Dosage Form Design: Pharmaceutical and Formulation Considerations
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Softgels' Clear Advantages
DEEPDIVE REPORT March 2019 naturalproductsinsider.com Softgels’ Clear Advantages Report brought to you by DEEPDIVE REPORT Softgels’ Clear Advantages Contents Market snapshot ..................................................................................... 3 Consumer appeal .................................................................................... 4 Softgel history .......................................................................................... 6 Advantages of softgels ........................................................................... 7 How softgels are made .......................................................................... 9 Softgel challenges and solutions .......................................................11 Oxidation ...........................................................................................11 Consumer experience .......................................................................12 Dietary considerations ......................................................................12 Shelf stability ....................................................................................14 Bioavailability ....................................................................................14 Innovative developments .....................................................................16 Copyright © 2019 Informa Exhibitions LLC. All rights reserved. The publisher reserves the right to accept or reject any advertising or editorial material. Advertisers, and/or their agents, assume the -

Oral Drug Delivery: Formulation Selection Methods & Novel Delivery Technologies
ORAL DRUG DELIVERY: FORMULATION SELECTION METHODS & NOVEL DELIVERY TECHNOLOGIES OUTSTANDING ISSUE SPONSOR www.ondrugdelivery.com “Oral Drug Delivery: Formulation Selection Approaches CONTENTS & Novel Delivery Technologies” This edition is one in the ONdrugDelivery series of pub- No Longer a Hit-or-Miss Proposition: lications from Frederick Furness Publishing. Each issue focuses on a specific topic within the field of drug deliv- Once-Daily Formulation for Drugs with ery, and is supported by industry leaders in that field. pH-Dependent Solubility Gopi Venkatesh, Director of R&D & Anthony Recupero, EDITORIAL CALENDAR 2011: Senior Director, Business Development June: Injectable Drug Delivery (Devices Focus) Aptalis Pharmaceutical Technologies 4-8 July: Injectable Drug Delivery (Formulations Focus) September: Prefilled Syringes A possible approach for the desire to innovate October: Oral Drug Delivery Brian Wang, CEO & Dr Junsang Park, CSO November: Pulmonary & Nasal Drug Delivery (OINDP) GL PharmTech 10-13 December: Delivering Biotherapeutics SUBSCRIPTIONS: COMPANY PROFILE - To arrange your FREE subscription (pdf or print) to Mayne Pharma International 14-15 ONdrugDelivery, contact: Guy Furness, Publisher From Powder to Pill: A Rational Approach to T: +44 (0) 1273 78 24 24 E: [email protected] Formulating for First-into-Man Studies Dr Robert Harris, Director, Early Development SPONSORSHIP/ADVERTISING: Molecular Profiles Ltd 16-19 To feature your company in ONdrugDelivery, contact: Guy Furness, Publisher LiquiTime* Oral Liquid -

Oral Dosage Forms That Should Not Be Crushed Formulary-Specific List for VCMC and SPH
Oral Dosage Forms That Should Not be Crushed Formulary-Specific List for VCMC and SPH Generic Brand Dosage Form(s) Reasons/Comments amoxicillin-clavulanate Augmentin XR Tablet Slow-release (b,h) aspirin Aspirin EC Caplet; Tablet Slow-release; Enteric-coated aspirin and dipyridamole Aggrenox XR Capsule Slow-release atazanavir Reyataz Capsule Note: an oral powder is available, see prescribing information for administration instructions atomoxetine Strattera Capsule Note: capsule contents can cause ocular irritation - Do not open capsules as contents are an ocular irritant benzonatate Tessalon Perles Capsule Note: swallow whole; local anesthesia of the oral mucosa; choking could occur - Capsules are liquid-filled “perles” - Do not alter (break, cut, chew) integrity of dosage form; local mucosal irritant and anesthetic bisacodyl Dulcolax Capsule; Tablet Enteric-coated (c) bosentan Tracleer Tablet Note: women who are, or may become, pregnant, should not handle crushed or broken tablets brivaracetam Briviact Tablet Film-coated (b) budesonide Entocort EC Capsule Enteric-coated (a) - Capsules contain enteric-coated granules in extended-release matrix; can open capsules but do not crush contents - Products are formulated to release active drug at mid- to late small intestine buPROPion Wellbutrin XL Tablet Slow-release - Do not crush extended-release tablets - Immediate-release tablet products may be film-coated March 2019 carvedilol phosphate Coreg CR Capsule Slow-release (a) (Note: may add contents of capsule to chilled, not warm, applesauce -

