An Overview of the MATH+, I-MASK+ and I-RECOVER Protocols a Guide to the Management of COVID-19
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Daft Punk Collectible Sales Skyrocket After Breakup: 'I Could've Made
BILLBOARD COUNTRY UPDATE APRIL 13, 2020 | PAGE 4 OF 19 ON THE CHARTS JIM ASKER [email protected] Bulletin SamHunt’s Southside Rules Top Country YOURAlbu DAILYms; BrettENTERTAINMENT Young ‘Catc NEWSh UPDATE’-es Fifth AirplayFEBRUARY 25, 2021 Page 1 of 37 Leader; Travis Denning Makes History INSIDE Daft Punk Collectible Sales Sam Hunt’s second studio full-length, and first in over five years, Southside sales (up 21%) in the tracking week. On Country Airplay, it hops 18-15 (11.9 mil- (MCA Nashville/Universal Music Group Nashville), debutsSkyrocket at No. 1 on Billboard’s lion audience After impressions, Breakup: up 16%). Top Country• Spotify Albums Takes onchart dated April 18. In its first week (ending April 9), it earned$1.3B 46,000 in equivalentDebt album units, including 16,000 in album sales, ac- TRY TO ‘CATCH’ UP WITH YOUNG Brett Youngachieves his fifth consecutive cording• Taylor to Nielsen Swift Music/MRCFiles Data. ‘I Could’veand total Made Country Airplay No.$100,000’ 1 as “Catch” (Big Machine Label Group) ascends SouthsideHer Own marks Lawsuit Hunt’s in second No. 1 on the 2-1, increasing 13% to 36.6 million impressions. chartEscalating and fourth Theme top 10. It follows freshman LP BY STEVE KNOPPER Young’s first of six chart entries, “Sleep With- MontevalloPark, which Battle arrived at the summit in No - out You,” reached No. 2 in December 2016. He vember 2014 and reigned for nine weeks. To date, followed with the multiweek No. 1s “In Case You In the 24 hours following Daft Punk’s breakup Thomas, who figured out how to build the helmets Montevallo• Mumford has andearned Sons’ 3.9 million units, with 1.4 Didn’t Know” (two weeks, June 2017), “Like I Loved millionBen in Lovettalbum sales. -

Super Green Superfoods
[Plant-Based Ingredients] Vol. 17 No. 12 December 2012 Super Green Superfoods By Celeste Sepessy, Associate Editor Once the secret of Birkenstock-wearing progressives, green foods are now filling the shopping carts of informed—if not guilty—conventional consumers. Nutrient-dense greens date back millions of years, and humans in the know have been eating them for centuries; green foods manufacturers commonly tout their ingredients as the energy food of ancient Mesoamericans, namely the Aztecs. The term "green foods" encompasses a range of raw materials including algae (chlorella, spirulina, etc.), grasses (alfalfa, barley grass, wheat grass, etc.) and common green vegetables (broccoli, spinach, etc.). Though each ingredient boasts its own benefits, they all pack a well-rounded nutritional punch not often found elsewhere. "Spirulina is nature's multivitamin," said John Blanco, president of AnMar International, noting the microalgae has 60-percent protein, unsaturated fatty acids and vitamin precursors, such as amino acids and proenzymes. "It's not a complete 100-percent balanced vitamin tablet, but it's pretty close." And this nutritional breakdown is similar across the green board, as the ingredients are densely filled with phytonutrients, antioxidants, vitamins, minerals and nucleic acid, among other nutrients. Consumers of all demographics are becoming more aware of the benefits of eating these green superfoods; Guinevere Lynn, director of business development at Sun Chlorella, pointed to the media for the industry's popularity surge. "Mass media has certainly played a major role in this 'green renaissance,' " she explained, citing Dr. Oz's help in particular. The television medical personality is a huge proponent of green foods, and Dr. -
Extended-Release 30 Mcg Capsules Service Request Form Fax: 1-844-660-7083 | Phone: 1-844-414-Opko (6756) E-Mail: [email protected]
RAYALDEE® (CALCIFEDIOL) EXTENDED-RELEASE 30 MCG CAPSULES SERVICE REQUEST FORM FAX: 1-844-660-7083 | PHONE: 1-844-414-OPKO (6756) E-MAIL: [email protected] 1. Patient Information Please complete all fields to prevent any delays. New start to Rayaldee® therapy Existing patient on therapy E-mail Address: Preferred Method of Contact: Cell Phone Home Phone Email Text First Name Last Name SS # (Last 4 only) Preferred Time of Contact: Morning Afternoon Evening Male Female Ok to leave a message: Yes No Date of Birth (MM/DD/YYYY) Primary Language: English Spanish Other:________________________________ 2. Patient Insurance Information Address Attached is a copy of both sides of the patient's insurance card City State ZIP Primary Insurance Phone # Cell Phone Home Phone Policy Holder Name Relationship to Patient Alternate Contact or Healthcare Proxy First Name, Last Name and Phone Insurance ID # Group # 3. Patient Clinical Information Please include supporting clinical documentation. ● ICD-10 Code: ● Lab Values & dates: Please check box 1. or 2. below 25(OH)D__________|__________ Calcium__________|__________ (N18.3) CKD stage 3, (N25.81) Secondary hyperparathyroidism, and 1. value date value date (E55.9) Vitamin D deficiency 2. (N18.4) CKD stage 4, (N25.81) Secondary hyperparathyroidism, and (E55.9) Vitamin D deficiency ● Therapies within the previous 6 months: No previous therapies Hectorol® (doxercalciferol) Rocaltrol® (calcitriol) OTC Vitamin D2 ® OTC Vitamin D3 Prescription Vitamin D2 (ergocalciferol) Zemplar (paricalcitol) 4. Prescriber Information Specialty of Prescriber: Nephrologist PCP Endocrinologist Internist First Name Last Name Phone Fax Practice Name Oce Contact Preferred Time of Contact Address NPI # City State ZIP 5. -

