Human Artificial Oocytes from Patients' Somatic Cells: Past, Present and Future
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Reproduction Methods
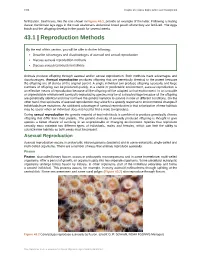
1336 Chapter 43 | Animal Reproduction and Development fertilization. Seahorses, like the one shown in Figure 43.1, provide an example of the latter. Following a mating dance, the female lays eggs in the male seahorse’s abdominal brood pouch where they are fertilized. The eggs hatch and the offspring develop in the pouch for several weeks. 43.1 | Reproduction Methods By the end of this section, you will be able to do the following: • Describe advantages and disadvantages of asexual and sexual reproduction • Discuss asexual reproduction methods • Discuss sexual reproduction methods Animals produce offspring through asexual and/or sexual reproduction. Both methods have advantages and disadvantages. Asexual reproduction produces offspring that are genetically identical to the parent because the offspring are all clones of the original parent. A single individual can produce offspring asexually and large numbers of offspring can be produced quickly. In a stable or predictable environment, asexual reproduction is an effective means of reproduction because all the offspring will be adapted to that environment. In an unstable or unpredictable environment asexually-reproducing species may be at a disadvantage because all the offspring are genetically identical and may not have the genetic variation to survive in new or different conditions. On the other hand, the rapid rates of asexual reproduction may allow for a speedy response to environmental changes if individuals have mutations. An additional advantage of asexual reproduction is that colonization of new habitats may be easier when an individual does not need to find a mate to reproduce. During sexual reproduction the genetic material of two individuals is combined to produce genetically diverse offspring that differ from their parents. -
![Oogenesis [PDF]](https://docslib.b-cdn.net/cover/2902/oogenesis-pdf-452902.webp)
Oogenesis [PDF]
Oogenesis Dr Navneet Kumar Professor (Anatomy) K.G.M.U Dr NavneetKumar Professor Anatomy KGMU Lko Oogenesis • Development of ovum (oogenesis) • Maturation of follicle • Fate of ovum and follicle Dr NavneetKumar Professor Anatomy KGMU Lko Dr NavneetKumar Professor Anatomy KGMU Lko Oogenesis • Site – ovary • Duration – 7th week of embryo –primordial germ cells • -3rd month of fetus –oogonium • - two million primary oocyte • -7th month of fetus primary oocyte +primary follicle • - at birth primary oocyte with prophase of • 1st meiotic division • - 40 thousand primary oocyte in adult ovary • - 500 primary oocyte attain maturity • - oogenesis completed after fertilization Dr Navneet Kumar Dr NavneetKumar Professor Professor (Anatomy) Anatomy KGMU Lko K.G.M.U Development of ovum Oogonium(44XX) -In fetal ovary Primary oocyte (44XX) arrest till puberty in prophase of 1st phase meiotic division Secondary oocyte(22X)+Polar body(22X) 1st phase meiotic division completed at ovulation &enter in 2nd phase Ovum(22X)+polarbody(22X) After fertilization Dr NavneetKumar Professor Anatomy KGMU Lko Dr NavneetKumar Professor Anatomy KGMU Lko Dr Navneet Kumar Dr ProfessorNavneetKumar (Anatomy) Professor K.G.M.UAnatomy KGMU Lko Dr NavneetKumar Professor Anatomy KGMU Lko Maturation of follicle Dr NavneetKumar Professor Anatomy KGMU Lko Maturation of follicle Primordial follicle -Follicular cells Primary follicle -Zona pallucida -Granulosa cells Secondary follicle Antrum developed Ovarian /Graafian follicle - Theca interna &externa -Membrana granulosa -Antrial -
Chapter 38: Reproduction and Development Computer Test Bank Cryopreservation
