Peroxisome Proliferator-Activated Receptors: Features, Functions, and Future
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Chemicals in the Fourth Report and Updated Tables Pdf Icon[PDF
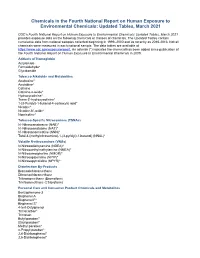
Chemicals in the Fourth National Report on Human Exposure to Environmental Chemicals: Updated Tables, March 2021 CDC’s Fourth National Report on Human Exposure to Environmental Chemicals: Updated Tables, March 2021 provides exposure data on the following chemicals or classes of chemicals. The Updated Tables contain cumulative data from national samples collected beginning in 1999–2000 and as recently as 2015-2016. Not all chemicals were measured in each national sample. The data tables are available at https://www.cdc.gov/exposurereport. An asterisk (*) indicates the chemical has been added since publication of the Fourth National Report on Human Exposure to Environmental Chemicals in 2009. Adducts of Hemoglobin Acrylamide Formaldehyde* Glycidamide Tobacco Alkaloids and Metabolites Anabasine* Anatabine* Cotinine Cotinine-n-oxide* Hydroxycotinine* Trans-3’-hydroxycotinine* 1-(3-Pyridyl)-1-butanol-4-carboxylic acid* Nicotine* Nicotine-N’-oxide* Nornicotine* Tobacco-Specific Nitrosamines (TSNAs) N’-Nitrosoanabasine (NAB)* N’-Nitrosoanatabine (NAT)* N’-Nitrosonornicotine (NNN)* Total 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol) (NNAL)* Volatile N-nitrosamines (VNAs) N-Nitrosodiethylamine (NDEA)* N-Nitrosoethylmethylamine (NMEA)* N-Nitrosomorpholine (NMOR)* N-Nitrosopiperidine (NPIP)* N-Nitrosopyrrolidine (NPYR)* Disinfection By-Products Bromodichloromethane Dibromochloromethane Tribromomethane (Bromoform) Trichloromethane (Chloroform) Personal Care and Consumer Product Chemicals and Metabolites Benzophenone-3 Bisphenol A Bisphenol F* Bisphenol -

Design Novel Dual Agonists for Treating Type-2 Diabetes by Targeting Peroxisome Proliferator-Activated Receptors with Core Hopping Approach
Design Novel Dual Agonists for Treating Type-2 Diabetes by Targeting Peroxisome Proliferator-Activated Receptors with Core Hopping Approach Ying Ma1., Shu-Qing Wang1,3*., Wei-Ren Xu2, Run-Ling Wang1*, Kuo-Chen Chou3 1 Tianjin Key Laboratory on Technologies Enabling Development of Clinical Therapeutics and Diagnostics (Theranostics), School of Pharmacy, Tianjin Medical University, Tianjin, China, 2 Tianjin Institute of Pharmaceutical Research (TIPR), Tianjin, China, 3 Gordon Life Science Institute, San Diego, California, United States of America Abstract Owing to their unique functions in regulating glucose, lipid and cholesterol metabolism, PPARs (peroxisome proliferator- activated receptors) have drawn special attention for developing drugs to treat type-2 diabetes. By combining the lipid benefit of PPAR-alpha agonists (such as fibrates) with the glycemic advantages of the PPAR-gamma agonists (such as thiazolidinediones), the dual PPAR agonists approach can both improve the metabolic effects and minimize the side effects caused by either agent alone, and hence has become a promising strategy for designing effective drugs against type-2 diabetes. In this study, by means of the powerful ‘‘core hopping’’ and ‘‘glide docking’’ techniques, a novel class of PPAR dual agonists was discovered based on the compound GW409544, a well-known dual agonist for both PPAR-alpha and PPAR- gamma modified from the farglitazar structure. It was observed by molecular dynamics simulations that these novel agonists not only possessed the same function as GW409544 did in activating PPAR-alpha and PPAR-gamma, but also had more favorable conformation for binding to the two receptors. It was further validated by the outcomes of their ADME (absorption, distribution, metabolism, and excretion) predictions that the new agonists hold high potential to become drug candidates. -

