An Act to Require Health Care Coverage for the Emergency Psychiatric Services
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Protect Your Collective Bargaining Rights!
PROTECT YOUR COLLECTIVE BARGAINING RIGHTS! On April 26th, a majority of the members of the Massachusetts of House Representatives voted to dramatically restrict the rights of municipal employees to collectively bargain over the issue of health insurance. It is critically important that you let your Representative know how you feel about their vote. These Representatives voted IN FAVOR of your collective bargaining rights: Democrats: Geraldo Alicea Denise Andrews Bruce Ayers Michael Brady Paul Brodeur Thomas Calter Christine Canavan James Cantwell Tackey Chan Nicholas Collins Edward Coppinger Geraldine Creedon Mark Cusack Marcos Devers James Dwyer Lori Ehrlich Christopher Fallon Robert Fennell John Fresolo Denise Garlick Coleen Garry John Mahoney Paul Mark James Miceli Kevin Murphy Rhonda Nyman James O’Day Thomas Petrolati Denise Provost Kathi-Anne Reinstein Carl Sciortino Joyce Spiliotis Thomas Stanley David Sullivan Walter Timilty Timothy Toomey Cleon Turner Marty Walsh Steven Walsh Alice Wolf Republicans: Bradford Hill Daniel Winslow If your state representative stood up for you, it is important that you call them and thank them for their support. You can say something like this: My name is ____________________ and I live in __________________. I work for the city/town of ___________ as a _____________. I am calling because Rep. ____________ voted in favor of maintaining collective bargaining rights for municipal workers like me. I wanted to thank Rep. ______________ for standing up for my union rights. These Representatives voted AGAINST -

FRCOG 2018-2019 Municipal Directory
Franklin Regional Council of Governments 2018 - 2019 Service • Advocacy We’d like to Acknowledge... This directory is published with the assistance of many people working in our member communities. We greatly ap- preciate the municipal employees who took time away from their busy schedules to provide us with the contact information listed in this book. Without this collaborative effort, publishing the booklet would not be possible. 2018 - 2019 Municipal Directory Table of Contents Franklin Regional Council of Governments New Salem 40 Council & Committee Membership 1 Northfield 42 Franklin Regional Planning Board (FRPB) 3 Orange 44 FRCOG Core Values 4 Rowe 46 Departments & Staff Directory 5 Shelburne 48 Shutesbury 50 Annual Town Meetings & Elections 7 Sunderland 52 Warwick 54 Municipal Offices and Officials Directory Wendell 56 Whately 58 Ashfield 8 Bernardston 10 Buckland 12 Franklin County Town Facts and Figures Charlemont 14 Population and Voter Census Data 60 Colrain 16 Equalized Valuations and Tax Rates 61 Conway 18 Town Area & Road Mileage 62 Deerfield 20 Erving 22 Regional Services Gill 24 Regional Programs 63 Greenfield 26 Franklin County Public Schools Systems 64 Hawley 28 Senior Centers & Services 65 Heath 30 Leverett 32 Legislative Delegations Leyden 34 State Legislative Delegation 67 Monroe 36 Federal Legislative Delegation 68 Montague 38 Contents FRCOG Council Membership The Franklin Regional Council of Governments is comprised of three bodies: the Council, acting as the representative body; the Executive Committee, acting as the executive body; and the Franklin Regional Planning Board, acting as an advisory body on regional planning issues and policies. The FRCOG Council meets at least quarterly, typically on the third Thursday of the months of July, October, January, and April. -

