Washington State Department of Health Data Notes for Opioid Dashboards
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Insomnia and Anxiety in Older People Sleeping Pills Are Usually Not the Best Solution
® Insomnia and anxiety in older people Sleeping pills are usually not the best solution lmost one-third of older people in the people who take one of United States take sleeping pills. These these medicines sleep medicines are also sometimes called only a little longer and A“sedative-hypnotics” or “tranquilizers.” They better than those who affect the brain and spinal cord. don’t take a medicine. Doctors prescribe some of these medicines Sleeping pills can for sleep problems. Some of these medicines have serious side effects. also can be used to treat other conditions, such All sedative-hypnotic medicines have special as anxiety or alcohol withdrawal. Sometimes, risks for older adults. Seniors are likely to be doctors also prescribe certain anti-depressants more sensitive to the medicines’ effects than for sleep, even though that’s not what they’re younger adults. And these medicines may designed to treat. stay in older people’s bodies longer. These Most older adults should first try to treat their medicines can cause confusion and memory insomnia without medicines. According to the problems that: American Geriatrics Society, there are safer and • Increase the risk of falls and hip fractures. better ways to improve sleep or reduce anxiety. These are common causes of hospital stays Here’s why: and death in older people. Sleeping pills may not help much. • Increase the risk of car accidents. Many ads say that sleeping pills help people get a full, restful night’s sleep. But studies show that this is not exactly true in real life. On average, The new “Z” medicines also have risks. -

Early Morning Insomnia, Daytime Anxiety, and Organic Mental Disorder Associated with Triazolam
Early Morning Insomnia, Daytime Anxiety, and Organic Mental Disorder Associated with Triazolam Tjiauw-Ling Tan, MD, Edward 0. Bixler, PhD, Anthony Kales, MD, Roger J. Cadieux, MD, and Amy L. Goodman, MD Hershey, Pennsylvania A psychiatric syndrome characterized by agita Sleep Disorders Clinic. He began taking triazolam tion, paranoid ideation, depersonalization, and de at bedtime in a 0.5-mg dose eight months before pression, as well as paresthesias and hyperacusis, his referral. Although the drug was effective ini has been attributed to administration of triazolam tially, tolerance developed, causing the patient to (Halcion).1 The occurrence of these reactions led gradually increase the dosage until eventually he to the removal of the drug from the market in the was taking a total of 1.5 mg nightly. Netherlands. Isolated behavioral side effects that The physical examination revealed no contribu include amnesia2-4 and hallucinations5 have also tory conditions. However, assessment of the pa been reported with administration of triazolam. tient’s mental status revealed that he was extreme Rebound insomnia6 and early morning insom ly guarded and suspicious and preoccupied with nia,7 both associated with increases in daytime his sleeplessness to the degree that this hypochon anxiety,7,8 are withdrawal syndromes known driacal concern had a delusional quality. He also to occur with rapidly eliminated benzodiazepine described two episodes indicating memory impair hypnotics such as triazolam. Rebound insomnia ment; both incidents occurred in the late afternoon consists of a marked increase in wakefulness and involved preparing to eat certain foods, which above baseline levels following drug withdrawal. -

And Calcium, Magnesium, Potassium and Sodium Oxybates (Xywav™)
