91St Inaugural Lecture of the University of Port Harcourt-UNIQUE UNIPORT
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Jurnal Sosialisasi Reinventing the Theatre Curriculum to Address
Jurnal Sosialisasi Jurnal Hasil Pemikiran, Penelitian, dan Pengembangan Keilmuan Sosiologi Pendidikan Vol. 8, Nomor 2, Juli 2021 Reinventing the Theatre Curriculum to Address Contemporary Development Needs and Job Alignment in Nigeria Esekong H. Andrew-Essien Department of Theatre and Media Studies University of Calabar, Nigeria [email protected] ABSTRACT As the social and economic terrain is changing in Nigeria, theatre training and practice have not evolved commensurately to address the current development needs and job alignment. The models used in many Nigerian universities mainly offer theoretical knowledge of theatre and basic training for entertainment roles. Even though the philosophy and objectives of theatre training in the NUC Benchmark for minimum academic standards are couched with the anticipation for innovation and programme expansion, it does not specify the type or scope of expansion needed to retain the viability of theatre practice within the current knowledge economy. Nigerian universities are therefore not firmly guided to develop their theatre curricula in a direction that is sensitive to the exigencies of time and age. There is currently a lot of interest in film production, carnival, standup comedy, development communication, applied theatre and event management. This paper argues that theatre and performing art programmes in universities and other theatre training centres should develop more courses around these emerging areas of interest. The paper submits that while there are many specialties in which theatre graduates can be professionally engaged, and while the nature of theatre training imbues numerous subjective qualities desired in the contemporary world of work, much more could be done by reinventing the theatre curriculum to give theatre graduates wider opportunities. -
Election Report 3Rd EDITION
N O I T C E BROADCAST MEDIA L E L COVERAGE OF 2019 A R E N E NIGERIA G A I GENERAL ELECTION R E G I APRIL-JUNE, N 9 1 2019 0 2 F O E G A R E V O C A I D E M T S A C D A O R B S M I BROADCAST MEDIA COVERAGE OF 2019 NIGERIA GENERAL ELECTION APRIL-JUNE, , 2019 IMS European Union Published in 2020 By Institute for Media and Society (IMS) 3, Emina Crescent, Off Toyin Street, Ikeja, Lagos, Nigeria. Email: [email protected] [email protected] Website: www.imesoimeso.org DISCLAIMER This publication has been produced with the assistance of the European Union. The contents of this publication are the sole responsibility of the Institute for Media and Society, and can in no way be taken to reflect the views of the European Union. Funded by the EUROPEAN UNION iv C O N T E N T S FOREWORD vi ACKNOWLEDGEMENTS viii APRIL 2019 REPORT 9 PART I: CONTENTS OF POLITICAL PROGRAMMES ON 12 RADIO PART II: CONTENTS OF POLITICAL PROGRAMMES ON 23 TELEVISION PART III: COMBINED REPORT ON RADIO AND TELEVISION 34 MAY 2019 REPORT 45 PART I: CONTENTS OF POLITICAL PROGRAMMES ON RADIO 48 PART II: CONTENTS OF POLITICAL PROGRAMMES ON 58 TELEVISION PART III: COMBINED REPORT ON RADIO AND TELEVISION 68 JUNE 2019 REPORT 80 PART I: CONTENTS OF POLITICAL PROGRAMMES ON RADIO 83 PART II: CONTENTS OF POLITICAL PROGRAMMES ON 92 TELEVISION PART III: COMBINED CONTENTS OF POLITICAL 102 BROADCASTS FOR DECEMBER 2019 APRIL - JUNE 2019 REPORT 112 PART I: CONTENTS OF RADIO BROADCASTS 1N THE SECOND 115 QUARTER OF 2019 PART II: CONTENTS OF TELEVISION BROADCASTS 1N THE 127 SECOND QUARTER OF 2019 PART III: COMBINED CONTENTS OF RADIO AND TELEVISION 138 BROADCASTS IN THE SECOND QUARTER OF 2019 v F O R E W O R D The Institute for Media and Society established a Media Monitoring activity in 2018 within the context of the Support to Media component of the European Union Support to Democratic Governance in Nigeria (EU-SDGN) Project. -
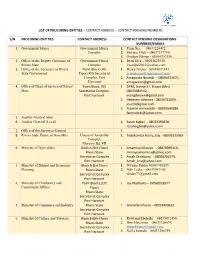
List of Procuring Entities – Contact Address – Contact Persons/Numbers
