Primary Health Matters
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Impact of Sea Level Rise on Coastal Natural Values in Tasmania
Impact of sea level rise on coastal natural values in Tasmania JUNE 2016 Department of Primary Industries, Parks, Water and Environment Acknowledgements Thanks to the support we received in particular from Clarissa Murphy who gave six months as a volunteer in the first phase of the sea level rise risk assessment work. We also had considerable technical input from a range of people on various aspects of the work, including Hans and Annie Wapstra, Richard Schahinger, Tim Rudman, John Church, and Anni McCuaig. We acknowledge the hard work over a number of years from the Sea Level Rise Impacts Working Group: Oberon Carter, Louise Gilfedder, Felicity Faulkner, Lynne Sparrow (DPIPWE), Eric Woehler (BirdLife Tasmania) and Chris Sharples (University of Tasmania). This report was compiled by Oberon Carter, Felicity Faulkner, Louise Gilfedder and Peter Voller from the Natural Values Conservation Branch. Citation DPIPWE (2016) Impact of sea level rise on coastal natural values in Tasmania. Natural and Cultural Heritage Division, Department of Primary Industries, Parks, Water and Environment, Hobart. www.dpipwe.tas.gov.au ISBN: 978-1-74380-009-6 Cover View to Mount Cameron West by Oberon Carter. Pied Oystercatcher by Mick Brown. The Pied Oystercatcher is considered to have a very high exposure to sea level rise under both a national assessment and Tasmanian assessment. Its preferred habitat is mudflats, sandbanks and sandy ocean beaches, all vulnerable to inundation and erosion. Round-leaved Pigface (Disphyma australe) in flower in saltmarsh at Lauderdale by Iona Mitchell. Three saltmarsh communities are associated with the coastal zone and are considered at risk from sea level rise. -

Deal Island an Historical Overview
Introduction. In June 1840 the Port Officer of Hobart Captain W. Moriarty wrote to the Governor of Van Diemen’s Land, Sir John Franklin suggesting that lighthouses should be erected in Bass Strait. On February 3rd. 1841 Sir John Franklin wrote to Sir George Gipps, Governor of New South Wales seeking his co-operation. Government House, Van Diemen’s Land. 3rd. February 1841 My Dear Sir George. ………………….This matter has occupied much of my attention since my arrival in the Colony, and recent ocurances in Bass Strait have given increased importance to the subject, within the four years of my residence here, two large barques have been entirely wrecked there, a third stranded a brig lost with all her crew, besides two or three colonial schooners, whose passengers and crew shared the same fate, not to mention the recent loss of the Clonmell steamer, the prevalence of strong winds, the uncertainty of either the set or force of the currents, the number of small rocks, islets and shoals, which though they appear on the chart, have but been imperfectly surveyed, combine to render Bass Strait under any circumstances an anxious passage for seamen to enter. The Legislative Council, Votes and Proceedings between 1841 – 42 had much correspondence on the viability of erecting lighthouses in Bass Strait including Deal Island. In 1846 construction of the lightstation began on Deal Island with the lighthouse completed in February 1848. The first keeper William Baudinet, his wife and seven children arriving on the island in March 1848. From 1816 to 1961 about 18 recorded shipwrecks have occurred in the vicinity of Deal Island, with the Bulli (1877) and the Karitane (1921) the most well known of these shipwrecks. -

South-East Marine Region Profile
South-east marine region profile A description of the ecosystems, conservation values and uses of the South-east Marine Region June 2015 © Commonwealth of Australia 2015 South-east marine region profile: A description of the ecosystems, conservation values and uses of the South-east Marine Region is licensed by the Commonwealth of Australia for use under a Creative Commons Attribution 3.0 Australia licence with the exception of the Coat of Arms of the Commonwealth of Australia, the logo of the agency responsible for publishing the report, content supplied by third parties, and any images depicting people. For licence conditions see: http://creativecommons.org/licenses/by/3.0/au/ This report should be attributed as ‘South-east marine region profile: A description of the ecosystems, conservation values and uses of the South-east Marine Region, Commonwealth of Australia 2015’. The Commonwealth of Australia has made all reasonable efforts to identify content supplied by third parties using the following format ‘© Copyright, [name of third party] ’. Front cover: Seamount (CSIRO) Back cover: Royal penguin colony at Finch Creek, Macquarie Island (Melinda Brouwer) B / South-east marine region profile South-east marine region profile A description of the ecosystems, conservation values and uses of the South-east Marine Region Contents Figures iv Tables iv Executive Summary 1 The marine environment of the South-east Marine Region 1 Provincial bioregions of the South-east Marine Region 2 Conservation values of the South-east Marine Region 2 Key ecological features 2 Protected species 2 Protected places 2 Human activities and the marine environment 3 1. -