High-Mobility Group A1 Proteins May Be Involved in Estrogen Receptor Status of Breast Cancer
3786 Editorial Commentary High-mobility group A1 proteins may be involved in estrogen receptor status of breast cancer Yoshihiro Harada, Kenji Ohe Department of Pharmacotherapeutics, Faculty of Pharmaceutical Sciences, Fukuoka University, Jonan-ku, Fukuoka, Japan Correspondence to: Kenji Ohe. Department of Pharmacotherapeutics, Faculty of Pharmaceutical Sciences, Fukuoka University, Building 17, 8-19-1 Nanakuma, Jonan-ku, Fukuoka 814-180, Japan. Email: [email protected]. Provenance and Peer Review: This article was commissioned by the editorial office, Translational Cancer Research. The article did not undergo external peer review. Comment on: Gorbounov M, Carleton NM, Asch-Kendrick RJ, et al. High mobility group A1 (HMGA1) protein and gene expression correlate with ER-negativity and poor outcomes in breast cancer. Breast Cancer Res Treat 2020;179:25-35. Submitted Apr 27, 2020. Accepted for publication May 13, 2020. doi: 10.21037/tcr-20-1921 View this article at: http://dx.doi.org/10.21037/tcr-20-1921 The three types of breast cancer HMGA1 proteins: old and new proteins in breast cancer Breast cancer is one of the most common of cancers in woman. About 316,700 new cases were diagnosed as breast HMGA1 (previously called HMGI/Y) is a member of the cancer in US woman in 2019 and 41,760 were predicted to high-mobility group (HMG) proteins that were found from die from it (1). Breast cancer has a characteristic of therapy- their high mobility characteristics during polyacrylamide targeting receptors: hormone receptors (HR) that are electrophoresis of non-histone chromatin-associated estrogen receptor [ER: human ERα protein (NCBI protein proteins (3). -

Pfoa) Or Perfluorooctane Sulfonate (Pfos
National Toxicology Program NTP U.S. Department of Health and Human Services NTP Monograph Immunotoxicity Associated with Exposure to Perfluorooctanoic Acid or Perfluorooctane Sulfonate September 2016 NTP MONOGRAPH ON IMMUNOTOXICITY ASSOCIATED WITH EXPOSURE TO PERFLUOROOCTANOIC ACID (PFOA) OR PERFLUOROOCTANE SULFONATE (PFOS) September, 2016 Office of Health Assessment and Translation Division of the National Toxicology Program National Institute of Environmental Health Sciences National Institutes of Health U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Systematic Review of Immunotoxicity Associated with Exposure to PFOA or PFOS TABLE OF CONTENTS Table of Contents ...............................................................................................................................II List of Table and Figures ................................................................................................................... IV Abstract ............................................................................................................................................. 1 Peer Review Of The Draft NTP Monograph ......................................................................................... 2 Peer-Review Panel .............................................................................................................................. 2 Introduction ...................................................................................................................................... 3 Objective and Specific Aims ............................................................................................................... -

PFAS MCL Technical Support Document
ATTACHMENT 1 New Hampshire Department of Environmental Services Technical Background Report for the June 2019 Proposed Maximum Contaminant Levels (MCLs) and Ambient Groundwater Quality Standards (AGQSs) for Perfluorooctane sulfonic Acid (PFOS), Perfluorooctanoic Acid (PFOA), Perfluorononanoic Acid (PFNA), and Perfluorohexane sulfonic Acid (PFHxS) And Letter from Dr. Stephen M. Roberts, Ph.D. dated 6/25/2019 – Findings of Peer Review Conducted on Technical Background Report June 28, 2019 New Hampshire Department of Environmental Services Technical Background Report for the June 2019 Proposed Maximum Contaminant Levels (MCLs) and Ambient Groundwater Quality Standards (AGQSs) for Perfluorooctane sulfonic Acid (PFOS), Perfluorooctanoic Acid (PFOA), Perfluorononanoic Acid (PFNA), and Perfluorohexane sulfonic Acid (PFHxS) June 28, 2019 Table of Contents Abbreviations ................................................................................................................................................. i Acknowledgements ...................................................................................................................................... iii Section I. Executive Summary ....................................................................................................................... 1 Section II. Introduction ................................................................................................................................. 2 Section III. Reference Dose Derivation ........................................................................................................ -

