pulmonary hygiene is formerly referred to as pulmonary toilet which is a set of methods used to clear mucus and secretions from the airways and it is depends on consistent clearance of airway secretions. Objective: To determine the level of knowledge and to identify the socio-demographic factors affecting knowledge on pulmonary hygiene among Health Professionals. Methodology: Institution based cross sectional study design was employed among one hundred twelve health professionals using systematic random sampling technique. The collected data were analyzed using descriptive and inferential statistics. Results: The mean knowledge score of the total sample was 13.80 (+ 3.01 SD). Subjects who scored above the mean value were categorized as having good level of knowledge. But only 37 (33 %) study participants had good knowledge about pulmonary hygiene and rest 67 % had poor knowledge. In the multivariable logistic analysis, Married subjects were 3.7 times (AOR = 3.7, CI=1.38, 10.04) more likely to have good knowledge as compared to single individuals. -

Respiratory Therapy Handbook
WASHINGTON STATE COMMUNITY COLLEGE RESPIRATORY THERAPY STUDENT HANDBOOK 2020-2021 Written: July, 1996 Revised: December, 2020 TABLE OF CONTENTS Statement of Non-Discrimination…………………………………………………………………………….. 2 Introduction……………………………………………………………………………………………………………..3 Goal………………………………………………………………………………………………………………………5-6 Accreditation……………………………………………………………………………………………………………6 Program Organization………………………………………………………………………………………………7 Plan for Consistency of Clinical Instruction & Evaluation of Clinical courses, Preceptors & Clinical Sites…………………………………………………………………………………………………………9 STUDENT POLICIES Course of Study………………………………………………………………………………………………………11 Student Schedule/Class sessions……………………………………………………………………………..11 Clinical Experiences…………………………………………………………………………………………..11-12 Tardiness……………………………………………………………………………………………………………….12 Absenteeism, Clinical…………………………………………………………………………………………12-13 Absenteeism, Classroom………………………………………………………………………………………….13 Absenteeism, Lab……………………………………………………………………………………………….13-14 Clinical Evaluations……………………………………………………………………………………………15-16 Clinical Competency…………………………………………………………………………………………..17-20 ACADEMIC POLICIES Clinical Evaluation Forms…………………………………………………………………………………..15-16 Clinical Competency Evaluation………………………………………………………………………….17-20 Promotion………………………………………………………………………………………………………………21 Evaluation………………………………………………………………………………………………………………21 Remediation …………………………………………………………………………………………………………..22 Probation/Dismissal……………………………………………………………………………………………….22 Leave of Absence…………………………………………………………………………………………………….22 -

Suction of the Patient with an Artificial Airway Effective: 11/07/94 Formulated: 03/80 Revised: 12/02/14 Reviewed: 04/17/18
UTMB RESPIRATORY CARE SERVICES Policy 7.3.50 PROCEDURE - Suction of the Patient with an Artificial Page 5 of 5 Airway Suction of the Patient with an Artificial Airway Effective: 11/07/94 Formulated: 03/80 Revised: 12/02/14 Reviewed: 04/17/18 Suction of the Patient with an Artificial Airway Purpose To outline the procedure for suction of the patient with an artificial airway. Audience All respiratory care practitioners Scope Suction of the patient with an artificial airway is a procedure for the mobilization and removal of secretions. It is used to assist the patient with pulmonary hygiene when the airway severely limits the patient’s own ability to remove lung secretions and to evaluate the patient's cough reflex mechanic in the lung clearing process. Suction to a patient’s airway will be done using sterile techniques according to physician’s orders. A closed catheter suction system will be used on all ventilated patients. Accountability This procedure may be administered by a Licensed Respiratory Care Practitioner with understanding of age specific requirements of patient population. Physician's The physician's order must specify type of therapy and frequency. This Order procedure will automatically be performed as needed unless a physician order specifies a particular frequency. Indications This procedure is indicated for any patient who is intubated or has a tracheostomy, whether or not they are receiving continuous mechanical ventilation. Contra- Suction shall be postponed if the patient's well being is threatened by the indications procedure due to: Acute cardiac arrhythmia, which could be exacerbated by hypoxia or vagal stimulation. -