Chapter 38 Organizer Reproduction and Development Refer to pages 4T-5T of the Teacher Guide for an explanation of the National Science Education Standards correlations. Teacher Classroom Resources Activities/FeaturesObjectivesSection MastersSection TransparenciesReproducible Reinforcement and Study Guide, pp. 167-168 L2 Section Focus Transparency 93 L1 ELL Section 38.1 1. Identify the parts of the male and Inside Story: Sex Cell Production, p. 1033 Section 38.1 female reproductive systems. Problem-Solving Lab 38-1, p. 1035 Concept Mapping, p. 38 L3 ELL Basic Concepts Transparency 74 L2 ELL Human Reproductive 2. Summarize the negative feedback Human Critical Thinking/Problem Solving, p. 38 L3 Basic Concepts Transparency 75 L2 ELL Systems control of reproductive hormones. Reproductive Content Mastery, pp. 185-186, 188 L1 Reteaching Skills Transparency 55 L1P ELL National Science Education 3. Sequence the stages of the menstrual Systems P P cycle. Standards UCP.1-3, UCP.5; P C.1, C.5; F.1 (2 sessions, 11/ P 2 Reinforcement and Study Guide, p. 169 L2 P Section Focus Transparency 94 L1 ELLP blocks) Section 38.2 P LS BioLab and MiniLab Worksheets, pp. 169-170 L2 Reteaching Skills Transparency 56a,P 56b L1 LS P LS Development Laboratory Manual, pp. 277-284 L2 ELL P Before Birth LS Section 38.2 4. Summarize the events during each MiniLab 38-1: Examining Sperm and Egg Content Mastery, pp. 185,LS 187-188 L1 LS P LS trimester of pregnancy. Attraction, p. 1038 LS Development Before MiniLab 38-2: Making a Graph of Fetal Size, P LS P Reinforcement and Study Guide, p. -
The Reproductive System
PowerPoint® Lecture Slides prepared by Meg Flemming Austin Community College C H A P T E R 19 The Reproductive System © 2013 Pearson Education, Inc. Chapter 19 Learning Outcomes • 19-1 • List the basic components of the human reproductive system, and summarize the functions of each. • 19-2 • Describe the components of the male reproductive system; list the roles of the reproductive tract and accessory glands in producing spermatozoa; describe the composition of semen; and summarize the hormonal mechanisms that regulate male reproductive function. • 19-3 • Describe the components of the female reproductive system; explain the process of oogenesis in the ovary; discuss the ovarian and uterine cycles; and summarize the events of the female reproductive cycle. © 2013 Pearson Education, Inc. Chapter 19 Learning Outcomes • 19-4 • Discuss the physiology of sexual intercourse in males and females. • 19-5 • Describe the age-related changes that occur in the reproductive system. • 19-6 • Give examples of interactions between the reproductive system and each of the other organ systems. © 2013 Pearson Education, Inc. Basic Reproductive Structures (19-1) • Gonads • Testes in males • Ovaries in females • Ducts • Accessory glands • External genitalia © 2013 Pearson Education, Inc. Gametes (19-1) • Reproductive cells • Spermatozoa (or sperm) in males • Combine with secretions of accessory glands to form semen • Oocyte in females • An immature gamete • When fertilized by sperm becomes an ovum © 2013 Pearson Education, Inc. Checkpoint (19-1) 1. Define gamete. 2. List the basic components of the reproductive system. 3. Define gonads. © 2013 Pearson Education, Inc. The Scrotum (19-2) • Location of primary male sex organs, the testes • Hang outside of pelvic cavity • Contains two chambers, the scrotal cavities • Wall • Dartos, a thin smooth muscle layer, wrinkles the scrotal surface • Cremaster muscle, a skeletal muscle, pulls testes closer to body to ensure proper temperature for sperm © 2013 Pearson Education, Inc. -

N Wa Brahma/Atman
NÜ Wa God Brahma/Atman HUMANHUMAN EMBRYOLOGYEMBRYOLOGY Department of Histology and Embryology Jilin University ChapterChapter 11 IntroductionIntroduction toto HumanHuman EmbryologyEmbryology 1.1. WhatWhat isis EmbryologyEmbryology?? ontogenesis ovumovum Zygote/fertilizedZygote/fertilized ovumovum spermsperm NineNine monthsmonths (266(266 daysdays oror 3838 weeksweeks toto bebe exact)exact) inin thethe uterusuterus InfantInfant fetusfetus 1.1. WhatWhat isis EmbryologyEmbryology?? Traditional /descriptive embryology focuses on understanding the basic structural pattern of the embryonic body. Teratology is concerned with the reasons, mechanisms and protective measures of malformations. Comparative embryology seeks several general rules by comparison the identities or the differences among the development of many species. Experimental embryology researches on the causative factors in development by posing hypotheses and testing them with different experimental techniques. Chemical embryology researches on the changes of some chemical materials in cells or tissues and the chemical basis of morphogenesis during the development . Molecular embryology focuses on the molecular mechanisms of morphogenesis, and the gene regulation of embryonic development. Reproductive biology emphases on normal gametogenesis, endocrinology of reproduction, transport of gametes and fertilization, early embryonic development, and implantation of the mammalian embryo, in addition to more practically oriented problems involving techniques of fertilization and -