Us 2018 / 0296525 A1
UN US 20180296525A1 ( 19) United States (12 ) Patent Application Publication (10 ) Pub. No. : US 2018/ 0296525 A1 ROIZMAN et al. ( 43 ) Pub . Date: Oct. 18 , 2018 ( 54 ) TREATMENT OF AGE - RELATED MACULAR A61K 38 /1709 ( 2013 .01 ) ; A61K 38 / 1866 DEGENERATION AND OTHER EYE (2013 . 01 ) ; A61K 31/ 40 ( 2013 .01 ) DISEASES WITH ONE OR MORE THERAPEUTIC AGENTS (71 ) Applicant: MacRegen , Inc ., San Jose , CA (US ) (57 ) ABSTRACT ( 72 ) Inventors : Keith ROIZMAN , San Jose , CA (US ) ; The present disclosure provides therapeutic agents for the Martin RUDOLF , Luebeck (DE ) treatment of age - related macular degeneration ( AMD ) and other eye disorders. One or more therapeutic agents can be (21 ) Appl. No .: 15 /910 , 992 used to treat any stages ( including the early , intermediate ( 22 ) Filed : Mar. 2 , 2018 and advance stages ) of AMD , and any phenotypes of AMD , including geographic atrophy ( including non -central GA and Related U . S . Application Data central GA ) and neovascularization ( including types 1 , 2 and 3 NV ) . In certain embodiments , an anti - dyslipidemic agent ( 60 ) Provisional application No . 62/ 467 ,073 , filed on Mar . ( e . g . , an apolipoprotein mimetic and / or a statin ) is used 3 , 2017 . alone to treat or slow the progression of atrophic AMD Publication Classification ( including early AMD and intermediate AMD ) , and / or to (51 ) Int. CI. prevent or delay the onset of AMD , advanced AMD and /or A61K 31/ 366 ( 2006 . 01 ) neovascular AMD . In further embodiments , two or more A61P 27 /02 ( 2006 .01 ) therapeutic agents ( e . g ., any combinations of an anti - dys A61K 9 / 00 ( 2006 . 01 ) lipidemic agent, an antioxidant, an anti- inflammatory agent, A61K 31 / 40 ( 2006 .01 ) a complement inhibitor, a neuroprotector and an anti - angio A61K 45 / 06 ( 2006 .01 ) genic agent ) that target multiple underlying factors of AMD A61K 38 / 17 ( 2006 .01 ) ( e . -

An Ontogenetic Switch Drives the Positive and Negative Selection of B Cells
An ontogenetic switch drives the positive and negative selection of B cells Xijin Xua, Mukta Deobagkar-Lelea, Katherine R. Bulla, Tanya L. Crockforda, Adam J. Meadb, Adam P. Cribbsc, David Simsc, Consuelo Anzilottia, and Richard J. Cornalla,1 aMedical Research Council Human Immunology Unit, Weatherall Institute of Molecular Medicine, University of Oxford, OX3 9DS Oxford, United Kingdom; bMedical Research Council Molecular Haematology Unit, Weatherall Institute of Molecular Medicine, University of Oxford, OX3 9DS Oxford, United Kingdom; and cMedical Research Council, Weatherall Institute of Molecular Medicine, Centre for Computational Biology, Weatherall Institute of Molecular Medicine, University of Oxford, OX3 9DS Oxford, United Kingdom Edited by Michael Reth, University of Freiburg, Freiburg, Germany, and approved January 6, 2020 (received for review September 3, 2019) + Developing B cells can be positively or negatively selected by self- BM HSCs increased CD5 B-1a B cell development (15), while antigens, but the mechanisms that determine these outcomes are expression of let-7b in FL pro-B cells blocked the development of incompletely understood. Here, we show that a B cell intrinsic B-1 B cells (17). These findings support the notion of hard-wired switch between positive and negative selection during ontogeny differences during ontogeny, but possibly downstream of the HSC is determined by a change from Lin28b to let-7 gene expression. commitment stage. Ectopic expression of a Lin28b transgene in murine B cells restored Several lines of evidence also suggest that B-1 B cells can un- the positive selection of autoreactive B-1 B cells by self-antigen in dergo positive selection, which is linked to their B cell receptor adult bone marrow. -

Health Effects Support Document for Perfluorooctanoic Acid (PFOA)
United States Office of Water EPA 822-R-16-003 Environmental Protection Mail Code 4304T May 2016 Agency Health Effects Support Document for Perfluorooctanoic Acid (PFOA) Perfluorooctanoic Acid – May 2016 i Health Effects Support Document for Perfluorooctanoic Acid (PFOA) U.S. Environmental Protection Agency Office of Water (4304T) Health and Ecological Criteria Division Washington, DC 20460 EPA Document Number: 822-R-16-003 May 2016 Perfluorooctanoic Acid – May 2016 ii BACKGROUND The Safe Drinking Water Act (SDWA), as amended in 1996, requires the Administrator of the U.S. Environmental Protection Agency (EPA) to periodically publish a list of unregulated chemical contaminants known or anticipated to occur in public water systems and that may require regulation under SDWA. The SDWA also requires the Agency to make regulatory determinations on at least five contaminants on the Contaminant Candidate List (CCL) every 5 years. For each contaminant on the CCL, before EPA makes a regulatory determination, the Agency needs to obtain sufficient data to conduct analyses on the extent to which the contaminant occurs and the risk it poses to populations via drinking water. Ultimately, this information will assist the Agency in determining the most appropriate course of action in relation to the contaminant (e.g., developing a regulation to control it in drinking water, developing guidance, or deciding not to regulate it). The PFOA health assessment was initiated by the Office of Water, Office of Science and Technology in 2009. The draft Health Effects Support Document for Perfluoroctanoic Acid (PFOA) was completed in 2013 and released for public comment in February 2014. -

