Student's Self-Study Guidelines
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Effects of Hyperaemia on Left Ventricular Longitudinal Strain In
Neth Heart J https://doi.org/10.1007/s12471-017-1071-3 ORIGINAL ARTICLE Effects of hyperaemia on left ventricular longitudinal strain in patients with suspected coronary artery disease A first-pass stress perfusion cardiovascular magnetic resonance imaging study P. G a r g 1 ·R.Aziz1 ·T.AlMusa1 ·D.P.Ripley1 · P.Haaf1 ·J.R.J.Foley1 ·P.P.Swoboda1 ·G.J.Fent1 ·L.E.Dobson1 · J. P.Greenwood1 ·S.Plein1 © The Author(s) 2018. This article is an open access publication. Abstract Aims Myocardial perfusion imaging during hyperaemic stress is commonly used to detect coronary artery disease. The aim of this study was to investigate the relationship between left ventricular global longitudinal strain (GLS), strain rate (GLSR), myocardial early (E’) and late diastolic velocities (A’) with adenosine stress first-pass perfusion cardiovascular magnetic resonance (CMR) imaging. Methods and results 44 patients met the inclusion criteria and underwent CMR imaging. The CMR imaging proto- col included: rest/stress horizontal long-axis (HLA) cine, rest/stress first-pass adenosine perfusion and late gadolinium enhancement imaging. Rest and stress HLA cine CMR images were analysed using feature-tracking software for the assessment of myocardial deformation. The presence of perfusion defects was scored on a binomial scale. In patients with hyperaemia-induced perfusion defects, rest global longitudinal strain GLS (–16.9 ± 3.7 vs. –19.6 ± 3.4; p-value = 0.02), E’ (–86 ± 22 vs. –109 ± 38; p-value = 0.02), GLSR (69 ± 31 vs. 93 ± 38; p-value = 0.01) and stress GLS (–16.5 ± 4 vs. –21 ± 3.1; p < 0.001) were significantly reduced when compared with patients with no perfusion defects. -

Mechanisms of Exertional Angina in Patients with Normal Coronary Arteries
CLINICAL 10.7861/clinmed.20-2-s44 Mechanisms of exertional angina in patients with normal coronary arteries Authors: Haseeb Rahman,A Ozan Demir,A Matthew Ryan,A Hannah McConkey,A Howard Ellis,A Cian Scannell,A Amedeo Chiribiri,A Andrew WebbA and Divaka PereraA Background was defined as hyperaemic endo/epi<1.0.8 Myocardial perfusion reserve (MPR) was calculated as hyperaemic myocardial blood Forty per cent of patients undergoing angiography to investigate flow / resting myocardial blood flow.9 Patients were classified exertional chest pain have normal coronary arteries. While as having MVD if CFR<2.5 and controls if CFR≥2.5, with described for nearly half a century, this condition has remained researchers blinded to the classification.10 a mechanistic enigma.1–2 Diminished coronary blood flow augmentation to a pharmacological vasodilator, or coronary microvascular dysfunction (MVD), portends a greater risk Results 3–4 of major adverse cardiovascular events. However, patients A total of 95 patients were enrolled (57±10 years, 81% report symptoms during physical exercise, and the response women); 52 were classified as having MVD and 43 as controls. to pharmacological ‘stress’ and physical exercise differ in Microvascular resistance (MR) and CBF during peak exercise 5 the healthy heart. Moreover, it is unclear whether MVD is were similar in MVD and controls (4.5±1.6 vs 4.7±1.6 mmHg/ confined to the coronary circulation or a generalised disorder cm/s and 30±10 vs 27±8 cm/s; p=0.68 and p=0.15). However, in myocardial and systemic blood flow during stress. -