Louisiana Medicaid Sodium Oxybate (Xyrem®) and Calcium, Magnesium, Potassium and Sodium Oxybates (Xywav™) The Louisiana Uniform Prescription Drug Prior Authorization Form should be utilized to request clinical authorization for sodium oxybate (Xyrem®) and calcium, magnesium, potassium and sodium oxybates (Xywav™). These agents have Black Box Warnings and are subject to Risk Evaluation and Mitigation Strategy (REMS) under FDA safety regulations. Please refer to individual prescribing information for details. Approval Criteria • The recipient is 7 years of age or older on date of request; AND • The recipient has a documented diagnosis of narcolepsy or cataplexy; AND • The prescribing provider is a Board-Certified Neurologist or a Board-Certified Sleep Medicine Physician; AND • By submitting the authorization request, the prescriber attests to the following: o The prescribing information for the requested medication has been thoroughly reviewed, including any Black Box Warning, Risk Evaluation and Mitigation Strategy (REMS), contraindications, minimum age requirements, recommended dosing, and prior treatment requirements; AND o All laboratory testing and clinical monitoring recommended in the product prescribing information have been completed as of the date of the request and will be repeated as recommended; AND o The recipient has no inappropriate concomitant drug therapies or disease states. Duration of initial authorization approval: 3 months Reauthorization Criteria • The recipient continues to meet all initial approval criteria; AND -

Prescription Drug Management
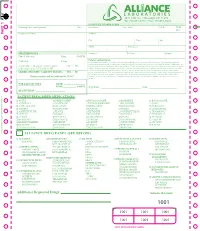
Check out our new site: www.acllaboratories.com Prescription Drug Management Non Adherence, Drug Misuse, Increased Healthcare Costs Reports from the Centers for DiseasePrescription Control and Prevention (CDC) say Drug deaths from Managementmedication overdose have risen for 11 straight years. In 2008 more than 36,000 people died from drug overdoses, and most of these deaths were caused by prescription Nondrugs. Adherence,1 Drug Misuse, Increased Healthcare Costs The CDC analysis found that nearly 40,000 drug overdose deaths were reported in 2010. Prescribed medication accounted for almost 60 percent of the fatalities—far more than deaths from illegal street drugs. Abuse of painkillers like ReportsOxyContin from and the VicodinCenters forwere Disease linked Control to the and majority Prevention of the (CDC) deaths, say deaths from according to the report.1 medication overdose have risen for 11 straight years. In 2008 more than 36,000 people died from drug overdoses, and most of these deaths were caused by prescription drugs. 1 A health economics study analyzed managed care claims of more than 18 million patients, finding that patients undergoing opioid therapyThe CDCfor chronic analysis pain found who that may nearly not 40,000 be following drug overdose their prescription deaths were regimenreported in 2010. Prescribed medication accounted for almost 60 percent of the fatalities—far more than deaths have significantly higher overall healthcare costs. from illegal street drugs. Abuse of painkillers like OxyContin and Vicodin were linked to the majority of the deaths, according to the report.1 ACL offers drug management testing to provide information that can aid clinicians in therapy and monitoring to help improve patientA health outcomes. -

Comparison of Short-And Long-Acting Benzodiazepine-Receptor Agonists
J Pharmacol Sci 107, 277 – 284 (2008)3 Journal of Pharmacological Sciences ©2008 The Japanese Pharmacological Society Full Paper Comparison of Short- and Long-Acting Benzodiazepine-Receptor Agonists With Different Receptor Selectivity on Motor Coordination and Muscle Relaxation Following Thiopental-Induced Anesthesia in Mice Mamoru Tanaka1, Katsuya Suemaru1,2,*, Shinichi Watanabe1, Ranji Cui2, Bingjin Li2, and Hiroaki Araki1,2 1Division of Pharmacy, Ehime University Hospital, Shitsukawa, Toon, Ehime 791-0295, Japan 2Department of Clinical Pharmacology and Pharmacy, Neuroscience, Ehime University Graduate School of Medicine, Shitsukawa, Toon, Ehime 791-0295, Japan Received November 7, 2007; Accepted May 15, 2008 Abstract. In this study, we compared the effects of Type I benzodiazepine receptor–selective agonists (zolpidem, quazepam) and Type I/II non-selective agonists (zopiclone, triazolam, nitrazepam) with either an ultra-short action (zolpidem, zopiclone, triazolam) or long action (quazepam, nitrazepam) on motor coordination (rota-rod test) and muscle relaxation (traction test) following the recovery from thiopental-induced anesthesia (20 mg/kg) in ddY mice. Zolpidem (3 mg/kg), zopiclone (6 mg/kg), and triazolam (0.3 mg/kg) similarly caused an approximately 2-fold prolongation of the thiopental-induced anesthesia. Nitrazepam (1 mg/kg) and quazepam (3 mg/kg) showed a 6- or 10-fold prolongation of the anesthesia, respectively. Zolpidem and zopiclone had no effect on the rota-rod and traction test. Moreover, zolpidem did not affect motor coordination and caused no muscle relaxation following the recovery from the thiopental-induced anesthesia. However, zopiclone significantly impaired the motor coordination at the beginning of the recovery. Triazolam significantly impaired the motor coordination and muscle relaxant activity by itself, and these impairments were markedly exacerbated after the recovery from anesthesia. -