LIST OF PROCURING ENTITIES – CONTACT ADDRESS – CONTACT PERSONS/NUMBERS S/N PROCURING ENTITIES CONTACT ADDRESS CONTACT PERSONS-DESIGNATIONS- NUMBERS/EMAILS 1. Government House Government House 1. Perm Sec. – 08037224492 Complex 2. Margret Dick – 08037277770, 3. Oyoboy Edman - 08036757330 2. Office of the Deputy Governor of Government House 1. Iwari Jack – 08055625938, Rivers State Complex [email protected] 3. Office of the Secretary to Rivers Point Block (4th 1. Henry Nzeka – 08038831847, State Government Floor),R/S Secretariat [email protected] Complex, Port 2. Amagwula Nnamdi – 08064525671, Harcourt [email protected] 4. Office of Head of Service of Rivers Point Block, R/S 1 DPRS, Inyingi S.I. Brown (Mrs) - State Secretariat Complex, 08033384942, Port Harcourt [email protected] 2 Hekerem Adanma - 08036721069, [email protected] 3 Franklin Aminadoki – 08035640289 [email protected] 5. Auditor -General State 6. Auditor General (Local) 1. Sarah Kigbel - 08033393878 [email protected] 7. Office of the Surveyor-General 1. 8. Rivers State House of Assembly House of Assembly 1. Tubokomba Harry, Esq. - 08033125065 Complex Moscow Rd, PH 9. Ministry of Agriculture Block A (5th Floor) 1. Amamina Minaiyo - 08078969110, Rivers State [email protected] Secretariat Complex 2. Amah Christiana - 08036702579, Port Harcourt [email protected] 3. Ministry of Budget and Economic Block B (1st Floor) 1. Nwume Friday 08039382679 Planning Rivers State 2. Ndii Ledee - 08033097140 Secretariat Complex [email protected] Port Harcourt 4. Ministry of Chieftaincy and Point Block (11th 1. Joy Wariboko – 07068018977 Community Affairs Floor) Rivers State Secretariat Complex Port Harcourt 5. Ministry of Commerce and Industry Rivers State 1. Granville Elfreda – 08033409613 Secretariat Complex Port Harcourt 6. -

Download Attachment
3 4 5 6 7 8 9 10 11 12 13 2019 BUDGET SPEECH DELIVERED BY HIS EXCELLENCY, CHIEF NYESOM EZENWO WIKE, CON, GSSRS, POS (AFRICA), THE EXECUTIVE GOVERNOR, RIVERS STATE ON THE OCCASION OF BUDGET PRESENTATION TO THE RIVERS STATE HOUSE OF ASSEMBLY. Mr Speaker, Principal Officers of the House, Honourable Members, Distinguished Guests, Ladies and Gentlemen. It is my privilege and joy to stand before this great Assembly to present the First Budget Estimates of our second term administration being the Budget for the 2019 Fiscal Year. 2. It is demanded of every conscientious and people-oriented Government to account for its stewardship and also provide a road map for future activities and engagements. This 2019 Budget meets these criteria. It provides a detailed account of our stewardship for the past three years of our Administration and in particular, the year 2018 in relation to our electioneering promises to our people and more importantly, provides the vision, articulates the mission and directs the energies of the Government and our people for the upcoming year. 3. On this note, Mr. Speaker, the 2019 Budget has been christened ''the Budget of Re-evaluation for a New Beginning”. Re- evaluation in the sense that having made remarkable progress in the fulfilment of our campaign promises to our dear people of Rivers State in the areas of infrastructure, security, education, health, youth employment and women empowerment, agriculture, human capital development as well as social welfare; it is wise for us to pause and examine our efforts and chart a new course for a new beginning. -

Application of Ict in Television Broadcasting: a Study of Nta Port Harcourt
Stella Eludu et al., IJSIT, 2016, 5(2), 169-182 APPLICATION OF ICT IN TELEVISION BROADCASTING: A STUDY OF NTA PORT HARCOURT 1Stella Eludu, 2Mbazie Sunny and 3Ndinojuo Ben-Collins Emeka 1,2,3Department of linguistics and Communication Studies, University of Port Harcourt, Rivers State Nigeria ABSTRACT Information and communication technology, ICT, has revolutionized the media industry. It has transformed information gathering and dissemination in television broadcasting. This study examines the application of ICT by broadcast professionals of Nigerian Television Authority, NTA Channel 10, Port Harcourt. The objectives of the study were to examine the extent NTA makes use of ICT in its broadcasting; to find out if NTA uses website(s) for broadcasting and to identify the benefits of ICT to broadcast professionals of NTA. Survey design was adopted for the study using personal interview and the data collected was qualitative. The study revealed that ICTs have been widely applied in television broadcasting by broadcast professionals at Nigeria Television Authority, NTA, Channel 10, Port Harcourt. Study results also showed that NTA Port Harcourt does not have a website whereas the