HMGA2 Promotes Adipogenesis by Activating C/EBP&Beta
CORE Metadata, citation and similar papers at core.ac.uk Provided by Elsevier - Publisher Connector Biochemical and Biophysical Research Communications 472 (2016) 617e623 Contents lists available at ScienceDirect Biochemical and Biophysical Research Communications journal homepage: www.elsevier.com/locate/ybbrc HMGA2 promotes adipogenesis by activating C/EBPb-mediated expression of PPARg * Yang Xi a, Wanjing Shen a, Lili Ma a, Ming Zhao a, Jiachen Zheng a, Shizhong Bu a, , ** Shinjiro Hino b, Mitsuyoshi Nakao b, c, a Diabetes Center, and Zhejiang Provincial Key Laboratory of Pathophysiology, Institute of Biochemistry and Molecular Biology, School of Medicine, Ningbo University, Ningbo 315211, China b Department of Medical Cell Biology, Institute of Molecular Embryology and Genetics, Kumamoto University, Kumamoto, 860-0811, Japan c Core Research for Evolutional Science and Technology (CREST), Japan Agency for Medical Research and Development, Tokyo, Japan article info abstract Article history: Adipogenesis is orchestrated by a highly ordered network of transcription factors including peroxisome- Received 1 March 2016 proliferator activated receptor-gamma (PPARg) and CCAAT-enhancer binding protein (C/EBP) family Accepted 6 March 2016 proteins. High mobility group protein AT-hook 2 (HMGA2), an architectural transcription factor, has been Available online 8 March 2016 reported to play an essential role in preadipocyte proliferation, and its overexpression has been impli- cated in obesity in mice and humans. However, the direct role of HMGA2 in regulating the gene Keywords: expression program during adipogenesis is not known. Here, we demonstrate that HMGA2 is required for Adipogenesis C/EBPb-mediated expression of PPARg, and thus promotes adipogenic differentiation. We observed a HMGA2 C/EBPb transient but marked increase of Hmga2 transcript at an early phase of differentiation of mouse 3T3-L1 PPARg preadipocytes. -

The Opportunities and Challenges of Peroxisome Proliferator-Activated Receptors Ligands in Clinical Drug Discovery and Development
International Journal of Molecular Sciences Review The Opportunities and Challenges of Peroxisome Proliferator-Activated Receptors Ligands in Clinical Drug Discovery and Development Fan Hong 1,2, Pengfei Xu 1,*,† and Yonggong Zhai 1,2,* 1 Beijing Key Laboratory of Gene Resource and Molecular Development, College of Life Sciences, Beijing Normal University, Beijing 100875, China; [email protected] 2 Key Laboratory for Cell Proliferation and Regulation Biology of State Education Ministry, College of Life Sciences, Beijing Normal University, Beijing 100875, China * Correspondence: [email protected] (P.X.); [email protected] (Y.Z.); Tel.: +86-156-005-60991 (P.X.); +86-10-5880-6656 (Y.Z.) † Current address: Center for Pharmacogenetics and Department of Pharmaceutical Sciences, University of Pittsburgh, Pittsburgh, PA 15213, USA. Received: 22 June 2018; Accepted: 24 July 2018; Published: 27 July 2018 Abstract: Peroxisome proliferator-activated receptors (PPARs) are a well-known pharmacological target for the treatment of multiple diseases, including diabetes mellitus, dyslipidemia, cardiovascular diseases and even primary biliary cholangitis, gout, cancer, Alzheimer’s disease and ulcerative colitis. The three PPAR isoforms (α, β/δ and γ) have emerged as integrators of glucose and lipid metabolic signaling networks. Typically, PPARα is activated by fibrates, which are commonly used therapeutic agents in the treatment of dyslipidemia. The pharmacological activators of PPARγ include thiazolidinediones (TZDs), which are insulin sensitizers used in the treatment of type 2 diabetes mellitus (T2DM), despite some drawbacks. In this review, we summarize 84 types of PPAR synthetic ligands introduced to date for the treatment of metabolic and other diseases and provide a comprehensive analysis of the current applications and problems of these ligands in clinical drug discovery and development. -