Additional Requested Drugs
PART 1 PART PATIENT PRESCRIBED MEDICATIONS: o ACTIQ o DESIPRAMINE o HYDROCODONE o MORPHINE o ROXICODONE o ADDERALL o DIAZEPAM* o HYDROMORPHONE o MS CONTIN o SOMA o ALPRAZOLAM* o DILAUDID o IMIPRAMINE o NEURONTIN o SUBOXONE o AMBIEN o DURAGESIC o KADIAN o NORCO o TEMAZEPAM o AMITRIPTYLINE o ELAVIL o KETAMINE o NORTRIPTYLINE o TRAMADOL* o ATIVAN o EMBEDA o KLONOPIN o NUCYNTA o TYLENOL #3 o AVINZA o ENDOCET o LORAZEPAM o OPANA o ULTRAM o BUPRENEX o FENTANYL* o LORTAB o OXYCODONE o VALIUM o BUPRENORPHINE o FIORICET o LORCET o OXYCONTIN o VICODIN o BUTRANS o GABAPENTIN o LYRICA o PERCOCET o XANAX o CLONAZEPAM* o GRALISE o METHADONE o RESTORIL TO RE-ORDER CALL RITE-PRINT 718/384-4288 RITE-PRINT CALL TO RE-ORDER ALLIANCE DRUG PANEL (SEE BELOW) o ALCOHOL o BARBITURATES o ILLICITS o MUSCLE RELAXANTS o OPIODS (SYN) ETHANOL PHENOBARBITAL 6-MAM (HEROIN)* CARISPRODOL FENTANYL* BUTABARBITAL a-PVP MEPROBAMATE MEPERIDINE o AMPHETAMINES SECOBARBITAL BENZOYLECGONINE NALOXONE AMPHETAMINE PENTOBARBITAL LSD o OPIODS (NATURAL) METHADONE* METHAMPHETAMINE BUTALBITAL MDA CODEINE METHYLPHENEDATE MDEA MORPHINE o NON-OPIOID o BENZODIAZEPINES MDMA ANALGESICS o OPIODS (SEMI-SYN) o ANTICONVULSIVES ALPRAZOLAM* MDPV TRAMADOL BUPRENORPHINE* GABAPENTIN CLONAZEPAM* MEPHEDRONE TAPENTADOL DIHROCODEINE PREGABALIN DIAZEPAM METHCATHINONE DESOMORPHINE o NON-BENZODIAZEPINE FLUNITRAZEPAM* METHYLONE HYDROCODONE HYPNOTIC o ANTIDEPRESSANTS FLURAZEPAM* PCP HYDROMORPHONE ZOLPIDEM* AMITRIPTYLINE LORAZEPAM THC* OXYCODONE DOXEPIN OXAZEPAM CBD ° OXYMORPHONE o MISCELLANEOUS DRUGS IMIPRIMINE -
![Nembutal [Pentobarbital] Injection and Seconal [Secobarbital] Capsules](https://docslib.b-cdn.net/cover/6349/nembutal-pentobarbital-injection-and-seconal-secobarbital-capsules-686349.webp)
Nembutal [Pentobarbital] Injection and Seconal [Secobarbital] Capsules
Pharmacy Benefit Coverage Criteria Effective Date .......................................... 12/1/2020 Next Review Date… ................................... 12/1/2021 Coverage Policy Number ................................ P0095 Nembutal [pentobarbital] injection and Seconal [secobarbital] capsules Table of Contents Related Coverage Resources Overview .............................................................. 1 Coverage Policy ................................................... 1 FDA Summary ..................................................... 1 General Background ............................................ 2 References .......................................................... 2 INSTRUCTIONS FOR USE The following Coverage Policy applies to health benefit plans administered by Cigna Companies. Certain Cigna Companies and/or lines of business only provide utilization review services to clients and do not make coverage determinations. References to standard benefit plan language and coverage determinations do not apply to those clients. Coverage Policies are intended to provide guidance in interpreting certain standard benefit plans administered by Cigna Companies. Please note, the terms of a customer’s particular benefit plan document [Group Service Agreement, Evidence of Coverage, Certificate of Coverage, Summary Plan Description (SPD) or similar plan document] may differ significantly from the standard benefit plans upon which these Coverage Policies are based. For example, a customer’s benefit plan document may contain a specific -

S1 Table. List of Medications Analyzed in Present Study Drug