INVESTIGATION of NATURAL PRODUCT SCAFFOLDS for the DEVELOPMENT of OPIOID RECEPTOR LIGANDS by Katherine M
INVESTIGATION OF NATURAL PRODUCT SCAFFOLDS FOR THE DEVELOPMENT OF OPIOID RECEPTOR LIGANDS By Katherine M. Prevatt-Smith Submitted to the graduate degree program in Medicinal Chemistry and the Graduate Faculty of the University of Kansas in partial fulfillment of the requirements for the degree of Doctor of Philosophy. _________________________________ Chairperson: Dr. Thomas E. Prisinzano _________________________________ Dr. Brian S. J. Blagg _________________________________ Dr. Michael F. Rafferty _________________________________ Dr. Paul R. Hanson _________________________________ Dr. Susan M. Lunte Date Defended: July 18, 2012 The Dissertation Committee for Katherine M. Prevatt-Smith certifies that this is the approved version of the following dissertation: INVESTIGATION OF NATURAL PRODUCT SCAFFOLDS FOR THE DEVELOPMENT OF OPIOID RECEPTOR LIGANDS _________________________________ Chairperson: Dr. Thomas E. Prisinzano Date approved: July 18, 2012 ii ABSTRACT Kappa opioid (KOP) receptors have been suggested as an alternative target to the mu opioid (MOP) receptor for the treatment of pain because KOP activation is associated with fewer negative side-effects (respiratory depression, constipation, tolerance, and dependence). The KOP receptor has also been implicated in several abuse-related effects in the central nervous system (CNS). KOP ligands have been investigated as pharmacotherapies for drug abuse; KOP agonists have been shown to modulate dopamine concentrations in the CNS as well as attenuate the self-administration of cocaine in a variety of species, and KOP antagonists have potential in the treatment of relapse. One drawback of current opioid ligand investigation is that many compounds are based on the morphine scaffold and thus have similar properties, both positive and negative, to the parent molecule. Thus there is increasing need to discover new chemical scaffolds with opioid receptor activity. -
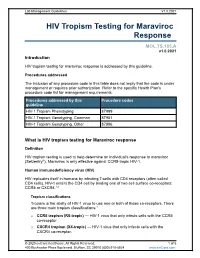
HIV Tropism Testing for Maraviroc Response
Lab Management Guidelines V1.0.2021 HIV Tropism Testing for Maraviroc Response MOL.TS.185.A v1.0.2021 Introduction HIV tropism testing for maraviroc response is addressed by this guideline. Procedures addressed The inclusion of any procedure code in this table does not imply that the code is under management or requires prior authorization. Refer to the specific Health Plan's procedure code list for management requirements. Procedures addressed by this Procedure codes guideline HIV-1 Tropism Phenotyping 87999 HIV-1 Tropism Genotyping, Common 87901 HIV-1 Tropism Genotyping, Other 87906 What is HIV tropism testing for Maraviroc response Definition HIV tropism testing is used to help determine an individual's response to maraviroc (Selzentry®). Maraviroc is only effective against CCR5-tropic HIV-1. Human immunodeficiency virus (HIV) HIV replicates itself in humans by infecting T-cells with CD4 receptors (often called CD4 cells). HIV-1 enters the CD4 cell by binding one of two cell surface co-receptors: CCR5 or CXCR4.1,2 Tropism classifications Tropism is the ability of HIV-1 virus to use one or both of these co-receptors. There are three main tropism classifications:3 o CCR5 tropism (R5-tropic) — HIV-1 virus that only infects cells with the CCR5 co-receptor. o CXCR4 tropism (X4-tropic) — HIV-1 virus that only infects cells with the CXCR4 co-receptor. © 2020 eviCore healthcare. All Rights Reserved. 1 of 5 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Lab Management Guidelines V1.0.2021 o Dual or mixed tropism (D/M-tropic) — HIV-1 virus populations that can use either co-receptor to infect cells. -