Tasmania Results
2019 federal election Results Map TASMANIA MACQUARIE ISLAND VICTORIA AUSTRALIA Macquarie Island is part of the Division of Franklin. Macquarie 0 1000 km Island BRADDON (includes King Island) King Island BASS STRAIT Flinders Island BASS (includes Flinders Island and Cape Barren Island) Cape Barren Island Smithton Wynyard Bridport Burnie George Town Ulverstone Branxholm Devonport BASS Lilydale Shefeld Waratah Launceston Scamander Mole Creek Evandale BRADDON Cressy Fingal Zeehan Bicheno Campbell Town Queenstown Swansea LYONS Oatlands Bothwell Orford FRANKLIN Bridgewater Maydena Richmond New Norfolk Sorell Eaglehawk Neck Franklin Cygnet Nubeena FRANKLIN Key Dover Division boundary LYONS Division name Bruny Island FRANKLIN (includes Party Bruny Island) Liberal Party* Australian Labor Party * Liberal/National Coalition The electoral boundaries represented on this map are those in place at the 2019 election. 0 50 km 2019 federal election Results Map TASMANIA Hobart Urban Tea Tree Bridgewater River Austins Ferry FRANKLIN Claremont Derwent Chigwell Dowsing Point Risdon Vale Berriedale Glenlusk Rosetta Montrose Derwent Park Lutana Glenorchy Collinsvale FRANKLIN Moonah West Moonah New Town Lenah North Valley Hobart Bellerive West Hobart Hobart Wellington Park CLARK Battery Point South Hobart Dynnyrne Sandy Bay Mount Nelson Ridgeway Fern Tree Taroona Neika Bonnet Longley Hill Leslie Vale Kingston Key Division boundary CLARK Division name Party Independent The electoral boundaries represented on this map are those in place at the 2019 election. 0 2 km. -

Overview of Tasmania's Offshore Islands and Their Role in Nature
Papers and Proceedings of the Royal Society of Tasmania, Volume 154, 2020 83 OVERVIEW OF TASMANIA’S OFFSHORE ISLANDS AND THEIR ROLE IN NATURE CONSERVATION by Sally L. Bryant and Stephen Harris (with one text-figure, two tables, eight plates and two appendices) Bryant, S.L. & Harris, S. 2020 (9:xii): Overview of Tasmania’s offshore islands and their role in nature conservation.Papers and Proceedings of the Royal Society of Tasmania 154: 83–106. https://doi.org/10.26749/rstpp.154.83 ISSN: 0080–4703. Tasmanian Land Conservancy, PO Box 2112, Lower Sandy Bay, Tasmania 7005, Australia (SLB*); Department of Archaeology and Natural History, College of Asia and the Pacific, Australian National University, Canberra, ACT 2601 (SH). *Author for correspondence: Email: [email protected] Since the 1970s, knowledge of Tasmania’s offshore islands has expanded greatly due to an increase in systematic and regional surveys, the continuation of several long-term monitoring programs and the improved delivery of pest management and translocation programs. However, many islands remain data-poor especially for invertebrate fauna, and non-vascular flora, and information sources are dispersed across numerous platforms. While more than 90% of Tasmania’s offshore islands are statutory reserves, many are impacted by a range of disturbances, particularly invasive species with no decision-making framework in place to prioritise their management. This paper synthesises the significant contribution offshore islands make to Tasmania’s land-based natural assets and identifies gaps and deficiencies hampering their protection. A continuing focus on detailed gap-filling surveys aided by partnership restoration programs and collaborative national forums must be strengthened if we are to capitalise on the conservation benefits islands provide in the face of rapidly changing environmental conditions and pressure for future use. -
Nowhere Else on Earth
Nowhere Else on Earth: Tasmania’s Marine Natural Values Environment Tasmania is a not-for-profit conservation council dedicated to the protection, conservation and rehabilitation of Tasmania’s natural environment. Australia’s youngest conservation council, Environment Tasmania was established in 2006 and is a peak body representing over 20 Tasmanian environment groups. Prepared for Environment Tasmania by Dr Karen Parsons of Aquenal Pty Ltd. Report citation: Parsons, K. E. (2011) Nowhere Else on Earth: Tasmania’s Marine Natural Values. Report for Environment Tasmania. Aquenal, Tasmania. ISBN: 978-0-646-56647-4 Graphic Design: onetonnegraphic www.onetonnegraphic.com.au Online: Visit the Environment Tasmania website at: www.et.org.au or Ocean Planet online at www.oceanplanet.org.au Partners: With thanks to the The Wilderness Society Inc for their financial support through the WildCountry Small Grants Program, and to NRM North and NRM South. Front Cover: Gorgonian fan with diver (Photograph: © Geoff Rollins). 2 Waterfall Bay cave (Photograph: © Jon Bryan). Acknowledgements The following people are thanked for their assistance The majority of the photographs in the report were with the compilation of this report: Neville Barrett of the generously provided by Graham Edgar, while the following Institute for Marine and Antarctic Studies (IMAS) at the additional contributors are also acknowledged: Neville University of Tasmania for providing information on key Barrett, Jane Elek, Sue Wragge, Chris Black, Jon Bryan, features of Tasmania’s marine -