Altered Mental Status Predicts Mortality in Cardiogenic Shock – Results From
ACC0010.1177/2048872617702505European Heart Journal: Acute Cardiovascular CareKataja et al. 702505research-article2017 EUROPEAN SOCIETY OF Original scientific paper CARDIOLOGY ® European Heart Journal: Acute Cardiovascular Care 2018, Vol. 7(1) 38 –44 Altered mental status predicts © The European Society of Cardiology 2017 Reprints and permissions: sagepub.co.uk/journalsPermissions.nav mortality in cardiogenic shock – https://doi.org/10.1177/2048872617702505DOI: 10.1177/2048872617702505 results from the CardShock study journals.sagepub.com/home/acc Anu Kataja1, Tuukka Tarvasmäki1, Johan Lassus2, Lars Køber3, Alessandro Sionis4, Jindrich Spinar5, John Parissis6, Valentina Carubelli7, Jose Cardoso8, Marek Banaszewski9, Rossella Marino10, Markku S Nieminen2, Alexandre Mebazaa11 and Veli-Pekka Harjola1 Abstract Background: Altered mental status is among the signs of hypoperfusion in cardiogenic shock, the most severe form of acute heart failure. The aim of this study was to investigate the prevalence of altered mental status, to identify factors associating with it, and to assess the prognostic significance of altered mental status in cardiogenic shock. Methods: Mental status was assessed at presentation of shock in 215 adult cardiogenic shock patients in a multinational, prospective, observational study. Clinical picture, biochemical variables, and short-term mortality were compared between patients presenting with altered and normal mental status. Results: Altered mental status was detected in 147 (68%) patients, whereas 68 (32%) patients had normal mental status. Patients with altered mental status were older (68 vs. 64 years, p=0.04) and more likely to have an acute coronary syndrome than those with normal mental status (85% vs. 74%, p=0.04). Altered mental status was associated with lower systolic blood pressure (76 vs. -
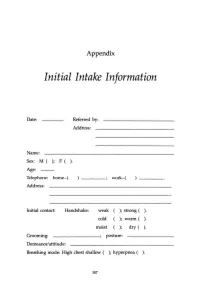
Initial Intake Information
Appendix Initial Intake Information Date: Referred by: Address: Name: Sex: M ( ); F ( ). Age: Telephone: home-( work-( Address: Initial contact: Handshake: weak ); strong ( ). cold ); warm ( ). moist ); dry ( ). Grooming: ________; posture: Demeanor/attitude: Breathing mode: High chest shallow ( ); hyperpnea ( ). 307 308 APPENDIX Sighing: frequent ( ); occasional ( ); absent ( ). Occupation: Contact with: dust ( ); fibers (); paints ( ); solvents ( ); sprays ( ); detergents ( ). Other chemicals or airborne particles: Status: Married ( ); single ( ); divorced ( ); other: children: No. Boys ( ); No. Girls ( ). Physician(s) of record: Last medical examination: _________,199__ Diagnos(e)s: 'Ireatmentts): Medication(s): Do you now have, have you ever had, or has any family member related to you by blood (mother, father, sister, brother, familial grandparents or uncles and aunts) had: ( ) High blood pressure () Heart disease APPENDIX 309 ) Low blood pressure ) Angina ) Diabetes (insulin-dependent) ) Anemia ) Diabetes (non-insulin- ) Allergies dependent) ) Dermatitis ) Colitis ) Muscle spasms ) Gastritis ) Tingling in hands and/or feet ) Ulcer ) Fainting (syncope) ) Shortness of breath ) Dizziness (vertigo) ) Asthma ) Stroke ) Emphysema ) Headache ) Hyperventilation ) TMJlbruxism ) Mitral valve prolapse ) Chronic low backache ) Other heart murmur ) EB virus (mononucl.) ) Heart arrhythmia ) PMS ) Chronic vaginal yeast ) Chronic tiredness ) Cystitis ) Menstrual irregul. ) Raynaud's disease ) Tinnitus ) Chronic pain ) Hyperthyroid ) Eating disorder -

The Diving Response in Man, Rat and Echidna
t('1;'7> THE DIVING RESPONSE IN MAI{, R,AT AÀTD ECHIDNA A TTIESIS Submitted tor the degree of DOCTOR OF I,IEDICINE of The llniversitg of Adelaìde, South AusttaTía bg BRETT ÀùIDREW GOODEN, M.B. rB.S. L97L DECLARATION AIÛD ACKNOIÍLEDGEMENTS I declare that this thesis is of my ovJn composition and that it is a record of original work conducted during the years 19681 1969, I97O a¡¡d I97I in the Department of Human Physiology and Pharmacolog¡¡, University of Adetaide. The work described herein has not been sr¡buritted for any other degree, award or diploma. I wish to record my gratitude to Professor R. F. Itlhelan for his invaluable guidance and encouragement duríng this work. I record my gratitude to Dr M. L. Augee, Mr L. B. Campbell, Dr R. W. Elsner, Mr J. D. Horowitz, Vlt R. G. Lehrnanr Mr J. Plm, Dr S. M. Robinson and Dr P. R. !{ilson with whom I have had the privilege of working during various stages of these investigations. I would also like to thank Dr D. B. Frewin, Dr D. H. LeMessurier and Dr J. A. Vlalsh for their interest in the work, Mrs L. L. Kingston and Èhe Medical School Workshop staff for expert technical assistance, the colleagues and students who volunteered as subjects for experiments, and Lesley, my wife, for her tireless support. I a¡r indebted to the "X" Bequest, National Health and Medical Research Council, National Heart Foundation of Australia and the University of Adelaide for supPort during the years I968-7L. CONTENTS PREFACE HISTORTCAL REVIEW (A) tutimaL SÈudies (B) Human Studies GENERAL I'IETHOÀS Venous Occlusion -