Efficacy of Active Cycle of Breathing Technique and Postural Drainage in Patients with Bronchiectesis - a Comparative Study
Innovative Journal of Medical and Health Science 2: 6 Nov – Dec (2012) 129 – 132. Contents lists available at www.innovativejournal.in INNOVATIVE JOURNAL OF MEDICAL AND HEALTH SCIENCE Journal homepage: http://www.innovativejournal.in/index.php/ijmhs EFFICACY OF ACTIVE CYCLE OF BREATHING TECHNIQUE AND POSTURAL DRAINAGE IN PATIENTS WITH BRONCHIECTESIS - A COMPARATIVE STUDY Bipin Puneeth1, Mohamed Faisal,C.K2, Renuka Devi.M3, Ajith S4 1Assistant Professor, 3Assistant Professor, JSS college Of Physiotherapy, Mysore 2Professor & Vice Principal, Nitte Institute of Physiotherapy, Nitte University, Mangalore, India-575018 4Assistant Professor, Nitte Institute of Physiotherapy, Nitte University, Mangalore, India-575018 ARTICLE INFO ABSTRACT Corresponding Author: Back Ground and Objective: Bronchiectasis is one of the most common Mohamed Faisal, C. K diseases in the rural and industrial areas of India. The most accepted treatment Professor & Vice Principal, Nitte protocol preferred for Bronchiectasis now days includes oral, aerosolized or Institute of Physiotherapy, intravenous antibiotic therapy according to the severity of the exacerbation and Nitte University, Mangalore, mucus clearance by means of bronchial hygiene assistive devices, surgical India resection, chest physiotherapy like breathing exercises, postural drainage, high- 575018. frequency chest compression, forced expiratory techniques etc. Active cycle of breathing techniques (ACBT) is also the standard airway clearance technique Keywords: ACBT, Postural used in patients with bronchiectasis. So this study is intended to know and Drainage, PEFR, Forced Vital compare the effectiveness of ACBT and Postural drainage techniques as a means Capacity, FEV1, SPO2 of treatments in patients with bronchiectasis. Methodogy: It was a Randomized experimental study with 30 subjects who satisfied the inclusion criteria with a mean age group of 44 were selected for the study. -

Download Download
Prema K et al / Int. J. of Allied Med. Sci. and Clin. Research Vol-5(4) 2017 [823-828] International Journal of Allied Medical Sciences and Clinical Research (IJAMSCR) ISSN:2347-6567 IJAMSCR |Volume 5 | Issue 4 | Oct - Dec - 2017 www.ijamscr.com Research article Medical research Attitude towards pulmonary hygiene and socio-demographic factors affecting it among health workers in two government hospitals East Amhara, Ethiopia Prema Kumara,1 Yemiamrew Getachew,2 Wondwossen Yimam3 1Assistant Professor, Department of Comprehensive Nursing, College of Medicine and Health Sciences, Wollo University Dessie, Ethiopia 2MSc in Clinical and Community Mental Health, Department of Comprehensive Nursing, College of Medicine and Health Science, Wollo University Dessie, Ethiopia 3MSc in Medical Surgical Nursing, School of Nursing and Midwifery, College of Medicine and Health Science, Wollo University Dessie, Ethiopia *Corresponding author: Prema Kumara Email: [email protected] ABSTRACT Introduction Pulmonary hygiene is formerly referred to as pulmonary toilet which is a set of methods used to clear mucus and secretions from the airways and it is depends on consistent clearance of airway secretions. Pulmonary hygiene is a technique designed to help clear mucus and secretions from your lungs. It can be used for people who have chronic obstructive pulmonary disease (COPD), pneumonia, cystic fibrosis, or bronchiectasis and others. Objective To determine level of attitude towards pulmonary hygiene and socio-demographic factors affecting it among health workers in two government hospitals East Amhara, Ethiopia Methodology Institution based cross sectional study design was employed among one hundred twelve health professionals using systematic random sampling technique. The collected data were analyzed using descriptive and inferential statistics. -