Impact of Using Organic Yeast in the Fermentation Process of Wine
processes Article Impact of Using Organic Yeast in the Fermentation Process of Wine Balázs Nagy 1, Zsuzsanna Varga 2,Réka Matolcsi 1, Nikolett Kellner 1 , Áron Szövényi 1 and Diána Nyitrainé Sárdy 1,* 1 Faculty of Horticultural Science Department of Oenology, Szent István University, 1118 Budapest, Hungary; [email protected] (B.N.); [email protected] (R.M.); [email protected] (N.K.); [email protected] (Á.S.) 2 Faculty of Horticultural Science Department of Viticulture, Szent István University, 1118 Budapest, Hungary; [email protected] * Correspondence: [email protected] Abstract: The aim of this study was to find out what kind of “Bianca” wine could be produced when using organic yeast, what are the dynamics of the resulting alcoholic fermentation, and whether this method is suitable for industrial production as well. Due to the stricter rules and regulations, as well as the limited amount and selection of the permitted chemicals, resistant, also known as interspecific or innovative grape varieties, can be the ideal basic materials of alternative cultivation technologies. Well-designed analytical and organoleptic results have to provide the scientific background of resistant varieties, as these cultivars and their environmentally friendly cultivation techniques could be the raw materials of the future. The role of the yeast in wine production is crucial. We fermented wines from the “Bianca” juice samples three times where model chemical solutions were applied. In our research, we aimed to find out how organic yeast influenced the biogenic amine formation of three important compounds: histamine, tyramine, and serotonin. The main results of this study showed that all the problematic values (e.g., histamine) were under the critical limit (1 g/L), although the organic samples resulted in a significantly higher level than the control wines. -

Firearms Seizures and Trafficking: a «Local» Phenomenon
Volume 1, Issue 1 Firearms Seizures and Trafficking: A «Local» Phenomenon NICHOLAS MARSH1 Abstract This article presents findings from the 2015 UN Office on Drugs and Crime (UNODC) Study on firearms trafficking, which was based upon information collected from 48 governments. It outlines the methodology and sources used in the UNODC Study, and discusses their strengths and limitations. The UNODC Study is then located within three wider bodies of research on firearms trafficking. Three key findings from data reported by the states that took part in the Study are summarized. In those states firearms trafficking is mostly small scale and local – occurring across neighbouring borders or within regions. Trafficked firearms tend to be obtained by people engaged in other forms of criminal activity. In many states there is a marked lack of capacity to collect and analyse data on firearms trafficking. These findings suggest the need to re-evaluate how firearms trafficking is often perceived. Keywords Firearms, small arms, illicit, trafficking, United Nations, arms trade Introduction The illicit trade2in firearms, also referred to as ‘small arms’ and often combined in policy processes with light weapons, and their parts and ammunition, has been a key area of international concern since the late 1990s. For example, in a 2015 resolution the United Nations Security Council notes that it is: 1Nicholas Marsh is a Research Fellow at the Peace Research Institute Oslo (PRIO) where he runs a database project that tracks the illicit and licensed trade in small arms and light weapons. He has been the Chair of a European research network on small arms, a Consultant to the UN Office on Drugs and Crime and to the SmallArms Survey, and is a founder member of the Small Arms Data Observatory. -