Legislative Profiles Spring 2019 |
Legislative Profiles Spring 2019 | Announcement Inside This Issue This portfolio contains the profiles of all legislators that belong to PG. 2: Forward key committees within the Commonwealth of Massachusetts. PG. 4: House Bill – H.2366 Each key committee will play a role in the review and approval of the retirement bills that have been filed. PG. 8: Senate Bill – SD.1962 PG. 11: Joint Committee on Public Service – Profiles PG. 29: House Ways & Means – Profiles This portfolio is for the members of MCSA to use to determine PG. 63: House Committee on Third Reading – Profiles which members reside within their regions so contact can be made with each legislator for support of both retirement bills. PG. 67: Senate Ways & Means – Profiles PG. 86: Senate Committee on Third Reading – Profiles PG. 92: Talking Point Tips PG. 93: Legislative Members by MCSA Regions FORWARD Many of us do not have experience with advocating for legislation or meeting with our legislative representatives. This booklet was created with each you in mind to assist in determining which members reside within your region or represent your town and city. We request you contact your respective legislators for support of both retirement bills. If you are familiar with the legislative process and your representatives this may seem rudimentary. The Massachusetts Legislature is comprised of 200 members elected by the people of the Commonwealth. The Senate is comprised of 40 members, with each representing a district of approximately 159,000 people. The House of Representatives is comprised of 160 members, with each legislator representing districts consisting of approximately 40,000 people. -
View the Vote Chart
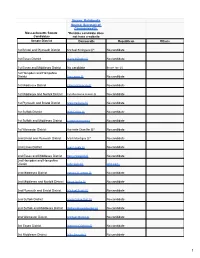
UPDATE THE BOTTLE BILL YES! I pledge to help. The Bottle Bill (5¢ deposit on some beverage containers) is the single most successful recycling tool in the country. But the Updated Bottle Bill—adding water, juice and sports drinks to the deposits—is being blocked by powerful business interests on Beacon Hill. The Updated Bottle Bill (H890/S1650) will reduce litter, increase recycling, and save cities and towns money in trash disposal and litter cleanup. In fact, 208 cities and towns, 375 small businesses, and 90 state and local organizations have endorsed our campaign and joined the effort to pass this bill. Despite this overwhelming support, the Updated Bottle Bill has been “bottled up” in the Legislature for more than a decade. It has never been brought to the floor for a vote, and we need your help now. No more delays! Here’s how you can help: STEP 1: To find out the name of your representative and senator, go to www.WhereDoIVoteMA.com STEP 2: Find out where your legislators stand on the Updated Bottle Bill. See the back of this flyer for a complete guide. STEP 3: Call your state senator and representative today. The State House main number is (617) 722- 2000. Ask for your senator (and then call back and ask for your representative). Tell them: “I am a voter in (name your town) and I support the Updated Bottle Bill. There should be no more delays, this bill needs to come up for a vote now.” (If your legislator supports the Updated Bottle Bill, make sure to thank them, if they are undecided or not supporting the bill, ask them to consider supporting the bill.) STEP 4: After you call, please email [email protected] to let us know your legislator’s response. -

Women's Bar Association's 2021-2022 Legislative Agenda
Women’s Bar Association’s 2021-2022 Legislative Agenda Priority Items : An Act to Lift Kids Out of Deep Poverty (Sen. DiDomenico – S.96)/An Act to Reduce Deep Poverty Among Kids (Rep Decker – H.199). An Act Relative to Inmate Telephone Calls (Rep. Tyler – H.1900) / An Act relative to inmate telephone Calls (Sen. Creem – S.1559). Civil Legal Aid Funding: FY2022 Massachusetts Legal Assistance Corporation State Budget Line Item: 0321-1600. An Act Relative to Employment Protections for Victims of Abusive Behavior (Reps. Livingstone & Elugardo – H.2018 / Sen. Creem – S.1173). An Act Relative to Wage Transparency (Rep. Josh S. Cutler – H.1950 / Sen. Patricia D. Jehlen – S.1208). Supported Items: An Act Supporting Survivors of Trafficking and Abuse and Encouraging Increased Access to Opportunities Through Expungement and/or Sealing of Records (Rep. Tram Nguyen – H.1825 / Sen. Sonia Chang-Diaz – S.947). An Act Providing Affordable and Accessible High Quality Early Education and Care to Promote Child Development and Well-being and Support the Economy in the Commonwealth (“The Common Start Legislation”) (Rep. Kenneth I. Gordon and Rep. Adrian C. Madaro – H.605 / Sen. Jason M. Lewis – S.362) An Act to Strengthen Family and Community Connection with Incarcerated People (Rep. Marjorie C. Decker – H.2440 / Sen. Sonia Chang-Diaz – S.1550). An Act Relative to Determining the Best Interest of Children in Family Court (Rep. Marjorie C. Decker – H.1528) An Act to Protect the Civil Rights and Safety of All Massachusetts Residents (“The Safe Communities Act”) (Rep. Ruth B. Balser and Rep. Liz Miranda – H.2418 / Sen. -

