Glossary of Pharmaceutical Terms
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
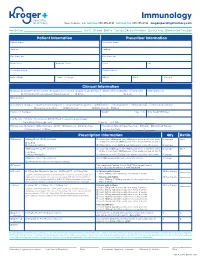
Immunology New Orleans, LA Toll Free 888.355.4191 Toll Free Fax 888.355.4192 Krogerspecialtypharmacy.Com
Immunology New Orleans, LA toll free 888.355.4191 toll free fax 888.355.4192 krogerspecialtypharmacy.com Need By Date: _________________________________________________ Ship To: Patient Office Fax Copy: Rx Card Front/Back Clinical Notes Medical Card Front/Back Patient Information Prescriber Information Patient Name Prescriber Name Address Address City State Zip City State Zip Main Phone Alternate Phone Phone Fax Social Security # Contact Person Date of Birth Male Female DEA # NPI # License # Clinical Information Diagnosis: J45.40 Moderate Asthma J45.50 Severe Asthma L20.9 Atopic Dermatitis L50.1 Chronic Idiopathic Urticaria (CIU) Eosinophil Levels J33 Chronic Rhinosinusitis with Nasal Polyposis Other: ________________________________ Dx Code: ___________ Drug Allergies Concomitant Therapies: Short-acting Beta Agonist Long-acting Beta Agonist Antihistamines Decongestants Immunotherapy Inhaled Corticosteroid Leukotriene Modifiers Oral Steroids Nasal Steroids Other: _____________________________________________________________ Please List Therapies Weight kg lbs Date Weight Obtained Lab Results: History of positive skin OR RAST test to a perennial aeroallergen Pretreatment Serum lgE Level: ______________________________________ IU per mL Test Date: _________ / ________ / ________ MD Specialty: Allergist Dermatologist ENT Pediatrician Primary Care Prescription Type: Naïve/New Start Restart Continued Therapy Pulmonologist Other: _________________________________________ Last Injection Date: _________ / ________ -
The Origin of Bimaristans (Hospitals) in Islamic Medical History
The Origin of Bimaristans (Hospitals) in Islamic Medical History IMPORTANT NOTICE: Author: Dr. Sharif Kaf Al-Ghazal Chief Editor: Prof. Mohamed El-Gomati All rights, including copyright, in the content of this document are owned or controlled for these purposes by FSTC Limited. In Deputy Editor: Prof. Mohammed Abattouy accessing these web pages, you agree that you may only download the content for your own personal non-commercial Associate Editor: Dr. Salim Ayduz use. You are not permitted to copy, broadcast, download, store (in any medium), transmit, show or play in public, adapt or Release Date: April 2007 change in any way the content of this document for any other purpose whatsoever without the prior written permission of FSTC Publication ID: 682 Limited. Material may not be copied, reproduced, republished, Copyright: © FSTC Limited, 2007 downloaded, posted, broadcast or transmitted in any way except for your own personal non-commercial home use. Any other use requires the prior written permission of FSTC Limited. You agree not to adapt, alter or create a derivative work from any of the material contained in this document or use it for any other purpose other than for your personal non-commercial use. FSTC Limited has taken all reasonable care to ensure that pages published in this document and on the MuslimHeritage.com Web Site were accurate at the time of publication or last modification. Web sites are by nature experimental or constantly changing. Hence information published may be for test purposes only, may be out of date, or may be the personal opinion of the author. -

STEM Disciplines
STEM Disciplines In order to be applicable to the many types of institutions that participate in the HERI Faculty Survey, this list is intentionally broad and comprehensive in its definition of STEM disciplines. It includes disciplines in the life sciences, physical sciences, engineering, mathematics, computer science, and the health sciences. Agriculture/Natural Resources Health Professions 0101 Agriculture and related sciences 1501 Alternative/complementary medicine/sys 0102 Natural resources and conservation 1503 Clinical/medical lab science/allied 0103 Agriculture/natural resources/related, other 1504 Dental support services/allied 1505 Dentistry Biological and Biomedical Sciences 1506 Health & medical administrative services 0501 Biochem/biophysics/molecular biology 1507 Allied health and medical assisting services 0502 Botany/plant biology 1508 Allied health diagnostic, intervention, 0503 Genetics treatment professions 0504 Microbiological sciences & immunology 1509 Medicine, including psychiatry 0505 Physiology, pathology & related sciences 1511 Nursing 0506 Zoology/animal biology 1512 Optometry 0507 Biological & biomedical sciences, other 1513 Osteopathic medicine/osteopathy 1514 Pharmacy/pharmaceutical sciences/admin Computer/Info Sciences/Support Tech 1515 Podiatric medicine/podiatry 0801 Computer/info tech administration/mgmt 1516 Public health 0802 Computer programming 1518 Veterinary medicine 0803 Computer science 1519 Health/related clinical services, other 0804 Computer software and media applications 0805 Computer systems -