Parts of the Body 1) Head – Caput, Capitus 2) Skull- Cranium Cephalic- Toward the Skull Caudal- Toward the Tail Rostral- Toward the Nose 3) Collum (Pl
BIO 3330 Advanced Human Cadaver Anatomy Instructor: Dr. Jeff Simpson Department of Biology Metropolitan State College of Denver 1 PARTS OF THE BODY 1) HEAD – CAPUT, CAPITUS 2) SKULL- CRANIUM CEPHALIC- TOWARD THE SKULL CAUDAL- TOWARD THE TAIL ROSTRAL- TOWARD THE NOSE 3) COLLUM (PL. COLLI), CERVIX 4) TRUNK- THORAX, CHEST 5) ABDOMEN- AREA BETWEEN THE DIAPHRAGM AND THE HIP BONES 6) PELVIS- AREA BETWEEN OS COXAS EXTREMITIES -UPPER 1) SHOULDER GIRDLE - SCAPULA, CLAVICLE 2) BRACHIUM - ARM 3) ANTEBRACHIUM -FOREARM 4) CUBITAL FOSSA 6) METACARPALS 7) PHALANGES 2 Lower Extremities Pelvis Os Coxae (2) Inominant Bones Sacrum Coccyx Terms of Position and Direction Anatomical Position Body Erect, head, eyes and toes facing forward. Limbs at side, palms facing forward Anterior-ventral Posterior-dorsal Superficial Deep Internal/external Vertical & horizontal- refer to the body in the standing position Lateral/ medial Superior/inferior Ipsilateral Contralateral Planes of the Body Median-cuts the body into left and right halves Sagittal- parallel to median Frontal (Coronal)- divides the body into front and back halves 3 Horizontal(transverse)- cuts the body into upper and lower portions Positions of the Body Proximal Distal Limbs Radial Ulnar Tibial Fibular Foot Dorsum Plantar Hallicus HAND Dorsum- back of hand Palmar (volar)- palm side Pollicus Index finger Middle finger Ring finger Pinky finger TERMS OF MOVEMENT 1) FLEXION: DECREASE ANGLE BETWEEN TWO BONES OF A JOINT 2) EXTENSION: INCREASE ANGLE BETWEEN TWO BONES OF A JOINT 3) ADDUCTION: TOWARDS MIDLINE -

Kuban State Medical University" of the Ministry of Healthcare of the Russian Federation
Federal State Budgetary Educational Institution of Higher Education «Kuban State Medical University" of the Ministry of Healthcare of the Russian Federation. ФЕДЕРАЛЬНОЕ ГОСУДАРСТВЕННОЕ БЮДЖЕТНОЕ ОБРАЗОВАТЕЛЬНОЕ УЧРЕЖДЕНИЕ ВЫСШЕГО ОБРАЗОВАНИЯ «КУБАНСКИЙ ГОСУДАРСТВЕННЫЙ МЕДИЦИНСКИЙ УНИВЕРСИТЕТ» МИНИСТЕРСТВА ЗДРАВООХРАНЕНИЯ РОССИЙСКОЙ ФЕДЕРАЦИИ (ФГБОУ ВО КубГМУ Минздрава России) Кафедра пропедевтики внутренних болезней Department of Propaedeutics of Internal Diseases BASIC CLINICAL SYNDROMES Guidelines for students of foreign (English) students of the 3rd year of medical university Krasnodar 2020 2 УДК 616-07:616-072 ББК 53.4 Compiled by the staff of the department of propaedeutics of internal diseases Federal State Budgetary Educational Institution of Higher Education «Kuban State Medical University" of the Ministry of Healthcare of the Russian Federation: assistant, candidate of medical sciences M.I. Bocharnikova; docent, c.m.s. I.V. Kryuchkova; assistent E.A. Kuznetsova; assistent, c.m.s. A.T. Nepso; assistent YU.A. Solodova; assistent D.I. Panchenko; docent, c.m.s. O.A. Shevchenko. Edited by the head of the department of propaedeutics of internal diseases FSBEI HE KubSMU of the Ministry of Healthcare of the Russian Federation docent A.Yu. Ionov. Guidelines "The main clinical syndromes." - Krasnodar, FSBEI HE KubSMU of the Ministry of Healthcare of the Russian Federation, 2019. – 120 p. Reviewers: Head of the Department of Faculty Therapy, FSBEI HE KubSMU of the Ministry of Health of Russia Professor L.N. Eliseeva Head of the Department -