The Human Reproductive System
ANATOMY- PHYSIOLOGY-REPRODUCTIVE SYSTEM - IN RESPONSE TO CONVID 19 APRIL 2, 2020 nd Dear students and parents, April 2 , 2020 Beginning two days prior to our last day at school I issued work packets to all students in all classed; the content of which was spanning a two-three week period. Now that our removal from school will continue to at least May 1st, I have provided the following work packets which will span the remainder of the year, should our crisis continue. The following folders are available: ANATOMY – PHYSIOLOGY 1. Packet – THE HUMAN REPRODUCATIVE AND ENDOCRINE SYSTEMS. 2. Packet- THE HUMAN NERVOUS SYSTEM 3. Packet handed our prior to our last day: THE HUMAN EXCRETORY SYSTEM ZOOLOGY 1. Packet- STUDY OF THE CRUSTACEANS 2. Packet- STUDY OF THE INSECTS 3. Packet- handed our prior to our last day- INTRODUCTION TO THE ARTRHROPODS- CLASSES MYRIAPODA AND ARACHNIDA AP BIOLOGY – as per the newly devised topics of study focus, structure of adapted test, test dates and supports provided as per the guidelines and policies of The College Board TO ALL STUDENTS! THESE PACKETS WILL BE GUIDED BY THE SAME PROCEDURES WE EMBRACED DURING FALL TECH WEEK WHERE YOU ARE RESPONSIBLE FOR THE WORK IN THE PACKETS- DELIVERED UPON YOUR RETURN TO SCHOOL OR AS PER UNFORESEEN CHANGES WHICH COME OUR WAY. COLLABORATION IS ENCOURAGED- SO STAY IN TOUCH AND DIG IN! YOUR PACKETS WILL BE A NOTEBOOK GRADE. EVENTUALLY YOU SHALL TAKE AN INDIVIDUAL TEST OF EACH PACKET = AN EXAM GRADE! SCHOOL IS OFF SITE BUT NOT SHUT DOWN SO PLEASE DO THE BODY OF WORK ASSIGNED IN THE PACKETS PROVIDED. -

Downloaded from Bioscientifica.Com at 10/06/2021 01:35:11PM Via Free Access 230
EFFECT OF BUSULPHAN ON THE DEVELOPING OVARY IN THE RAT B. N. HEMSWORTH and H. JACKSON Experimental Chemotherapy, Paterson Laboratories, Christie Hospital, Manchester 20 (Received 8th February 1963) Summary. Female rats were exposed to Busulphan on selected days between the 5th day of foetal life and Day 15 post partum, inclusive. The drug apparently had no effect on the foetal sex cells when admini- stered to the pregnant female between Days 5 and 7 post coitum. Later in pregnancy a destructive action became rapidly more powerful. So far as the developing ovary is concerned it would seem that the action of Busulphan at this dose level, i.e. 10 mg/kg intraperitoneally, is confined to the precursor of the oocyte, namely the oogonium and that when these cells enter meiotic prophase on about the 17th day of foetal life there is a marked decrease in their sensitivity to the action of the drug. The effect of the treatment on fertility has also been studied. INTRODUCTION The effect of Busulphan on the foetal ovary was described by Bollag (1954). He reported that a single dose given to pregnant rats 5 to 7 days ante partum resulted in sterility in the offspring. Later, Galton & Till (1956) stated that "earlier in pregnancy quite large doses do not interfere with its course and the F1 and F2 generations were apparently healthy". In view of these studies, it was decided to investigate the sensitivity of the proliferating cell systems of the gonad during development. A preliminary report of these investigations has been published elsewhere (Hemsworth & Jackson, 1962a). -

Physiology of Reproduction: Gametogenesis and the Female Cycles