The Contemporary Physician Leader
White Paper The Contemporary Physician Leader By Miles Snowden, MD Optum www.optum.com/aco 800.765.6619 Page 1 The Contemporary Physician Leader White Paper The “Triple Aim”—a term coined by the Institute of Healthcare Improvement to embody the goals of better care, controlled costs and improved health—has become a rallying cry in the health care industry.1 As the health care market in the United States focuses on changing incentives to accomplish the Triple Aim, a new generation of better improved leaders is needed who can clinically and financially transform provider care health organizations. Chief medical officers (CMOs) and other physician leaders Triple in hospitals, group practices and integrated delivery systems have unique Aim qualifications that can allow them to take ownership of these important changes. However, their success in this new era will require that they controlled evolve away from the roles they have traditionally played. costs This paper will share the perspectives of five physician leaders who represent the contemporary physician leader. In doing so, it will discuss the skill set, experience and qualities physician executives need to lead their organizations’ conversion from volume to value. Physician executive roles continue to evolve The role of the physician executive has evolved over the years. The traditional physician leader in a hospital setting is a medical director. Medical directors were sometimes employed by facilities but often were independent, affiliated doctors. These providers served as liaisons between hospitals and the credentialed medical staff. They worked closely with hospital administrators but rarely had a seat at the executive table. -

Pharmacy/Medical Drug Prior Authorization Form
High Cost Medical Drugs List High Cost Medical Drugs administered by Health Alliance™ providers within physician offices, infusion centers or hospital outpatient settings must be acquired from preferred specialty vendors. Health Alliance will not reimburse any drug listed as a “High Cost Medical Drug,” whether obtained from the provider’s own stock or via “buy-and-bill.” This drug list does not apply to members with Medicare coverage. Information on how to acquire these medications is located at the end of this document. Recent Updates Preferred Contact Drug Therapy Drug Name Code PA Effective Change Vendor Number Oncology – Injectable DARZALEX FASPRO J9144 YES 10/1/2021 CVS/Caremark® 800-237-2767 Added High Cost Medical Drug List Preferred Contact Drug Therapy Drug Name Code PA Effective Vendor Number Acromegaly SANDOSTATIN J2353 YES 7/1/2020 CVS/Caremark® 800-237-2767 Acromegaly SOMATULINE J1930 YES 7/1/2020 CVS/Caremark® 800-237-2767 Additional Products JETREA J7316 YES 7/1/2020 LDD Additional Products PROLASTIN J0256 YES 7/1/2020 LDD Additional Products QUTENZA J7336 NO 7/1/2020 LDD Additional Products REVCOVI J3590 YES 7/1/2020 LDD Additional Products RADICAVA J1301 YES 7/1/2020 CVS/Caremark® 800-237-2767 Additional Products SIGNIFOR J2502 YES 7/1/2020 Accredo® 866-759-1557 Additional Products SPRAVATO J3490 YES 7/1/2020 CVS/Caremark® 800-237-2767 Additional Products STRENSIQ J3590 YES 7/1/2020 LDD Additional Products THIOTEPA J9340 YES 7/1/2020 CVS/Caremark® 800-237-2767 Allergic Asthma CINQAIR J2786 YES 7/1/2020 CVS/Caremark® 800-237-2767 -

Chief Physician and Surgeon
OPEN SPOT CONTINUOUS EXAMINATION FOR DEPARTMENT OF STATE HOSPITALS- ATASCADERO, COALINGA, METROPOLITAN, NAPA, AND PATTON CHIEF PHYSICIAN AND SURGEON www.dsh.ca.gov The State of California is an equal opportunity employer to all, regardless of age, ancestry, color, disability (mental and physical), exercising the right to family care and medical leave, gender, gender expression, gender identity, genetic information, marital status, medical condition, military or veteran status, national origin, political affiliation, race, religious creed, sex (includes pregnancy, childbirth, breastfeeding and related medical conditions), and sexual orientation. It is the objective of the State of California to achieve a drug-free state workplace. Any applicant for State employment will be expected to behave in accordance with this objective because the use of illegal drugs is inconsistent with the law of the State, the rules governing civil service, and the special trust placed in public servants. EXAMINATION TYPE This is an open examination for the Department of State Hospitals. Examination and/or Employment Applications will not be accepted on a promotional basis. Career credits do not apply. HOW TO APPLY Please submit an Examination and/or Employment Application (STD. 678) form to the address indicated below. DO NOT SUBMIT EXAMINATION AND/OR EMPLOYMENT APPLICATION FORMS TO THE CALIFORNIA DEPARTMENT OF HUMAN RESOURCES. NOTE: All Examination and/or Employment Application forms must include: “to” and “from” dates (month/day/year); time base; and civil service class titles. Examination and/or Employment Application forms received without this information will be rejected. Resumes will not be accepted in lieu of a completed Examination and/or Employment Application (STD. -