A Randomized and Observer Blinded Comparison of Continuous Femoral
a & hesi C st lin e ic n a l A f R Möller. J Anesthe Clinic Res 2011, 4:1 o e l s e a Journal of Anesthesia & Clinical DOI: 10.4172/2155-6148.1000.277 a n r r c u h o J ISSN: 2155-6148 Research Case Report Open Access A Randomized and Observer Blinded Comparison of Continuous Femoral Block and Fascia Iliaca Compartment Block in Hip Replacement Surgery Thorsten Möller1,2, Sabine Benthaus2, Maria Huber2, Ingrid Bentrup2, Markus Schofer3, Leopold Eberhart2, Hinnerk Wulf2 and Astrid Morin2* 1Department of Anesthesiology and Intensive Care Medicine, Charité-Universitätsmedizin Berlin, Berlin, Germany 2Department of Anesthesiology and Critical Care Medicine, Philipps-University Marburg, Marburg, Germany 3Department of Orthopedy and Rheumatology, Philipps-University Marburg, Marburg, Germany Abstract Background: Techniques, analgesic effects and functional outcome of continuous femoral nerve and fascia iliaca compartment blocks were compared in patients undergoing hip replacement surgery. Methods: 80 patients were enroled in this randomized and observer-blinded study. 40 patients received a femoral nerve catheter with a stimulating catheter (FEM group) and 40 patients a fascia iliaca compartment catheter (FIC group). Before surgery, the catheters were placed. 50 mL prilocaine 1% was administered and a continuous infusion of ropivacaine 0.2% was maintained for 24 hours. Postoperative pain management with non-steroidal anti- inflammatory agents was standardized during the first 24 hours. No bolus application of a local anesthetic was allowed during this period. Intravenous opioide PCA with piritramide (comparable with morphin) was provided for 24 hours, and the patients were instructed to titrate their pain below a level of visual analogue scale of 3. -

An Introduction to Fast Dissolving Oral Thin Film Drug Delivery Systems: a Review
Muthadi Radhika Reddy /J. Pharm. Sci. & Res. Vol. 12(7), 2020, 925-940 An Introduction to Fast Dissolving Oral Thin Film Drug Delivery Systems: A Review Muthadi Radhika Reddy1* 1School of pharmacy, Gurunanak Institute of Technical Campus, Hyderabad, Telangana, India and Department of Pharmacy, Gandhi Institute of Technology and Management University, Vizag, Andhra Pradesh, India INTRODUCTION 2. Useful in situations where rapid onset of action Fast dissolving drug delivery systems were first developed required such as in motion sickness, allergic attack, in the late 1970s as an alternative to conventional dosage coughing or asthma forms. These systems consist of solid dosage forms that 3. Has wide range of applications in pharmaceuticals, Rx disintegrate and dissolve quickly in the oral cavity without Prescriptions and OTC medications for treating pain, the need of water [1]. Fast dissolving drug delivery cough/cold, gastro-esophageal reflux disease,erectile systems include orally disintegrating tablets (ODTs) and dysfunction, sleep disorders, dietary supplements, etc oral thin films (OTFs). The Centre for Drug Evaluation [4] and Research (CDER) defines ODTs as,“a solid dosage 4. No water is required for the administration and hence form containing medicinal substances which disintegrates suitable during travelling rapidly, usually within a matter of seconds, when placed 5. Some drugs are absorbed from the mouth, pharynx upon the tongue” [2]. USFDA defines OTFs as, “a thin, and esophagus as the saliva passes down into the flexible, non-friable polymeric film strip containing one or stomach, enhancing bioavailability of drugs more dispersed active pharmaceutical ingredients which is 6. May offer improved bioavailability for poorly water intended to be placed on the tongue for rapid soluble drugs by offering large surface area as it disintegration or dissolution in the saliva prior to disintegrates and dissolves rapidly swallowing for delivery into the gastrointestinal tract” [3]. -