ighapmLre43pg317_320 5/12/04 3:35 PM Page 317 impos03 302:bjighapmL:ighapmLrevshts:layouts: NAME ___________________________________ LAB TIME/DATE _______________________ REVIEW SHEET Physiology of Reproduction: exercise Gametogenesis and the Female Cycles 43 Meiosis 1. The following statements refer to events occurring during mitosis and/or meiosis. For each statement, decide if the event oc- curs in (a) mitosis only, (b) meiosis only, or (c) both mitosis and meiosis. c 1. dyads are visible b 2. tetrads are visible a 3. product is two diploid daughter cells b 4. product is four haploid daughter cells c 5. involves the phases prophase, metaphase, anaphase, and telophase a 6. occurs throughout the body b 7. occurs only in the ovaries and testes a 8. provides cells for growth and repair b 9. homologues synapse and chiasmata are seen b 10. daughter cells are quantitatively and qualitatively different from the mother cell a 11. daughter cells are genetically identical to the mother cell c 12. chromosomes are replicated before the division process begins b 13. provides cells for replication of the species b 14. consists of two consecutive nuclear divisions, without chromosomal replication occurring before the second division 2. Describe the process of synapsis. The homologous chromosomes become closely aligned along their entire length. 3. How does crossover introduce variability in the daughter cells? Where crossovers occur, chromosome breakage occurs and parts are exchanged. This results in chromosomes with different parental contributions. 4. Define homologous chromosomes. Chromosomes that carry genes for the same traits. (One ϭ paternal chromosome, the other maternal chromosome.) Review Sheet 43 317 ighapmLre43pg317_320 5/14/04 11:53 AM Page 318 impos06 302:bjighapmL:ighapmLrevshts:layouts: Spermatogenesis 5. -
The Reproductive System in Perspective
Essentials of Anatomy & Physiology, 4th Edition Martini / Bartholomew The Reproductive 19 System PowerPoint® Lecture Outlines prepared by Alan Magid, Duke University Slides 1 to 84 Copyright © 2007 Pearson Education, Inc., publishing as Benjamin Cummings Overview of Reproduction Reproductive System Essentials • Gonads (reproductive organs) • Testes in males, ovaries in females • Gametes (reproductive cells) • Spermatazoa (sperm) in males, • Ova (eggs) in females • Fertilization • Fusion of male and female gamete • Zygote • Fertilized egg Copyright © 2007 Pearson Education, Inc., publishing as Benjamin Cummings Male Reproductive System Reproductive Organs • Testes • Enclosed by scrotum • Produce spermatazoa (sperm) • Epididymis • Stores sperm • Ductus deferens (vas deferens) • Conducts sperm outward Copyright © 2007 Pearson Education, Inc., publishing as Benjamin Cummings Male Reproductive System Reproductive Organs (cont’d) • Ejaculatory duct • Accessory organs 1. Seminal vesicle 2. Prostate gland 3. Bulbourethral glands • Urethra • Inside the penis, an erectile organ Copyright © 2007 Pearson Education, Inc., publishing as Benjamin Cummings Male Reproductive System The Male Reproductive System Figure 19-1 Male Reproductive System The Testes • Primary sex organ in males • Hang within scrotum • Cremaster muscle lifts testis toward body • Tunica albuginea encloses testis Copyright © 2007 Pearson Education, Inc., publishing as Benjamin Cummings Male Reproductive System The Testes (cont’d) • Septa divide testis into lobules • Seminferous tubules -

Developmental Biology B.Sc. Biotechnology 4Th Semester (Generic Elective) Unit-I Gametogenesis and Fertilization Unit-I Reference Notes
INDIRA GANDHI NATIONAL TRIBAL UNIVERSITY AMARKANTAK, M.P. 484886 SUBJECT- Biotechnology TITLE- Developmental Biology B.Sc. Biotechnology 4th Semester (Generic Elective) Unit-I Gametogenesis and Fertilization Unit-I Reference Notes Dr. Parikipandla Sridevi Assistant Professor Dept. of Biotechnology Faculty of Science Indira Gandhi National Tribal University Amarkantak, MP, India Pin: 484887 Mob No: +919630036673, +919407331673 Email Id: [email protected], [email protected] [email protected] Unit I Definition, scope & historical perspective of development Biology, Gametogenesis – Spermatogenesis, Oogenesis Fertilization - Definition, mechanism, types of fertilization. Different types of eggs on the basis of yolk. CONTENTS 1. Introduction & history of development biology 2. Gametogenesis- spermatogenesis & oogenesis 3. Fertilization and types of fertilization 4. Type of eggs 1. Introduction & history of development biology 1.1. Introduction Developmental biology is the study of the process by which animals and plants grow and develop. Developmental biology also encompasses the biology of regeneration, asexual reproduction, metamorphosis, and the growth and differentiation of stem cells in the adult organism. 