Supporting Men's Health in the Pharmacy
SUPPORTING MEN’S HEALTH IN THE PHARMACY Important information about VIAGRA CONNECT® Sildenafil Essential information Sildenafil FULL ESSENTIAL INFORMATION Name of product: VIAGRA CONNECT 50 mg film-coated tabletsActive ingredient(s): sildenafil Product licence number: PL 50622/0063 Name and address of the product licence holder: Upjohn UK Limited, Ramsgate Road, Sandwich, Kent, CT13 9NJ, UK Supply classification: P Indications: For erectile dysfunction in adult men. Side Effects: The safety profile of VIAGRA is based on > 9,000 patients in > 70 double-blind placebo controlled clinical studies. The most commonly reported adverse reactions in clinical studies among sildenafil treated patients were headache, flushing, dyspepsia, nasal congestion, dizziness, nausea, hot flush, visual disturbance, cyanopsia and vision blurred. Adverse reactions from post marketing surveillance has been gathered covering an estimated period >10 years. Because not all adverse reactions are reported to the Marketing Authorisation Holder and included in the safety database, the frequencies of these reactions cannot be reliably determined. Very Common (≥ 1/10): Headache. Common (≥ 1/100 and <1/10): Dizziness, Visual colour distortions (Chloropsia, Chromatopsia, Cyanopsia, Erythropsia and Xanthopsia), Visual disturbance, Vision blurred, Flushing, Hot flush, Nasal congestion, Nausea, Dyspepsia. Uncommon (≥ 1/1,000 and <1/100): Rhinitis, Hypersensitivity; Somnolence; Hypoaesthesia, Lacrimation disorders (Dry eye, Lacrimal disorder and Lacrimation increased), Eye pain, -

EMS Quick Study Guide NOTICE: You DO NOT Have the Right to Reprint Or Resell This Publication
Presents The EMS Quick Study Guide NOTICE: You DO NOT Have the Right to Reprint or Resell this Publication. You Also MAY NOT Give Away, Sell or Share the Content Herein. If you purchased this book/ebook from anywhere other than http://www.ems-safety.com , you have a pirated copy. Please help stop Internet crime by reporting this to: [email protected] © Copyright The EMS Professional ALL RIGHTS RESERVED. No part of this publication may be reproduced or transmitted in any form whatsoever, electronic, or mechanical, including photocopying, recording, or by any informational storage or retrieval system without the expressed written, dated and signed permission from the author. DISCLAIMER AND/OR LEGAL NOTICES: The information presented herein represents the views of the author as of the date of publication. Because of the rate with which conditions change, the author reserves the right to alter and update this information based on the new conditions. The publication is for informational purposes only. While every attempt has been made to verify the information provided in this publication, neither the author nor its affiliates/partners assume any responsibility for errors, inaccuracies or omissions. Any slights of people or organizations are unintentional. If advice concerning medical, legal or related matters is needed, the services of a fully qualified professional should be sought. You should be aware of any laws/practices or local policies which govern emergency care or other pre hospital care practices in your country and state. -