Preparation and Characterization of Oil-In-Water and Water-In-Oil Emulsions
1 Preparation and Characterization of Oil-in-Water and Water-in-Oil Emulsions Prepared For Dr. Reza Foudazi, Ph.D. Chemical and Materials Engineering New Mexico State University By Muchu Zhou May 10, 2016 2 1 Introduction 1.1 Purpose of This Report The objective of this report is to clarify what I have done this semester for research course CHME 498. The research interest is “Preparation and Characterization of Oil-in-Water and Water-in-Oil Emulsions”. Thus, I would like to talk about what is emulsion, what are the main characteristics of emulsions, what are the existing methods for preparations of emulsions and how to make simple emulsions. 1.2 Background of This Report Emulsion is a kind of mixture comprised of two or more liquids, which usually are immiscible, and surfactant. The common types of emulsions are oil-in-water emulsion and water-in-oil emulsion. According to Aronson (1988), the emulsions have important industrial value in the wide range of field and it has been studied extensively recently. The emulsions play an important role in the industrial production and it has been applied to many fields including food industry, cosmetics industry and pharmaceutical industry. In the food industry, emulsifier can function as dough conditioners in order to improve tolerance to variations in flour and other ingredient quality. In the cosmetic industry, the majority of facial creams and lotions are emulsions. 1.3 Scope of This Report 3 This report is going to cover the following contents. Introduction of emulsions. Effect of surfactant. Common materials for preparation of emulsions. -

The Toxicology of Glycol Ethers and Its Relevance to Man (Fourth Edition) Volume I
The Toxicology of Glycol Ethers and its Relevance to Man (Fourth Edition) Volume I Technical Report No. 95 ISSN-0773-8072-95 Brussels, February 2005 The Toxicology of Glycol Ethers and its Relevance to Man ECETOC TECHNICAL REPORT No. 95 © Copyright – ECETOC AISBL European Centre for Ecotoxicology and Toxicology of Chemicals 4 Avenue E. Van Nieuwenhuyse (Bte 6), B-1160 Brussels, Belgium. All rights reserved. No part of this publication may be reproduced, copied, stored in a retrieval system or transmitted in any form or by any means, electronic, mechanical, photocopying, recording or otherwise without the prior written permission of the copyright holder. Applications to reproduce, store, copy or translate should be made to the Secretary General. ECETOC welcomes such applications. Reference to the document, its title and summary may be copied or abstracted in data retrieval systems without subsequent reference. The content of this document has been prepared and reviewed by experts on behalf of ECETOC with all possible care and from the available scientific information. It is provided for information only. ECETOC cannot accept any responsibility or liability and does not provide a warranty for any use or interpretation of the material contained in the publication. ECETOC TR No. 95 The Toxicology of Glycol Ethers and its Relevance to Man The Toxicology of Glycol Ethers and its Relevance to Man CONTENTS - VOLUMES I AND II EXECUTIVE SUMMARY 1 SUMMARY AND CONCLUSIONS 3 Recommendations for further work 13 1. INTRODUCTION 14 1.1 Conversion factors and physico-chemical properties 14 1.2 Production and use 14 1.2.1 Manufacture of ethylene-series glycol ethers 14 1.2.2 Manufacture of propylene-series glycol ethers 15 1.2.3 Uses 15 2. -
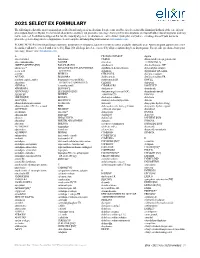
2021 SELECT EX FORMULARY the Following Is a List of the Most Commonly Prescribed Brand and Generic Medications
2021 SELECT EX FORMULARY The following is a list of the most commonly prescribed brand and generic medications. It represents an abbreviated version of the formulary list that is at the core of your prescription drug benefit plan. The list is not all-inclusive and does not guarantee coverage. Some preferred medications overlap with other clinical programs and may not be covered. In addition to drugs on this list, the majority of generic medications are covered under your plan and you are encouraged to ask your doctor to prescribe generic drugs whenever appropriate. Search complete formulary drug information at elixirsolutions.com. PLEASE NOTE: Preferred brand drugs may move to non-preferred status if a generic version becomes available during the year. Any medication approved to enter the market will not be covered until reviewed by Elixir. Not all drugs listed are covered by all prescription drug benefit programs. For specific questions about your coverage, please visit elixirsolutions.com. A B CILOXAN OINTMENT digoxin abacavir tablet balsalazide CIMDUO diltiazem ER (except generics for abacavir-lamivudine BAQSIMI cinacalcet CARDIZEM LA) ABILIFY MAINTENA [INJ] BASAGLAR [INJ] ciprofloxacin dimethyl fumarate DR* abiraterone* BD ULTRAFINE INSULIN SYRINGES ciprofloxacin-dexamethasone diphenoxylate-atropine acetic acid & NEEDLES citalopram dipyridamole ER-aspirin acitretin BELBUCA CITRANATAL divalproex sodium ACUVAIL BELSOMRA clarithromycin divalproex sodium ER acyclovir capsule, tablet benzonatate (except NDCs: clarithromycin ER DIVIGEL -