The Expression of HMGA Genes Is Regulated by Their 3Оutr
Oncogene (2001) 20, 4537 ± 4541 ã 2001 Nature Publishing Group All rights reserved 0950 ± 9232/01 $15.00 www.nature.com/onc The expression of HMGA genes is regulated by their 3'UTR Lars Borrmann1, S Wilkening1 and J Bullerdiek*,1 1Center for Human Genetics, University of Bremen, Leobenerstr. ZHG, 28359 Bremen, Germany Many benign mesenchymal tumors are characterized by binding by HMGA proteins leads to a conformational chromosomal abnormalities of the regions 12q15 or change in DNA modulating the environment for the 6p21.3 leading to aberrant expression of either HMGA2 binding of transcription factors. (formerly HMGIC) or HMGA1 (formerly HMGIY). Whereas HMGA2 is almost exclusively expressed in The proteins of both genes belong to the HMGA proliferating undierentiated cells during embryogen- (formerly HMGI(Y)) family of architectural transcrip- esis and in benign and malignant tumors, HMGA1 can tion factors. As a rule, aberrant HMGA transcripts also be detected at very low levels in dierentiated cells found in a variety of benign tumors have intact coding (Chiappetta et al., 1996; Zhou et al., 1995; Busse- regions at least for the DNA binding domains with a makers et al., 1991; Abe et al., 2000). An increased truncation of their 3' untranslated regions. Adding this to HMGA1 gene expression has been considered as a the ®nding that an altered HMGA protein level is not general diagnostic marker for neoplastic transforma- always correlated with an increased amount of corre- tion (Goodwin et al., 1985; Giancotti et al., 1987, 1989) sponding mRNA indicates a posttranscriptional expres- and the metastatic potential of malignant neoplasms sion control mediated by regulatory elements within the (Bussemakers et al., 1991; Tamimi et al., 1993; 3'UTR. -

Integrative and Systemic Approaches for Evaluating Pparβ/Δ (PPARD)
Integrative and systemic approaches for evaluating PPAR β/δ (PPARD) function Greta MP Giordano Attianese and Béatrice Desvergne Center for Integrative Genomics, University of Lausanne, Switzerland Footnotes: Corresponding author, BD: [email protected] Competing interests: The authors declare no competing financial interests Author contributions: Both authors have been involved in drafting the manuscript and revising it critically. Received December 5, 2014; Accepted March 9, 2015; Published April 27, 2015 Copyright © 2015 Giordano Attianese and Desvergne. This is an open-access article distributed under the terms of the Creative Commons Non-Commercial Attribution License, which permits unrestricted non-commercial use distribution and reproduction in any medium, provided the original work is properly cited. Abbreviations: αMyHC, α-Myosin Heavy Chain; BCL6, B-cell lymphoma 6 protein; BAT, Brown adipose tissue; ChIP, Chromatin Immunoprecipitation; CHD, Coronary heart disease; DBD, DNA-binding domain; FAO, Fatty Acid Oxidation; FA, Fatty Acid; GSIS, Glucose-stimulated insulin secretion; HSC, Hematopoietic Stem cells; H&E, Hematoxylin and Eosin; HDAC1, Histone deacetylase 1; LBD, Ligand binding domain; MCP1, Monocyte chemotactic protein 1; NFkB, Nuclear factor kappa-light-chain- enhancer of activated B cells; NR, Nuclear Receptor; NCoR1, Nuclear receptor co-repressor 1; PPARs, Peroxisome proliferator- activated receptors; PPRE, PPAR-responsive element; RER, Respiratory Exchange Ratio; RA, Retinoic Acid; RXR, Retinoid X receptor; SMRT, Silencing mediator of retinoic acid and thyroid hormone receptors; SNPs, Single Nucleotide Polymorphisms; SUMO, Small Ubiquitin-like Modifier; TZDs, Thiazolidinediones; TR, Thyroid hormone receptor; TG, Triglycerides; VLDL, Very large density lipoprotein; WOSCOPS, West of Scotland Coronary Prevention Study; WAT, White adipose tissue. Citation: Giordano Attianese G and Desvergne B (2015) Integrative and systemic approaches for evaluating PPAR β/δ (PPARD) function.