The Psychology of Erection Problems
Introduction EPs are complex and can affect men at any age. Sildenafil They often have both psychological and physical components. Careful questioning will help to ensure that the advice is tailored to each patient. Giving men the opportunity to discuss any medical THE PSYCHOLOGY concerns and issues may highlight opportunities for signposting to other services to improve their overall health. OF ERECTION Men are often reticent to speak to healthcare professionals about their health. Every consultation for EPs gives an opportunity to discuss lifestyle PROBLEMS changes, medication use, health monitoring, mental wellbeing and general health concerns, and support male patients to improve their overall wellbeing. This training is for pharmacy professionals to support them to advise men affected by erection problems (EPs) and recognise opportunities for Remember that you can record any learning and engaging with men about their general health. how you use this information in your consultations as part of your revalidation. Objectives: l Understand the potential psychological causes of EPs l Appreciate how both younger and older men may be affected by EPs l Understand the wider physical and mental health aspects of EPs REFLECTION: Are you confident to signpost men to other services when having conversations about EPs? Do you know what other services are available in your area to support men’s health? Pharmacist Tom Advising on EPs Depression Having difficulty getting or Depression can affect how sustaining an erection hard men feel about themselves enough for sex (called erectile and others, and sufferers are less likely to seek help.1 dysfunction, or erection EPs may either contribute problems) is common and to, or result from, can be treated in many cases. -

Angina: Contemporary Diagnosis and Management Thomas Joseph Ford ,1,2,3 Colin Berry 1
Education in Heart CHRONIC ISCHAEMIC HEART DISEASE Heart: first published as 10.1136/heartjnl-2018-314661 on 12 February 2020. Downloaded from Angina: contemporary diagnosis and management Thomas Joseph Ford ,1,2,3 Colin Berry 1 1BHF Cardiovascular Research INTRODUCTION Learning objectives Centre, University of Glasgow Ischaemic heart disease (IHD) remains the leading College of Medical Veterinary global cause of death and lost life years in adults, and Life Sciences, Glasgow, UK ► Around one half of angina patients have no 2 notably in younger (<55 years) women.1 Angina Department of Cardiology, obstructive coronary disease; many of these Gosford Hospital, Gosford, New pectoris (derived from the Latin verb ‘angere’ to patients have microvascular and/or vasospastic South Wales, Australia strangle) is chest discomfort of cardiac origin. It is a 3 angina. Faculty of Health and Medicine, common clinical manifestation of IHD with an esti- The University of Newcastle, ► Tests of coronary artery function empower mated prevalence of 3%–4% in UK adults. There Newcastle, NSW, Australia clinicians to make a correct diagnosis (rule- in/ are over 250 000 invasive coronary angiograms rule- out), complementing coronary angiography. Correspondence to performed each year with over 20 000 new cases of ► Physician and patient education, lifestyle, Dr Thomas Joseph Ford, BHF angina. The healthcare resource utilisation is appre- medications and revascularisation are key Cardiovascular Research Centre, ciable with over 110 000 inpatient episodes each aspects of management. University of Glasgow College year leading to substantial associated morbidity.2 In of Medical Veterinary and Life Sciences, Glasgow G128QQ, UK; 1809, Allen Burns (Lecturer in Anatomy, Univer- tom. -
Monographie Des Dégenérations Skirrheuses De L'estomac, Fondée
PART II. COMPREHENSIVE ANALYTICAL REVIEW OF MEDICAL LITERATURE. u Tros, tyriusve, nobis nullo discrimine agetur." Monographic des Degenerations Skirrheuses de VEstOmac, Jondee sur un grand nombre d'Observations recueillies tant a la Clinique de VEcole de Medecine de Paris, qvHa / Hopilal Cochin. Par Frederic Chardel, D. M. Medecin de l'Hopital Cochin, &c. 8vo. pp. 216. A Paris. " This excellent Monograph on scirrhous Affections of the Stomach" is the production of Dr. Chardel, a disciple of the celebrated Corvisart, to whom the volume is inscribed. Chardel, on scirrhous Affections of the Stomach. 1Q? a Although publication of no very recent date, we feel persuaded that, in announcing it, we shall introduce to the acquaintance of the general practitioner a work, the contents and even title of which are little known within his sphere of reading and conversation ; and we are in- cited to the labour of its analysis by the hope of confer- ring no mean benefit upon those to whom the original is inaccessible, but who prefer the researches of the dead- house to the abstract and commonly futile speculations of the closet, and regard a correct knowledge of the anato- mical character and varieties of a disease quite as essen- tial to sound nosological arrangement and successful prac- tice, as vigilant observation of the external phaenomena which it presents. To such, then, our analytical sketch is dedicated: and may the ardour displayed by the en- lightened foreigner in the prosecution of his pathological inquiries, exert a benignant influence upon those for whom we write, and arouse them to emulate his example.