S1 Table. List of medications analyzed in present study Drug class Drugs Propofol, ketamine, etomidate, Barbiturate (1) (thiopental) Benzodiazepines (28) (midazolam, lorazepam, clonazepam, diazepam, chlordiazepoxide, oxazepam, potassium Sedatives clorazepate, bromazepam, clobazam, alprazolam, pinazepam, (32 drugs) nordazepam, fludiazepam, ethyl loflazepate, etizolam, clotiazepam, tofisopam, flurazepam, flunitrazepam, estazolam, triazolam, lormetazepam, temazepam, brotizolam, quazepam, loprazolam, zopiclone, zolpidem) Fentanyl, alfentanil, sufentanil, remifentanil, morphine, Opioid analgesics hydromorphone, nicomorphine, oxycodone, tramadol, (10 drugs) pethidine Acetaminophen, Non-steroidal anti-inflammatory drugs (36) (celecoxib, polmacoxib, etoricoxib, nimesulide, aceclofenac, acemetacin, amfenac, cinnoxicam, dexibuprofen, diclofenac, emorfazone, Non-opioid analgesics etodolac, fenoprofen, flufenamic acid, flurbiprofen, ibuprofen, (44 drugs) ketoprofen, ketorolac, lornoxicam, loxoprofen, mefenamiate, meloxicam, nabumetone, naproxen, oxaprozin, piroxicam, pranoprofen, proglumetacin, sulindac, talniflumate, tenoxicam, tiaprofenic acid, zaltoprofen, morniflumate, pelubiprofen, indomethacin), Anticonvulsants (7) (gabapentin, pregabalin, lamotrigine, levetiracetam, carbamazepine, valproic acid, lacosamide) Vecuronium, rocuronium bromide, cisatracurium, atracurium, Neuromuscular hexafluronium, pipecuronium bromide, doxacurium chloride, blocking agents fazadinium bromide, mivacurium chloride, (12 drugs) pancuronium, gallamine, succinylcholine -
2019 01 07 Classification Substances
DRUG TESTING STANDARDS AND PRACTICES PROGRAM. Uniform Classification Guidelines for Foreign Substances And Recommended Penalties Model Rule. January, 2019 (V.14.0) © ASSOCIATION OF RACING COMMISSIONERS INTERNATIONAL – 2019. Association of Racing Commissioners International 2365 Harrodsburg Road- B450 Lexington, Kentucky, USA www.arci.com Page 1 of 66 Preamble to the Uniform Classification Guidelines of Foreign Substances The Preamble to the Uniform Classification Guidelines was approved by the RCI Drug Testing and Quality Assurance Program Committee (now the Drug Testing Standards and Practices Program Committee) on August 26, 1991. Minor revisions to the Preamble were made by the Drug Classification subcommittee (now the Veterinary Pharmacologists Subcommittee) on September 3, 1991. "The Uniform Classification Guidelines printed on the following pages are intended to assist stewards, hearing officers and racing commissioners in evaluating the seriousness of alleged violations of medication and prohibited substance rules in racing jurisdictions. Practicing equine veterinarians, state veterinarians, and equine pharmacologists are available and should be consulted to explain the pharmacological effects of the drugs listed in each class prior to any decisions with respect to penalities to be imposed. The ranking of drugs is based on their pharmacology, their ability to influence the outcome of a race, whether or not they have legitimate therapeutic uses in the racing horse, or other evidence that they may be used improperly. These classes of drugs are intended only as guidelines and should be employed only to assist persons adjudicating facts and opinions in understanding the seriousness of the alleged offenses. The facts of each case are always different and there may be mitigating circumstances which should always be considered. -

Prescription Sleep Aid Use Among Adults: United States, 2005–2010
NCHS Data Brief ■ No. 127 ■ August 2013 Prescription Sleep Aid Use Among Adults: United States, 2005–2010 Yinong Chong, Ph.D.; Cheryl D. Fryar, M.S.P.H.; and Qiuping Gu, M.D., Ph.D. Sedative and hypnotic medications, often referred to as sleep aids, are used Key findings to induce or maintain sleep by suppressing activities in the central nervous Data from the National system. In the past two decades, both popular media and pharmaceutical Health and Nutrition companies have reported an increased number of prescriptions filled for sleep Examination Survey, aids in the United States (1,2). In fact, a market research firm has reported a 2005–2010 tripling in sleep aid prescriptions from 1998 to 2006 for young adults aged 18–24 (3). This report presents person-based nationally representative • About 4% of U.S. adults aged 20 and over used estimates on prescription sleep aid use in the past 30 days, describes prescription sleep aids in the sociodemographic differences