An Act to Promote Public Safety and Better Outcomes for Young Adults – S.825/H.3420
An Act to Promote Public Safety and Better Outcomes for Young Adults – S.825/H.3420 Lead Sponsors MASSACHUSETTS CURRENTLY SPENDS THE MOST MONEY ON Sen. Joseph Boncore (Winthrop) YOUNG ADULTS IN THE JUSTICE SYSTEM AND GETS THE Rep. James O'Day (West Boylston) Rep. Kay Khan (Newton) WORST OUTCOMES Co-Sponsors Shifting 18- to 20-year-olds into the juvenile system, where Rep. Ruth Balser (Newton) they must attend school and participate in rehabilitative Rep. Christine Barber (Somerville) programming, would lower recidivism. The young adult Sen. Michael Brady (Brockton) brain is still developing making them highly amenable to Rep. Mike Connolly (Cambridge) rehabilitation. This development is influenced – Sen. Brendan Crighton (Lynn) positively or negatively – by their environment. Rep. Daniel Cullinane (Dorchester) Sen. Julian Cyr (Truro) An overly punitive approach can actually cause more Rep. Marjorie Decker (Cambridge) Rep. Marcos Devers (Lawrence) offending: Most young people "age out" of offending by their Sen. Sal DiDomenico (Everett) mid-twenties, particularly with developmentally appropriate Rep. Daniel Donahue (Worcester) interventions. Exposure to toxic environments, like adult jails Rep. Carolyn Dykema (Holliston) and prisons, entrenches young people in problematic Sen. James Eldridge (Acton) behaviors, increasing probability of recidivism. Rep. Tricia Farley-Bouvier (Pittsfield) Sen. Cindy Friedman (Arlington) Recidivism among young people incarcerated in the adult Rep. Sean Garballey (Arlington) corrections is more than double similar youth released Rep. Carlos González (Springfield) from department of youth services commitment Rep. Tami Gouveia (Acton) Teens and young adults incarcerated in Massachusetts’ adult Rep. Jim Hawkins (Attleboro) correctional facilities have a 55% re-conviction rate, Rep. Stephan Hay (Fitchburg) compared to a similar profile of teens whose re-conviction Rep. -

Name Office Sought District
The candidates listed below have taken the Commonwealth Environmental Pledge. Name Office Sought District Gerly Adrien State Representative 28th Middlesex Representative Ruth B Balser State Representative 12th Middlesex Bryan P Barash Newton City Council Ward 2 Representative Christine P Barber State Representative 34th Middlesex Alex Bezanson State Representative 7th Plymouth 2nd Suffolk and Senator Will Brownsberger State Senate Middlesex Suezanne Patrice Bruce State Representative 9th Suffolk Michelle Ciccolo State Representative 15th Middlesex Matthew Cohen State Representative 15th Middlesex Hampshire, Franklin Jo Comerford State Senate and Worcester Representative Dan Cullinane State Representative 12th Suffolk Paul Cusack State Representative 2nd Barnstable Senator Julian Cyr State Senate Cape and Islands Representative Michael Day State Representative 31st Middlesex Representative Diana DiZoglio State Senate 1st Essex Christina Eckert State Representative 2nd Essex Representative Lori A. Ehrlich State Representative 8th Essex Middlesex and Senator James Eldridge State Senate Worcester Senator Paul Feeney State Senate Bristol and Norfolk Barnstable, Dukes and Representative Dylan Fernandes State Representative Nantucket 2nd Essex and Barry Finegold State Senate Middlesex Senator Cindy F. Friedman State Senate 4th Middlesex Representative Sean Garballey State Representative 23rd Middlesex Representative Carmine Lawrence Gentile State Representative 13th Middlesex 15 Court Square, Suite 1000, Boston, MA 02108 • (617) 742-0474 • www.elmaction.org Allison Gustavson State Representative 4th Essex Representative Solomon Goldstein-Rose State Representative 3rd Hampshire Tami Gouveia State Representative 14th Middlesex Representative Jim Hawkins State Representative 2nd Bristol Sabrina Heisey State Representative 36th Middlesex Sarah G. Hewins State Representative 2nd Plymouth Representative Natalie Higgins State Representative 4th Worcester Kevin Higgins State Representative 7th Plymouth John Hine State Representative 2nd Hampshire Senator Patricia D. -