Aeromedical Evacuation Springer New York Berlin Heidelberg Hong Kong London Milan Paris Tokyo William W
Aeromedical Evacuation Springer New York Berlin Heidelberg Hong Kong London Milan Paris Tokyo William W. Hurd, MD, MS, FACOG Nicholas J. Thompson Professor and Chair, Department of Obstetrics and Gynecology, Wright State University School of Medicine, Dayton, Ohio; Col, USAFR, MC, FS, Commander, 445th Aeromedical Staging Squadron, Wright-Patterson AFB, Dayton, Ohio John G. Jernigan, MD Brig Gen, USAF, CFS (ret), Formerly Commander, Human Systems Center, Brooks AFB, San Antonio, Texas Editors Aeromedical Evacuation Management of Acute and Stabilized Patients Foreword by Paul K. Carlton, Jr., MD Lt Gen, USAF, MC, CFS USAF Surgeon General With 122 Illustrations 1 3 William W. Hurd, MD, MS John G. Jernigan, MD Nicholas J. Thompson Professor and Chair Brig Gen, USAF, CFS (ret) Department of Obstetrics and Gynecology Formerly Commander Wright State University School of Medicine Human Systems Center Dayton, OH, USA Brooks AFB Col, USAFR, MC, FS San Antonio, TX, USA Commander 445th Aeromedical Staging Squadron Wright-Patterson AFB Dayton, OH, USA Cover illustration: Litter bearers carry a patient up the ramp of a C-9 Nightingale medical transport aircraft. (US Air Force photo by Staff Sgt. Gary R. Coppage). (Figure 7.4 in text) Library of Congress Cataloging-in-Publication Data Aeromedical evacuation : management of acute and stabilized patients / [edited by] William W. Hurd, John G. Jernigan. p. ; cm Includes bibliographical references and index. ISBN 0-387-98604-9 (h/c : alk. paper) 1. Airplane ambulances. 2. Emergency medical services. I. Hurd, William W. II. Jernigan, John J. [DNLM: 1. Air Ambulances. 2. Emergency Medical Services. 3. Rescue Work. WX 215 A252 2002] RA996.5 .A325 2002 616.02¢5—dc21 2002021045 ISBN 0-387-98604-9 Printed on acid-free paper. -
15-Coned-Ccrn-Pulmonary.Pdf
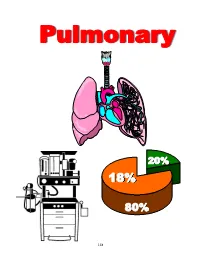
Pulmonary 20% 18% 80% 148 PULMONARY I. Introduction A. AACN-CCRN/CCRN-E Blueprint 18% Acute Lung Injury (e.g. ARDS, RDS) Acute Pulmonary Embolus Acute Respiratory Failure Acute Respiratory Infections (e.g. acute pneumonia, bronchiolitis) Air-Leak Syndromes (e.g. Pneumothorax, PIE, pneumopericardium) Aspiration (e.g. aspiration pneumonia, foreign-body) COPD, Asthma, Chronic Bronchitis, emphysema Pulmonary Hypertension Status Asthmaticus Thoracic Surgery Thoracic Trauma (e.g. fractured ribs, lung contusions, tracheal perforation) B. Review of Anatomy 149 C. Pulmonary Physiology 1. Definitions Ventilation: The process of moving air into and out of the lungs Diffusion: The process of molecules of gas pass from an area of high concentration to one of lower concentration. Alveolar Diffusion and Capillary Diffusion Perfusion: The process of transporting gases to the body (capillary) via the circulatory system. Oxygen Hemoglobin Relationship 150 Oxyhemoglobin Dissociation Curve 100 Shift to the Left pH 90 PaC02 80 Temperature 70 2,3 – DPG % Ph04 60 Saturation Shift to the Right 50 pH 40 PaC02 Temperature 30 2,3 – DPG 20 10 10 20 30 40 50 60 70 80 90 100 Pa02 Dead Space Ventilation: Alveolus is receiving ventilation but not perfusion (pulmonary emboli) Intrapulmonary Shunting: Alveolus is receiving perfusion but not ventilation (atelectasis, pneumonia) II. Assessment of Gas Exchange Variable Normal Arterial Range Pa02 80 - 100mmHg pH 7-35 - 7.45 PaC02 35 - 45mmHg HC03 22 - 26mEq/L Sa02 > 95% Base Excess - 2 - + 2 151 Indications of Oxygenation Status? Indications of Ventilation Status? Indications of Acid-Base State? The Physiology of Acid-Base Balance/Imbalance Respiratory Acid Base Regulation: Ventilation (inspiration & expiration) and Diffusion (movement of gases) are responsible for PaC02 levels. -

The Essential Intensivist Bronchoscopist
The Essential Intensivist Bronchoscopist Bronchoscopy in the Intensive Care Unit Modules I - IV Septimiu Murgu MD, FCCP, Tayfun Caliskan MD, Hugo Oliveira MD, and Henri Colt, MD, FCCP, FAWM With contributions from Drs. John Mullon, Fabien Maldonado, Shaheen Islam, and Patricia Vujacich THE ESSENTIAL INTENSIVIST BRONCHOSCOPIST© Laguna Beach, CA This module was specifically designed for training bronchoscopists working in the intensive care unit. The module and its post-tests, as well as accompanying interactive Powerpoint© presentations are part of a multidimensional curriculum that includes step-by-step hands-on instruction, simulation, instructional videos, patient-based practical approach exercises, and didactic lectures. This educational program has been designed in collaboration with the following members of the Bronchoscopy International team: Dr. John Mullon (Rochester, USA) Dr. Fabien Maldonado (Nashville, USA)) Dr. Shaheen Islam (Columbus, USA) Dr. Patricia Vujacich (Buenos Aires, Argentina) Bronchoscopy International, Laguna Beach, CA 92651 Copyright © 2017, Henri Colt All rights reserved. No part of this publication may be reproduced or transmitted by any means, electronic or mechanical, including photocopy or information storage and retrieval system, without permission from the publisher. Colt Henri G The Essential Intensivist Bronchoscopist© First Edition, 2017 From, The Essential Bronchoscopist Series Title 1: The Essential Intensivist Bronchoscopist; Pulmonary diseases; Thoracic medicine ISBN-13: 9780984834754 1. The Essential