1. Summer Rain by Carl Thomas 2. Kiss Kiss by Chris Brown Feat T Pain 3
1. Summer Rain By Carl Thomas 2. Kiss Kiss By Chris Brown feat T Pain 3. You Know What's Up By Donell Jones 4. I Believe By Fantasia By Rhythm and Blues 5. Pyramids (Explicit) By Frank Ocean 6. Under The Sea By The Little Mermaid 7. Do What It Do By Jamie Foxx 8. Slow Jamz By Twista feat. Kanye West And Jamie Foxx 9. Calling All Hearts By DJ Cassidy Feat. Robin Thicke & Jessie J 10. I'd Really Love To See You Tonight By England Dan & John Ford Coley 11. I Wanna Be Loved By Eric Benet 12. Where Does The Love Go By Eric Benet with Yvonne Catterfeld 13. Freek'n You By Jodeci By Rhythm and Blues 14. If You Think You're Lonely Now By K-Ci Hailey Of Jodeci 15. All The Things (Your Man Don't Do) By Joe 16. All Or Nothing By JOE By Rhythm and Blues 17. Do It Like A Dude By Jessie J 18. Make You Sweat By Keith Sweat 19. Forever, For Always, For Love By Luther Vandros 20. The Glow Of Love By Luther Vandross 21. Nobody But You By Mary J. Blige 22. I'm Going Down By Mary J Blige 23. I Like By Montell Jordan Feat. Slick Rick 24. If You Don't Know Me By Now By Patti LaBelle 25. There's A Winner In You By Patti LaBelle 26. When A Woman's Fed Up By R. Kelly 27. I Like By Shanice 28. Hot Sugar - Tamar Braxton - Rhythm and Blues3005 (clean) by Childish Gambino 29. -

Review CCR5 Antagonists: Host-Targeted Antivirals for the Treatment of HIV Infection
Antiviral Chemistry & Chemotherapy 16:339–354 Review CCR5 antagonists: host-targeted antivirals for the treatment of HIV infection Mike Westby* and Elna van der Ryst Pfizer Global R&D, Kent, UK *Corresponding author: Tel: +44 1304 649876; Fax: +44 1304 651819; E-mail: [email protected] The human chemokine receptors, CCR5 and suggest that these compounds have a long plasma CXCR4, are potential host targets for exogenous, half-life and/or prolonged CCR5 occupancy, which small-molecule antagonists for the inhibition of may explain the delay in viral rebound observed HIV-1 infection. HIV-1 strains can be categorised by following compound withdrawal in short-term co-receptor tropism – their ability to utilise CCR5 monotherapy studies. A switch from CCR5 to (CCR5-tropic), CXCR4 (CXCR4-tropic) or both (dual- CXCR4 tropism occurs spontaneously in approxi- tropic) as a co-receptor for entry into susceptible mately 50% of HIV-infected patients and has been cells. CCR5 may be the more suitable co-receptor associated with, but is not required for, disease target for small-molecule antagonists because a progression. The possibility of a co-receptor natural deletion in the CCR5 gene preventing its tropism switch occurring under selection pressure expression on the cell surface is not associated by CCR5 antagonists is discussed. The completion with any obvious phenotype, but can confer of ongoing Phase IIb/III studies of maraviroc, resistance to infection by CCR5-tropic strains – the aplaviroc and vicriviroc will provide further insight most frequently sexually-transmitted strains. into co-receptor tropism, HIV pathogenesis and The current leading CCR5 antagonists in clinical the suitability of CCR5 antagonists as a potent development include maraviroc (UK-427,857, new class of antivirals for the treatment of HIV Pfizer), aplaviroc (873140, GlaxoSmithKline) and infection. -