The General Court of the Commonwealth of Massachusetts State House, Boston, MA 02133-1053
The General Court of the Commonwealth of Massachusetts State House, Boston, MA 02133-1053 April 7, 2020 David L. Bernhardt, Secretary U.S. Department of the Interior 1849 C Street, N.W. Washington DC 20240 Dear Secretary Bernhardt, We are deeply dismayed and disappointed with the Department of the Interior's recent decision to disestablish and take lands out of trust for the Mashpee Wampanoag Tribe on March 27, 2020. Not since the mid-twentieth century has an Interior Secretary taken action to disestablish a reservation. This outrageous decision comes as we mark 400 years since the arrival of the Pilgrims in 1620 and recognize the People of the First Light who inhabited these shores for centuries before contact. The Department’s capricious action brings shame to your office and to our nation. Your decision was cruel and it was unnecessary. You were under no court order to take the Wampanoag land out of trust. Further, litigation to uphold the Mashpee Wampanoag’s status as a tribe eligible for the benefits of the Indian Reorganization Act is ongoing. Your intervention was without merit and completely unnecessary. The fact that the Department made this announcement on a Friday afternoon in the midst of the COVID-19 pandemic demonstrates a callous disregard for human decency. Mashpee Wampanoag leaders were focused on protecting members of their tribe, mobilizing health care resources, and executing response plans when they received your ill-timed announcement. As you are well aware, the Department of the Interior holds a federal trust responsibility to tribes, which includes the protection of Native American lands. -

The Arc of Massachusetts 2021 2022 Legislative Platform
The Arc of Massachusetts 2021-2022 Legislative Platform DPPC Language H218 S117 — An Act updating terminology and investigative processes related to the protection of persons with disabilities Representative Sean Garballey and Senator John Keenan The bill would amend the current Disabled Person's Protection Commission's (DPPC) enabling statute to enhance protections and respect. This bill needs no appropriations yet will strengthen the DPPC's mission and align with Nicky's Law. Abuse Registry Expansion S137 — An Act to allow MassHealth Day Habilitation providers to use abuse registry Senator Mike Moore This bill will expand the abuse registry to MassHealth day program providers to ensure individuals substantiated of abuse will not be hired in other DDS day or residential programs or MassHealth day programs. Hospital Training H219 S1469 — An Act to enhance hospital care for people with intellectual and developmental disabilities, including autism through training, standards of care and certification requirements. Representative Sean Garballey and Senator Jason Lewis This bill will expand current hospital based medical providers' knowledge about autism and I/DD, in order to improve the treatment individuals receive in hospital settings. Cueing and Supervision for PCA Program H260 S129 — An Act relative to cueing and supervision in the PCA program Representative James O'Day and Senator Joan Lovely This bill amends Ch. 7 of the general law to allow the PCA program to include cueing and prompting as a covered services for those eligible members who need it. An Act Relative to Persons with Disabilities H261 S122 — An Act relative to persons with developmental disabilities Representative James O'Day and Senator Joan Lovely This bill adopts the federal definition of developmental disability in place of the current state definition of developmental disability and will amend the definition to include all adult individuals with a developmental disability, e.g. -