Current Status of Immunology Education in US Schools And
American Journal of Pharmaceutical Education 2019; 83 (7) Article 6994. RESEARCH Current Status of Immunology Education in US Schools and Colleges of Pharmacy Yuan Zhao, PhD,a Dana Ho, PharmD,a Benjamin Oldham, PharmD,a Bonnie Dong, PharmD,a Daniel Malcom, PharmDa,b a Sullivan University College of Pharmacy, Louisville, Kentucky b Associate Editor, American Journal of Pharmaceutical Education, Arlington, Virginia Submitted February 2, 2018; accepted June 17, 2018; published September 2019. Objective. To determine the extent of immunology education in US Doctor of Pharmacy (PharmD) programs. Methods. Curricular information on immunology education was collected from the web pages of US PharmD programs (N5142). The data were sorted, comparisons were made, and trends were identified. Results. Of 142 PharmD programs studied, 100% posted curriculum information on their websites. Among them, 73 programs (51.4%) had a dedicated immunology course in their curriculum, either as an independent course or a course combined with another subject. Most immunology education was offered in the first professional year (72.5%). Of the programs that offered immunology as an in- dependent course, the number of semester hours dedicated to the course varied from 1.5 to 3.5 (median53, mode53, mean52.7). More three-year programs offered immunology as a core compo- nent in the didactic curriculum than did four-year programs (64.7% vs 49.6%). Similarly, more private programs offered immunology than did public programs (64% vs 37.3%). Conclusion. Immunology education in US schools and colleges of pharmacy lacks consensus. Not all PharmD programs indicated they offered specific, focused immunology education in their curricula. -

Telepharmacy Rules and Statutes: a 50-State Survey
American Journal of Medical Research 5(2), 2018 pp. 7–23, ISSN 2334-4814, eISSN 2376-4481 doi:10.22381/AJMR5220181 TELEPHARMACY RULES AND STATUTES: A 50-STATE SURVEY GEORGE TZANETAKOS Department of Health Management and Policy, College of Public Health, The University of Iowa FRED ULLRICH Department of Health Management and Policy, College of Public Health, The University of Iowa KEITH MUELLER [email protected] Department of Health Management and Policy, College of Public Health, The University of Iowa (corresponding author) ABSTRACT. There has been a significant decline in the number of independently owned rural pharmacies serving non-metropolitan areas, thereby limiting access to pharmaceutical services for rural residents, particularly for those most vulnerable and in need of these services. The use of telepharmacy is one potential solution to this problem. Telepharmacies deliver pharmaceutical care to outpatients at a distance via telecommunication and other advanced technologies. This study identifies rules and laws enacted by states authorizing the use of community telepharmacy initiatives within their respective jurisdictions. As of August 2016, the use of telepharmacy was authorized, in varying capacities, in 23 states (46%). Pilot program development that could apply to telepharmacy initiatives was authorized by six states (12%). Waivers to administrative or legislative pharmacy practice requirements that could allow for telepharmacy initiatives were permitted in five states (10%). Nearly one-third of the states (16, or 32%) did not authorize the use of telepharmacy, nor did they authorize the pursuit of telepharmacy initiatives via pilot programs or waivers. Keywords: telepharmacy; rule; statute; rural; community; outpatient How to cite: Tzanetakos, George, Fred Ullrich, and Keith Mueller (2018). -

Health Science: Biomedicine Public Service Endorsement
INNOVATE • COLLABORATE • EDUCATE • INNOVATE • COLLABORATE • EDUCATE Health Science: Biomedicine Public Service Endorsement Career Pathways • Biochemist • Biomedical Engineer • Biophysicist • Physician, Surgeon Certifications / Certificate Options • CPR • OSHA Program Highlights Biomedical engineering represents new areas of medical research and • Pathogen Analysis product development; biomedical engineers’ work helps pave the way • Human Anatomy & Physiology for new ways to help treat injuries and diseases. As medicine is a field • DNA / Genomics with vast numbers of specific disciplines, there are many different sub- • Laboratory Procedures fields in which biomedical engineers work. Some work to improve and • Dissection develop new machinery, such as robotic surgery equipment; others • Grow and Culture Bacteria endeavor to create better, more reliable replacement limbs (or parts • Real World Research which help existing limbs function better, such as joint replacements). • Learn to Treat Patients New and more comfortable patient beds, monitoring equipment, and electronics are also products that often begin as concepts from the CTSO(s) biomedical engineer’s or involve some level of input from them. • HOSA - Future Health Professionals KISD Biomedical Program: Program Fees / Requirements Biomedicine classes in KISD aim to prepare students to enter the • HOSA membership (Optional) health care field by giving them a foundation in real world problems, medical treatments, and a better understanding of the human body. Program Location Students will investigate causes and treatments of diseases that R Course(s) available at CHS affect the entire world as well as ones found in our own community. R Course(s) available at FRHS Students learn advanced techniques used in hospitals and research R Course(s) available at KHS labs and will become familiar with protocols used by doctors and R Course(s) available at TCHS researchers today. -