Parliamentary Debates (Hansard)
Tuesday Volume 678 21 July 2020 No. 90 HOUSE OF COMMONS OFFICIAL REPORT PARLIAMENTARY DEBATES (HANSARD) Tuesday 21 July 2020 © Parliamentary Copyright House of Commons 2020 This publication may be reproduced under the terms of the Open Parliament licence, which is published at www.parliament.uk/site-information/copyright/. 1979 21 JULY 2020 1980 Ben Everitt: That is absolutely right, but it is not just House of Commons about bouncing back; it is also about levelling up. Will the Secretary of State join my hon. Friend the Universities Tuesday 21 July 2020 Minister in giving his backing in the spending review to the shovel-ready MK:U—a much needed technical The House met at half-past Eleven o’clock university in Milton Keynes which will deliver cutting-edge science, technology and engineering jobs and skills for local employers? PRAYERS Alok Sharma: As my hon. Friend would expect, the [MR SPEAKER ] in the Chair MK:U proposal will be judged objectively on its merits. Virtual participation in proceedings commenced (Order, More generally, I can confirm that the Government 4 June). recognise the significant potential of the Oxford-Cambridge [NB: [V] denotes a Member participating virtually.] arc and the important role of Milton Keynes in achieving that potential. Oral Answers to Questions Andy Carter: Airline pilots working for easyJet took an unprecedented decision on Friday to declare no confidence in their senior management. I have heard BUSINESS, ENERGY AND INDUSTRIAL from many constituents who work at the airline in STRATEGY Liverpool and Manchester who are worried about the company’s approach of “fire and rehire on different The Secretary of State was asked— terms”. -

Familial Mediterranean Fever
:: Familial Mediterranean fever – This document is a translation of the French recommendations drafted by Prof Gilles Grateau, Dr Véronique Hentgen, Dr Katia Stankovic Stojanovic and Dr Gilles Bagou reviewed and published by Orphanet in 2010. – Some of the procedures mentioned, particularly drug treatments, may not be validated in the country where you practice. Synonyms: Periodic disease, FMF Definition: Familial Mediterranean fever (FMF) is an auto-inflammatory disease of genetic origin, affecting Mediterranean populations and characterised by recurrent attacks of fever accompanied by polyserositis that causes the symptoms. Colchicine is the basic reference treatment and is designed to tackle inflammatory attacks and prevent amyloidosis, the most severe complication of FMF. Further information: See the Orphanet abstract http://www.orpha.net/data/patho/Pro/en/Emergency_FamilialMediterraneanFever-enPro920.pdf ©Orphanet UK 1/5 Pre-hospital emergency care recommendations Call for a patient suffering from Familial mediterranean fever Synonyms periodic disease FMF Mechanisms auto-inflammatory disease that affects Mediterranean populations in particular, due to mutation of the MEFV gene that codes pyrin or marenostrin, this being the underlying cause of congenital immune dysfunction; repeated inflammatory attacks can lead to amyloidosis, particularly renal Specific risks in emergency situations acute inflammatory attack, particularly abdominal (pseudo-surgical), but also thoracic, articular (knees) or testicular fever as an expression -

Whole Day Download the Hansard
Tuesday Volume 675 5 May 2020 No. 54 HOUSE OF COMMONS OFFICIAL REPORT PARLIAMENTARY DEBATES (HANSARD) Tuesday 5 May 2020 © Parliamentary Copyright House of Commons 2020 This publication may be reproduced under the terms of the Open Parliament licence, which is published at www.parliament.uk/site-information/copyright/. 475 5 MAY 2020 476 to provide devices and internet access to vulnerable children House of Commons and published a list of high-quality online educational resources, and we continue to support parents and Tuesday 5 May 2020 teachers in supporting children at home. Julian Sturdy [V]: Headteachers in York have told me The House met at half-past Eleven o’clock of their frustration that they will have to wait at least another month until they can provide students with laptops under the Government’s scheme. What assurances PRAYERS can my right hon. Friend give me that support will be available to schools in the meantime to help their most [MR SPEAKER in the Chair] disadvantaged students learn from home? The House entered into hybrid scrutiny proceedings (Order, 22 April). Gavin Williamson: As I am sure my hon. Friend will understand, £100 million for computers and other support [NB: [V] denotes a Member participating virtually.] for schools is a major investment, and it takes a while for these resources to arrive at schools. We have already notified multi-academy trusts and local authorities of Oral Answers to Questions what resources they will be getting, and we continue to work to provide resources,with the BBC providing resources in the homes of children right across the country.