benefits of using ICTs by broadcast professionals of NTA Port Harcourt include ease of communication and easier access to information using the internet and shared network, amongst a host of other benefits. The recommendations for this study include making funds available to upgrade ICT facilities and NTA Port Harcourt should have its own website in order to control its online identity, image and domain email accounts for staff. Keywords: ICT; Television; NTA; Broadcasting 169 IJSIT (www.ijsit.com), Volume 5, Issue 2, March-April 2016 Stella Eludu et al., IJSIT, 2016, 5(2), 169-182 INTRODUCTION It is contestable that Marshal McLuhan had information communication technology (ICT) in mind several decades ago when he coined the phrase “global village” to prophesy that the electronic communicatiown would unite the world. -
University of Port Harcourt
UNIVERSITY OF PORT HARCOURT FACULTY OF HUMANITIES DEPARTMENT OF LINGUISTICS AND COMMUNICATION STUDIES ASSIGNMENT Investigate the organizational structure of Rivers State Television (RSTV) and give the number of journalist, also quoting your source of information. PRESENTED BY EKEANYANWU, EBUKA (U2008/1825294) COURSE CODE: LCS 416.1 COURSE TITLE: MEDIA MANAGEMENT COURSE LECTURER: MR. ASAK HISTORY OF RIVERS STATE TELEVISION (RSTV) Rivers State Television, the pioneer television station of Rivers State Nigeria, came into existence on 31st December, 1974. Its initial take off location was Mgbuoba along Choba Road. RSTV transmitted under the headship of Mr. Gabriel Okara, the first General Manager of the Television Station. However, in 1976, there was a change in ownership of the station, as the federal government decided to take over all existing television stations in the country. By virtue of Decree No. 24 of 1977, Nigerian Television Authority (NTA) was charged with the responsibility of coordinating the activities of television stations across the country and following this development, the property of RSTV was taken over by NTA, Port Harcourt. In 1979, the Chief Melford Okilo civilian administration in Rivers State set up a committee to work out modalities and recommend the establishment of a state-owned television station. Under the supervision of Rivers State Broadcast Corporation (RSBC) alias Radio Rivers, Rivers State Television was resuscitated. In May, 1983, the station commenced test transmission of a one (1) kilowatt transmitter, and transmission lasted till 31st December 1983 when the station went off-air, as a result of a Buhari led coup d’état which ousted the government of Alhaji Shehu Shagari. -

IMSU JOURNAL of COMMUNI VOL, 3.Cdr
IMSU JOURNAL OF COMMUNICATION STUDIES A PUBLICATION OF THE DEPARTMENT OF MASS COMMUNICATION, IMO STATE UNIVERSITY, OWERRI VOLUME 3 ISSN: 2682-6321 E-ISSN: 2705-2240 2019 IMSU Journal of Communication Studies, Vol. 3, 2019 @copyright IMSU JCS 2019 All Rights Reserved No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form by means of electronics, mechanical, photocopying, recording or otherwise without the prior written permission of the publisher. ii IMSU Journal of Communication Studies, Vol. 3, 2019 ABOUT IMSU JOURNAL OF COMMUNICATION STUDIES (IMSU JCS) IMSU Journal of Communication Studies (IMSU JCS) is a blind peer reviewed journal published annually by the Department of Mass Communication, Imo State University, Owerri. The journal accepts papers from all areas of Mass Communication and other communication related discipline. The journal accepts both empirical and position papers of high quality. All articles for submission must be original to the author(s) and free from plagiarism. The purpose of IMSU Journal of Communication Studies is to contribute to the body of knowledge in the field of communication and media studies. The journal is both in print and electronic version. The electronic version is an open access journal. Author shall be entitled to one copy of the volume in which his/her article appears. In the case of a co-author, the authors shall have only one complimentary copy and will be given more copies upon request and payment of certain amount which will be stipulated. Author(s) are expected to have their work written in UK English with proper grammar and spellings. -

Christian Churches and Nigeria's Political Economy of Oil and Conflict Ix