in use, and examines sleep aid use by self- past month. reported sleep duration and insomnia. • The percentage of adults Keywords: hypnotic medications • sleeping pills • insomnia • National Health using a prescription sleep and Nutrition Examination Survey aid increased with age and education. More adult women Prescription sleep aid use in the past 30 days increased (5.0%) used prescription sleep aids than adult men (3.1%). with age. • Non-Hispanic white adults Figure 1. Percentage of adults aged 20 and over who used prescription sleep aids in the past 30 were more likely to use sleep days, by age: United States, 2005–2010 aids (4.7%) than non-Hispanic 8 black (2.5%) and Mexican- 17.0 American (2.0%) adults. -

A Fast Analytical LC/MS/MS Method for the Simultaneous Analysis of Barbiturates and 11-Nor-9-Carboxy-Δ9- Tetrahydrocannabinol (THC-A) in Urine
Application Note Clinical Research A Fast Analytical LC/MS/MS Method for the Simultaneous Analysis of Barbiturates and 11-nor-9-carboxy-Δ9- tetrahydrocannabinol (THC-A) in Urine Using ESI negative ionization mode and alternating column regeneration Authors Abstract Andre Szczesniewski and Most of the compounds in large drug panels are analyzed using positive ionization Carrie J. Adler mode. However, barbiturates and 11-nor-9-carboxy-Δ9-THC (THC-A) perform better Agilent Technologies, Inc. using electrospray ionization (ESI) in negative mode with the mobile phase pH favorable for negative ionization. This work developed a fast analytical method combining eight barbiturates and THC-A in a single analysis using alternating column regeneration (ACR) to increase sample throughput. Moving the analytes preferring negative ionization into a separate test increases the analytical sensitivity of the compounds, allowing for greater research capabilities. The simple sample preparation techniques used provided rapid analysis, good analytical sensitivity, and quantitation over a wide dynamic range. This analysis used an Agilent 6470 triple quadrupole mass spectrometer with Agilent Jet Stream technology in ESI negative ionization mode and an Agilent Infinity II 1290 UHPLC system. A second pump and 2-position 10-port switching valve were added to facilitate use of the ACR. A 100 µL aliquot of human urine was used for the analysis of barbiturates and THC-A. Chromatographic separation of the analytes was achieved in less than 3 minutes using a gradient method composed of a H2O:acetonitrile mixture with 5 mM ammonium acetate and two Agilent Poroshell 120 EC-C18, 2.1 × 100 mm, 1.9 μm columns. -

Treatment for Acute Pain: an Evidence Map Technical Brief Number 33
Technical Brief Number 33 R Treatment for Acute Pain: An Evidence Map Technical Brief Number 33 Treatment for Acute Pain: An Evidence Map Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 5600 Fishers Lane Rockville, MD 20857 www.ahrq.gov Contract No. 290-2015-0000-81 Prepared by: Minnesota Evidence-based Practice Center Minneapolis, MN Investigators: Michelle Brasure, Ph.D., M.S.P.H., M.L.I.S. Victoria A. Nelson, M.Sc. Shellina Scheiner, PharmD, B.C.G.P. Mary L. Forte, Ph.D., D.C. Mary Butler, Ph.D., M.B.A. Sanket Nagarkar, D.D.S., M.P.H. Jayati Saha, Ph.D. Timothy J. Wilt, M.D., M.P.H. AHRQ Publication No. 19(20)-EHC022-EF October 2019 Key Messages Purpose of review The purpose of this evidence map is to provide a high-level overview of the current guidelines and systematic reviews on pharmacologic and nonpharmacologic treatments for acute pain. We map the evidence for several acute pain conditions including postoperative pain, dental pain, neck pain, back pain, renal colic, acute migraine, and sickle cell crisis. Improved understanding of the interventions studied for each of these acute pain conditions will provide insight on which topics are ready for comprehensive comparative effectiveness review. Key messages • Few systematic reviews provide a comprehensive rigorous assessment of all potential interventions, including nondrug interventions, to treat pain attributable to each acute pain condition. Acute pain conditions that may need a comprehensive systematic review or overview of systematic reviews include postoperative postdischarge pain, acute back pain, acute neck pain, renal colic, and acute migraine.