1.2. The Foundations of Developmental Biology What is developmental biology, and why has it emerged as one of the most dynamic and exciting areas of biological investigation? Nothing in nature is more fascinating than the development of a complex, multicellular organism that progressively acquires the essential attributes of its parents. Developmental biologists study all aspects of development, from the genes and molecular events that control development to the structural changes that an organism undergoes as it develops. They study various modes of development, from embryonic development of animals and plants to aggregation of slime mold amebae, flowering of plants or regeneration of limbs in salamanders. -

Twinning and Recombination: a Review of the Data Francis P
The Linacre Quarterly Volume 48 | Number 1 Article 9 February 1981 Twinning and Recombination: A Review of the Data Francis P. Filice Follow this and additional works at: http://epublications.marquette.edu/lnq Recommended Citation Filice, Francis P. (1981) "Twinning and Recombination: A Review of the Data," The Linacre Quarterly: Vol. 48: No. 1, Article 9. Available at: http://epublications.marquette.edu/lnq/vol48/iss1/9 Twinning and Recombination: A Review of the Data 1 Francis P. Filice Father Filice, who is affiliated with the department of biology at the University of San Francisco, gave this address at the 1978 NFCPG annual meeting. A. INTRODUCTION A number of authors have raised the possibility that the ease with which twinning can take place in humans during the first week after fertilization might offer data that would allow the theologian to argue that the conceptus, during that period, is really not yet a human indi vidual. 2 As supportive evidence, the apparent existence of individuals whose genetic structure suggests the fusion of two distinct twins has been offered as indicating how little "hominization" is present at this stage. In this paper I would like to review the pertinent portions of devel opment during the period of fertilization, cleavage, and implantation in humans; then I would like to review what is known of twinning and discuss our present knowledge about recombinant humans. B. FERTILIZATION AND EARLY DEVELOPMENT As the graffian follicle enlarges in the ovary, the oogonium under goes the first meiotic division. One set of chromosomes is gathered into the diploid first polar body, which then can be seen as a small bit of protoplasm lying next to the ripe ovum. -

Downloaded from Bioscientifica.Com at 10/02/2021 04:15:20AM Via Free Access 98
DEVELOPMENT AND RADIO-RESPONSE OF THE PRENATAL BOVINE OVARY B. H. ERICKSON Agricultural Research Laboratory of the University of Tennessee,^ Oak Ridge, Tennessee, U.S.A. {Received \2th May 1965) Summary. Qualitative observations of forty-nine bovine foetuses taken at varying stages of gestation revealed the following: (1) the germinal ridge is established at the 32nd day of gestation; (2) due to the formation of the tunica albuginea of the primitive testis, foetal sex is distinguishable by Day 39; (3) meiosis begins in ovaries at 75 to 80 days post coitum; (4) oogonial mitosis is discontinued by 150 to 170 days; (5) the majority of the oocytes have attained their stage of rest (pachytene) and are enveloped in primordial follicles by Day 170; and (6) vesicular follicles appear in ovaries at Day 250 of ges- tation. Total germ-cell numbers, based on volumetric determinations or direct counts, increased from a low of approximately 16,000 at Day 50 to a high of 2,700,000 at Day 110. From Day 110 numbers declined abruptly to 107,000 at Day 170 and the ovaries of four foetuses at 270 days of gestation (average length of gestation, 283 days) contained an average of 68,000 \m=+-\21,000 germ cells. Seventy prenatally irradiated (400 R, whole-body to dam) and twenty-five non-irradiated heifers were slaughtered at either 9 or 23 months of age. Microscopic examinations of their ovaries revealed that irradiation was apparently without effect during the interval of 17 to 59 days of gestation, and of questionable effect during the interval of 59 to 119 days of gestation.