Christian Churches and Nigeria’s Political Economy of Oil and Conflict Christian Churches and Nigeria’s Political Economy of Oil and Conflict: Baptist and Pentecostal Perspectives By Nkem Emerald Osuigwe Christian Churches and Nigeria’s Political Economy of Oil and Conflict: Baptist and Pentecostal Perspectives, by Nkem Emerald Osuigwe This book first published 2014 Cambridge Scholars Publishing 12 Back Chapman Street, Newcastle upon Tyne, NE6 2XX, UK British Library Cataloguing in Publication Data A catalogue record for this book is available from the British Library Copyright © 2014 by Nkem Emerald Osuigwe All rights for this book reserved. No part of this book may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without the prior permission of the copyright owner. ISBN (10): 1-4438-6123-5, ISBN (13): 978-1-4438-6123-6 To the memory of my late parents and all the innocent victims of the Niger Delta conflict TABLE OF CONTENTS Figures and Tables ....................................................................................... x Foreword .................................................................................................... xi List of Abbreviations ................................................................................ xiii Acknowledgements ................................................................................... xv Chapter One ................................................................................................ -
How to Set up and Manage a Community Journalism Network
HOW TO SET UP AND MANAGE A COMMUNITY JOURNALISM NETWORK Implemented by Adam Smith International 1 How to Set Up and Manage a Community Journalism Network Preface Nigeria is blessed with numerous media organisations (though analysts are still asking for more), from the print – newspapers, magazines and other periodicals to broadcast – radio, television, satellite stations and online media. As of November 2016, there were over three hundred radio stations, one hundred television stations, thirty Internet radio stations, six international broadcasters across Nigeria and still counting. There were also sixty-six newspapers and magazines across the country during the same period1 Nigeria also enjoys relative freedom of the press when compared with some other African, Asian, Caribbean or even European countries. However, ninety per cent of Nigeria’s media spread are in the urban centres, leaving the remaining ten per cent to the semi urban fringes, with virtually no newspaper, radio or television station located in any remote, rural village. The implication of this, is that news coverage, programme focus, analyses and general perspectives on issues centre on the urban and semi urban areas, leaving the rural settlers, who contributed a chunk of Nigeria’s population with neither a voice nor fair representation in the media. This is what led to the community journalism initiative. Enhancing Nigeria’s Advocacy for Better Business Environment Phase 2 (ENABLE2), as part of its intervention to improve the professional competence of the Nigerian media in the coverage of small business women and men 1 See list of Nigerian media organisations in appendix 1 How to Set Up and Manage a Community Journalism Network 2 and the smallholder farmers in the rural communities, embarked on this initiative. -

Prioritizing Eco-Cultural Tourism Development in Nigeria for Wealth Generation and Sustainable Development
IIARD International Journal of Geography and Environmental Management ISSN 2504-8821 Vol. 4 No. 4 2018 www.iiardpub.org Prioritizing Eco-Cultural Tourism Development in Nigeria for Wealth Generation and Sustainable Development Ukpere, Dennis R. Tobins (PhD) Department of Geography and Environmental Studies Faculty of Social Sciences Rivers State University of Education Rumuolumeni, P.M.B. 5047 Port Harcourt Nigeria [email protected], [email protected] Wabah, Goodnews (PhD) Department of Sociology Faculty of Social Sciences Rivers State University of Education Rumuolumeni, P.M.B. 5047 Port Harcourt Nigeria Abstract This paper presents an expository examination of the roles of eco-cultural tourism for sustainable national development. It examined the aesthetical and utilitarian value of museums and cultural festivals in Nigeria by highlighting the combine impacts of the geo- spatial alignment between economics, cultural festivals and tourism in nation building