Preparing for a School Year Like No Other!
BOSTON TEACHERS UNION, LOCAL 66, AFT Non-Profit Org. 180 Mount Vernon Street U.S. Postage Boston, Massachusetts 02125 PAID Union Information Boston, MA you can use. Permit No. 52088 Refer to this newspaper throughout the year. EVERYONE ¡TODOS IS SON WELCOME BIENVENIDOS BBOSTON TEACHERSU HERE! AQUÍ! TUNION BT U BT U The Award-Winning Newspaper of the Boston Teachers Union, AFT Local 66, AFL-CIO • Volume 53, Number 1 • September, 2020 President’s Report Jessica J. Tang Preparing For A School Year Like No Other! ypically, each fall, we begin the new caravan and rally ending at City Hall It is only through our collective Tschool year with much anticipation, with hundreds of members, filling the action, the demonstration of our unity, hope and expectation. We eagerly pre- parking lot of Madison Park and circling strength and purpose that we have been pare our classrooms and look forward to the BPS headquarters before heading to able to make progress since the “hop- meeting new students and a fresh start. circle City Hall. scotch” plan was revealed. Since then, 2020, however, has brought unprec- We joined hundreds of educators we were able to win a delay in the start edented challenges and the usual excite- from across the state the next week for of the school year so that educators had Jessica J. Tang ment that a new school year brings has another car caravan—this time circling time to get professional development and BTU President been filled with strife and anxiety of the the State House as hundreds more educa- training in safety and health protocols. -
MA CCAN 2020 Program FINAL
Source: Ballotpedia Source: Secretary of Commonwealth Massachusetts Senate *Denotes candidate does Candidates not have a website Senate District Democratic Republican Others 1st Bristol and Plymouth District Michael Rodrigues (i)* No candidate 1st Essex District Diana DiZoglio (i) No candidate 1st Essex and Middlesex District No candidate Bruce Tarr (i) 1st Hampden and Hampshire District Eric Lesser (i) No candidate 1st Middlesex District Edward Kennedy (i) No candidate 1st Middlesex and Norfolk District Cynthia Stone Creem (i) No candidate 1st Plymouth and Bristol District Marc Pacheco (i) No candidate 1st Suffolk District Nick Collins (i) No candidate 1st Suffolk and Middlesex District Joseph Boncore (i) No candidate 1st Worcester District Harriette Chandler (i)* No candidate 2nd Bristol and Plymouth District Mark Montigny (i)* No candidate 2nd Essex District Joan Lovely (i) No candidate 2nd Essex and Middlesex District Barry Finegold (i) No candidate 2nd Hampden and Hampshire District John Velis (i) John Cain 2nd Middlesex District Patricia D. Jehlen (i) No candidate 2nd Middlesex and Norfolk District Karen Spilka (i) No candidate 2nd Plymouth and Bristol District Michael Brady (i) No candidate 2nd Suffolk District Sonia Chang-Diaz (i) No candidate 2nd Suffolk and Middlesex District William Brownsberger (i) No candidate 2nd Worcester District Michael Moore (i) No candidate 3rd Essex District Brendan Crighton (i) No candidate 3rd Middlesex District Mike Barrett (i) No candidate 1 Source: Ballotpedia Source: Secretary of Commonwealth -

Letter to Restore Asthma As a Co-Morbidity for COVID-19 Vaccines
February 12, 2021 February 12, 2021 Governor Charles Baker State House, Room 280 24 Beacon Street Boston, MA 02144 Secretary Marylou Sudders Executive OfFice oF Health and Human Services 1 Ashburton Place, 11th Floor Boston, MA 02108 Dear Governor Baker and Secretary Sudders: We write today to urge you to restore moderate to severe asthma to the list oF illnesses which constitute a co-morbidity For COVID-19 vaccine distribution and administration purposes. The CDC currently lists moderate to severe asthma as an illness that could present an increased risk For “severe illness From the virus that causes COVID-19” (https://www.cdc.gov/coronavirus/2019-ncov/need- extra-precautions/people-with-medical-conditions.html). In 2019, Springfield was described as the nation’s number one asthma capitol by the Asthma and Allergy Foundation of America (https://www.aafa.org/asthma-capitals-top-100-cities-ranking/). We believe the erroneous removal of moderate to severe asthma From the Massachusetts list oF eligible co-morbidities for phase two of the vaccination distribution must be revisited, especially when it is such a common experience among residents in the Commonwealth. Our own Massachusetts Department of Public Health has been engaged on multiple Fronts with combatting asthma in the Commonwealth, including community-based and medical interventions. Prioritizing asthma as a co-morbidity is a public health and racial equity issue. According to the MDPH, the “prevalence of current asthma in Massachusetts was higher among Black, Non-Hispanic adults than White, non-Hispanic adults.” (https://www.mass.gov/service-details/statistics-about- asthma). We recogniZe the importance oF addressing the disproportionate impact of moderate to severe asthma on black and brown communities in the Commonwealth and request that it be prioritized For vaccine distribution as a COVID-19 co-morbidity.