An Overview On: Sublingual Route for Systemic Drug Delivery
International Journal of Research in Pharmaceutical and Biomedical Sciences ISSN: 2229-3701 __________________________________________Review Article An Overview on: Sublingual Route for Systemic Drug Delivery K. Patel Nibha1 and SS. Pancholi2* 1Department of Pharmaceutics, BITS Institute of Pharmacy, Gujarat Technological university, Varnama, Vadodara, Gujarat, India 2BITS Institute of Pharmacy, Gujarat Technological University, Varnama, Vadodara, Gujarat, India. __________________________________________________________________________________ ABSTRACT Oral mucosal drug delivery is an alternative and promising method of systemic drug delivery which offers several advantages. Sublingual literally meaning is ''under the tongue'', administrating substance via mouth in such a way that the substance is rapidly absorbed via blood vessels under tongue. Sublingual route offers advantages such as bypasses hepatic first pass metabolic process which gives better bioavailability, rapid onset of action, patient compliance , self-medicated. Dysphagia (difficulty in swallowing) is common among in all ages of people and more in pediatric, geriatric, psychiatric patients. In terms of permeability, sublingual area of oral cavity is more permeable than buccal area which is in turn is more permeable than palatal area. Different techniques are used to formulate the sublingual dosage forms. Sublingual drug administration is applied in field of cardiovascular drugs, steroids, enzymes and some barbiturates. This review highlights advantages, disadvantages, different sublingual formulation such as tablets and films, evaluation. Key Words: Sublingual delivery, techniques, improved bioavailability, evaluation. INTRODUCTION and direct access to systemic circulation, the oral Drugs have been applied to the mucosa for topical mucosal route is suitable for drugs, which are application for many years. However, recently susceptible to acid hydrolysis in the stomach or there has been interest in exploiting the oral cavity which are extensively metabolized in the liver. -

Liposome-Based Drug Delivery Systems in Cancer Immunotherapy
pharmaceutics Review Liposome-Based Drug Delivery Systems in Cancer Immunotherapy Zili Gu 1 , Candido G. Da Silva 1 , Koen van der Maaden 2,3, Ferry Ossendorp 2 and Luis J. Cruz 1,* 1 Department of Radiology, Leiden University Medical Center, Albinusdreef 2, 2333 ZA Leiden, The Netherlands 2 Tumor Immunology Group, Department of Immunology, Leiden University Medical Center, Albinusdreef 2, 2333 ZA Leiden, The Netherlands 3 TECOdevelopment GmbH, 53359 Rheinbach, Germany Received: 1 October 2020; Accepted: 2 November 2020; Published: 4 November 2020 Abstract: Cancer immunotherapy has shown remarkable progress in recent years. Nanocarriers, such as liposomes, have favorable advantages with the potential to further improve cancer immunotherapy and even stronger immune responses by improving cell type-specific delivery and enhancing drug efficacy. Liposomes can offer solutions to common problems faced by several cancer immunotherapies, including the following: (1) Vaccination: Liposomes can improve the delivery of antigens and other stimulatory molecules to antigen-presenting cells or T cells; (2) Tumor normalization: Liposomes can deliver drugs selectively to the tumor microenvironment to overcome the immune-suppressive state; (3) Rewiring of tumor signaling: Liposomes can be used for the delivery of specific drugs to specific cell types to correct or modulate pathways to facilitate better anti-tumor immune responses; (4) Combinational therapy: Liposomes are ideal vehicles for the simultaneous delivery of drugs to be combined with other therapies, including chemotherapy, radiotherapy, and phototherapy. In this review, different liposomal systems specifically developed for immunomodulation in cancer are summarized and discussed. Keywords: liposome; drug delivery; cancer immunotherapy; immunomodulation 1. The Potential of Immunotherapy for the Treatment of Cancer Cancer immunotherapy has been widely explored because of its durable and robust effects [1]. -