through job creation, income generation, development of ancillary industries, increase in investments, opening-up of the hinterlands and strengthening of cultural values. The paper argued that, there is a global paradigm shift from over reliant on export earnings from natural resources to the promotion of geo-spatial eco-cultural tourism to boost employment and revenue generation. Nigeria is blessed with lots of tourism potentials. According to the authors, the right recipe for sustainable eco-cultural tourism business is for us to properly coordinate, utilize and package the nation’s rich cultural festivals and potential tourists’ sites. The paper however, decried the lack of a clearly defined road map on tourism development and concluded by stressing that instead of relying on non-renewable resources (e.g. -

Government of Rivers State of Nigeria Committee for the Accreditation Status and Approval of Private Schools Summary Sheet
GOVERNMENT OF RIVERS STATE OF NIGERIA COMMITTEE FOR THE ACCREDITATION STATUS AND APPROVAL OF PRIVATE SCHOOLS SUMMARY SHEET RIVERS SOUTH-EAST OYIGBO LGA S/N NAME OF SCHOOL SCHOOL ADDRESS ACCREDITATION Alpha Missionary Group of Schools 1 1 Alpha Close by Ohita Lane, Oyigbo INTERIM (Secondary) Anerobi International College 2 Afam Rd, Izuoma, Oyigbo INTERIM (Secondary) Bee Mec Model School (Nursery & 3 Izioma Asa Oyigbo INTERIM Primary) No 3 Unity Avenue, Off Isaiah Eletue Street, 4 Blessed Model Secondary School INTERIM Oyigbo Bravery Int'l School (Nursery & 5 9 Chris Avenue, Off 117 Afam Road, Oyigbo INTERIM Primary) Bright Kids Academy (Nursery & 6 Double Portion Avenue/Ogboso Obeama INTERIM Primary) 7 C. Conud Brain International School 6/7 Eberechi Str, Komkom, Oyigbo INTERIM 8 Calebs Model School Afam-Okoloma INTERIM Calvary Stars Montessori Group of Chief Nwadike Street off Tiper Park/seventh 9 INTERIM Schools (Nursery & Primary) days Adventist Church Mirinwayi-Asa Oyigbo 10 Champions Missionary School 33 Ekweru Ave, Mbano-Camp, Oyigbo INTERIM 3 Ndikelionwu Str, Satellite Village, Near 11 Charlaw Preparatory Academy INTERIM Timber Mkt, Oyigbo NO. NEW JERUSALEM, UMUEKE OBEAMA- 12 CHEZ BRAIN ACADEMY (Secondary) INTERIM ASA, OYIGBO 13 Chidan International School 1 Stino Close, Off Ehi Rd, Oyigbo INTERIM Chimac International School 14 Jeremiah Nwaji Str, Behind Bush Bar, Oyigbo INTERIM (Secondary) Covenant Joint Heirs Montessori 15 4 Umukam Street Oyigbo INTERIM Schools (Nursery & Primary) DAiLY quintessential QUEENS & KING 30 NWEKE STREET, Off Umusoya Road, 16 INTERIM ACADEMY (SECONDARY SCHOOL) OYIGBO No 11 Onyeche Street Okpulor Beside 17 De Kindlers' Int'l (Nursery & Primary) INTERIM Assemblies of God DE-SHILOH'S SCHOOL (NURSERY & OPPOSITE BISHOP OKOYE SECONDARY 18 INTERIM PRIMARY) SCHOOL, MIRINWANYI OYIGBO St. -

Accredited Laboratory
LAGOS ZONE S/N NAME OF COMPANY TYPE OF SERVICES ADDRESS 1 Environmental Resources Environmental Quality Monitoring, Block 61, Plot 11, Osaro Managers Limited Biomonitoring and Biodegradability Isokpan Street, Off Theophilus Services (Toxicity Analysis) Oji, Off Fola Osibo Rd Lekki Phase 1, Lagos 2 Searchgate Laboratories Environmental Quality Monitoring, 38, Diya Street Ifeko, Limited Biomonitoring and Biodegradability Gbagada, Lagos Services (Toxicity Analysis) 3 Nigerian Institute for Environmental Quality Monitoring, 3 Wilmot Point Raod, Bar- Oceanography and Biomonitoring and Biodegradability Beach, Victoria Island, Lagos Marine Studies (Toxicity Testing) Research (NIOMR) 4 Etina Environmental Biomonitoring and Biodegradability 34, Anite Crescent, Off Okota Services Limited Services (Toxicity Testing) Road, Isolo, Lagos 5 Jawura Environmental Environmental Quality Monitoring 130 Awolowo Way, Balogun Services Limited Services Bus stop, Ikeja, Lagos 6 Intertek Testing Services Petroleum Quality Monitoring 73B Marine Road, Apapa, Nigeria Limited Services (Petroleum Products Lagos Quality Analysis- PMS, AGO, HHK & Fuel Oils) 7 Clairgold Oil and Gas Petroleum Quality Monitoring 10, Ibiere Crescent, Off Kofo Engineering Limited Services (Petroleum Products Abayomi, Apapa, Lagos Quality Analysis- PMS, HHK & AGO) 8 Q & Q Control Services Petroleum Quality Monitoring 5C Oju Olobun Close, Nigeria Limited Services (Petroleum Products Victoria Island, Lagos Quality Analysis- PMS, HHK & AGO) 9 Spectrum Inspection Petroleum Quality Monitoring 4/5