Specialty Pharmacy Drug List
Specialty Pharmacy Drug List Our Specialty Pharmacy provides patients with comprehensive support services and coordinated delivery related to high-cost oral, inhaled or injectable specialty medications, used to treat complex conditions. We are your single source for high-touch patient care management to control side effects, patient support and education to ensure compliance or continued treatment, and specialized handling and distribution of medications directly to the patient or care provider. Specialty medications may be covered under either the medical or pharmacy benefit. Please consult your insurance documentation to determine which benefit covers these medications. We offer a broad specialty medication list containing nearly 500 drugs, covering 42 therapeutic categories and specialty disease states. This list is updated with new information each quarter. Characteristics of Specialty Medications “Specialty” medications are defined as high-cost oral or injectable medications used to treat complex chronic conditions. These are highly complex medications, typically biology-based, that structurally mimic compounds found within the body. High-touch patient care management is usually required to control side effects and ensure compliance. Specialized handling and distribution are also necessary to ensure appropriate medication administration. Medications must have at least one of the following characteristics in order to be classified as a specialty medication by Magellan Rx Management. High Cost High Complexity High Touch High-cost medications -

Credentials Policy
CREDENTIALS POLICY Deer Valley Medical Center John C. Lincoln Medical Center Scottsdale Osborn Medical Center Scottsdale Shea Medical Center Scottsdale Thompson Peak Medical Center Proposed April 11, 2018 Horty, Springer & Mattern, P.C. 259050.19 CREDENTIALS POLICY TABLE OF CONTENTS PAGE 1. GENERAL ..........................................................................................................................1 1.A. TIME LIMITS .........................................................................................................1 1.B. DELEGATION OF FUNCTIONS ..........................................................................1 1.C. CONFIDENTIALITY AND PEER REVIEW PROTECTION ...............................1 1.C.1. Confidentiality .............................................................................................1 1.C.2. Peer Review Protection ................................................................................2 1.D. INDEMNIFICATION..............................................................................................2 1.E. DEFINITIONS .........................................................................................................2 2. QUALIFICATIONS, CONDITIONS, AND RESPONSIBILITIES .............................7 2.A. QUALIFICATIONS ................................................................................................7 2.A.1. Threshold Eligibility Criteria .......................................................................7 2.A.2. Extension of Time Frame to Satisfy Board -

Biomedicine, Pharmacy and Health Care SECTORAL SERVICES of MATHEMATICAL RESEARCH Spanish Network for Mathematics & Industry for COMPANIES C/ Lope Gómez De Marzoa, S/N
Biomedicine, pharmacy and health care SECTORAL SERVICES OF MATHEMATICAL RESEARCH Spanish Network for Mathematics & Industry FOR COMPANIES C/ Lope Gómez de Marzoa, s/n. Campus Vida | CP 15782 Santiago de Compostela (A Coruña) Tel. 881 813 373 | 881 813 223 [email protected] | www.math-in.net math- in Biomedicine, Pharmacy and Health Care Specialized services Mathematics is an effective tool with proven ability to Biomedicine, Pharmacy and Health industries bring meet the demands and needs of businesses. In Spain, together the supply of 29 research groups of the i-MATH Biomedicine and Pharmacy many innovative solutions emerged from the experience project, of which up to 20 have proven experience from gained by research groups in this field through successful having effectively carried out consulting activities, training • Analysis and design of experiments. • Studies of efficacy and safety of treatments. partnerships with industry over the years. All those courses and other collaborations. The details of these • Characterization/grading of pharmaceutical and medical waste. encouraging cases support its potential in offering an groups can be found in the 'Sectors' section of the • Modelling of mortality tables. increasingly sophisticated and complete service to the platform www.math-in.net. • Numerical simulation of fractures, dental implants and orthodontic brackets. industry. • Biomechanics. Bones formation. The mathematical technology services provided in this • Bioinformatics. • Mathematical Biology. Synthetic Biology. The Spanish Network for Mathematics & Industry sector can be broken down into two blocks (on the one • Computational design of proteins. (math-in) is a stable platform that continues the work hand, Biomedicine and Pharmacy and, on the other • Metabolism.