Intra-Luminal Focused Ultrasound for Augmentation of Gastrointestinal Drug Delivery
Editorial Page 1 of 2 Intra-luminal focused ultrasound for augmentation of gastrointestinal drug delivery Ezekiel Maloney1, Joo Ha Hwang2 1Department of Radiology, 2Division of Gastroenterology, Department of Medicine, University of Washington, Seattle, WA, USA Correspondence to: Joo Ha Hwang, MD, PhD. Division of Gastroenterology, Department of Medicine, University of Washington, Box 359773, 325 Ninth Avenue, Seattle, WA 98104, USA. Email: [email protected]. Provenance: This is a Guest Editorial commissioned by Section Editor Hui Kong, MD, PhD (Department of Respiratory Medicine, The First Affiliated Hospital of Nanjing Medical University, Nanjing, China). Comment on: Schoellhammer CM, Schroeder A, Maa R, et al. Ultrasound-mediated gastrointestinal drug delivery. Sci Transl Med 2015;7:310ra168. Submitted Feb 01, 2017. Accepted for publication Feb 06, 2017. doi: 10.21037/atm.2017.03.42 View this article at: http://dx.doi.org/10.21037/atm.2017.03.42 The recent article by Schoellhammer et al., “Ultrasound- intensity ultrasound frequencies followed by quantification mediated gastrointestinal drug delivery” primarily of delivery of permeants (e.g., glucose, dextran, insulin). addresses practical limitations in drug delivery for medical Treated tissues showed enhanced transport. Similar management of inflammatory bowel disease (IBD), and findings were demonstrated in small and large bowel tissue presents pre-clinical data demonstrating that intra- for radiolabeled mesalamine and hydrocortisone. With 1 luminal, sub-ablative focused ultrasound (FUS), delivered minute of ultrasound treatment time, 3–5-fold improved via a trans-rectal transducer, can overcome some of these drug delivery was observed versus control. Additional limitations (1). The clinical application and benefit of such a ex vivo experiments utilizing variable FUS protocols to device is clear. -

Comprehensive Review on Herbal Toothpaste
Annals of R.S.C.B., ISSN:1583-6258, Vol. 25, Issue 4, 2021, Pages. 9509 - 9518 Received 05 March 2021; Accepted 01 April 2021. Comprehensive Review on Herbal Toothpaste Divya S1, Dr. J Suresh1*, Dr. S. Meenakshi 2 1. Department of Pharmacognosy, JSS College of Pharmacy, JSS Academy of Higher Education & Research, Mysuru-570015 2.Department of Prosthodontics, JSS Dental College, JSS Academy of Higher Education &Research, Mysuru-570015 Corresponding author Dr. J. Suresh Professor Department of Pharmacognosy, JSS College of Pharmacy, JSS Academy of Higher Education & Research, Mysuru-570015 Email: [email protected] Mobile No: 9480197611 ABSTRACT Herbal products for general as well as for oral health care have gained prominence around worldwide. People who aspire towards the use of herbal products often consider these products are relatively safer than products containing synthetic ingredients. Based on increased usage of herbal cosmetics we tried to make a comprehensive review on herbal toothpaste that helps to maintain a proper oral hygiene and free from periodontal disorder, reduce stain, gingivitis, calculus and caries. The present review gives basic information regarding antimicrobial potential of various herbs, formulationexcipients, that can be used in preparation of toothpaste. Key Words: Herbal toothpaste, Anti-microbial screening, Periodontal disorder, Gingivitis, calculus, Dental caries. INTRODUCTION In developing countries, the intensity of infections caused by certain pathogenic micro- organisms that may leads to mortality as well as morbidity in immune-suppressant patients [1]. Multiple abrasives, scent, green lead was used to remove the stain from teeth until mid- 19thcentury. In Medieval period rock salt, fine sand were the key ingredients used by Arabs for tooth cleaning.In the period 1950 AD, Dr.