Tasmanian Aborigines in the Furneaux Group in the Nine Teenth Century—Population and Land
‘I hope you will be my frend’: Tasmanian Aborigines in the Furneaux Group in the nine teenth century—population and land tenure Irynej Skira Abstract This paper traces the history of settlement of the islands of the Furneaux Group in Bass Strait and the effects of government regulation on the long term settlements of Tasma nian Aboriginal people from the 1850s to the early 1900s. Throughout the nineteenth century the Aboriginal population grew slowly eventually constituting approximately 40 percent of the total population of the Furneaux Group. From the 1860s outsiders used the existing land title system to obtain possession of the islands. Aborigines tried to establish tenure through the same system, but could not compete because they lacked capital, and were disadvantaged by isolation in their communication with gov ernment. Further, the islands' use for grazing excluded Aborigines who rarely had large herds of stock and were generally not agriculturalists. The majority of Aborigines were forced to settle on Cape Barren Island, where they built homes on a reserve set aside for them. European expansion of settlement on Flinders Island finally completed the disen franchisement of Aboriginal people by making the Cape Barren Island enclave depend ent on the government. Introduction In December 1869 Thomas Mansell, an Aboriginal, applied to lease a small island. He petitioned the Surveyor-General, T hope you will be my Frend...I am one of old hands Her, and haf Cast and have large family and no hum'.1 Unfortunately, he could not raise £1 as down payment. Mansell's was one of the many attempts by Aboriginal people in the Furneaux Group to obtain valid leasehold or freehold and recognition of their long term occupation. -

Papers and Proceedings of the Royal Society of Tasmania
— ;; CORE Metadata, citation and similar papers at core.ac.uk Provided by University of Tasmania Open Access Repository CONTRIBUTIONS TO THE PHYTOGRAPHY OF TASMANIA. [By Fred, BIueller, M.D., F.R.S,! This brief allusion to some plants, either unrecorded from Tasmania or rare in its territory, refers to contributions gained from various sources. Robert Brown's great treasures fur- nished some of the data, as will be evident on reference to the universal work on Australian Vegetation, issued by the Pre- sident of the Linnean Society. Others of the plants were kindly transmitted by Mr. J. Bennett from the British Museum, and gathered by Dr. Jos. Milligan. Some were detected by Mr. Aug. Oldfield, and remained unnoticed in the supplemental contribution, which it fell to my share to furnish for the " Flora Tasmanise." A few again were added by Mr. Walt. Bissell, in a recent voyage to the North-east Coast while I was agreeably surprised to receive from the venerable Dr. Gr. Story an extensive set of Museum-plants, secured in the Oyster Bay district. From a letter of this gentleman I sub- mit introductorily the following physiographic remarks, which claim in many respects originality : This district is a tract of waste, extending from Cape Bernier on the south to Doctor's Creek, or Seymour Coal. Mines, on the north ; it was formerly known as the District of Oyster Bay, as that bay occupies a considerable portion of the coast-line. At present the south part is in the County of Pembroke, and the other part forms the County of Glamorgan, forming together a coast-line of 80 miles. -
Appendix 7-2 Protected Matters Search Tool (PMST) Report for the Risk EMBA
Environment plan Appendix 7-2 Protected matters search tool (PMST) report for the Risk EMBA Stromlo-1 exploration drilling program Equinor Australia B.V. Level 15 123 St Georges Terrace PERTH WA 6000 Australia February 2019 www.equinor.com.au EPBC Act Protected Matters Report This report provides general guidance on matters of national environmental significance and other matters protected by the EPBC Act in the area you have selected. Information on the coverage of this report and qualifications on data supporting this report are contained in the caveat at the end of the report. Information is available about Environment Assessments and the EPBC Act including significance guidelines, forms and application process details. Report created: 13/09/18 14:02:20 Summary Details Matters of NES Other Matters Protected by the EPBC Act Extra Information Caveat Acknowledgements This map may contain data which are ©Commonwealth of Australia (Geoscience Australia), ©PSMA 2010 Coordinates Buffer: 1.0Km Summary Matters of National Environmental Significance This part of the report summarises the matters of national environmental significance that may occur in, or may relate to, the area you nominated. Further information is available in the detail part of the report, which can be accessed by scrolling or following the links below. If you are proposing to undertake an activity that may have a significant impact on one or more matters of national environmental significance then you should consider the Administrative Guidelines on Significance. World Heritage Properties: 11 National Heritage Places: 13 Wetlands of International Importance: 13 Great Barrier Reef Marine Park: None Commonwealth Marine Area: 2 Listed Threatened Ecological Communities: 14 Listed Threatened Species: 311 Listed Migratory Species: 97 Other Matters Protected by the EPBC Act This part of the report summarises other matters protected under the Act that may relate to the area you nominated. -
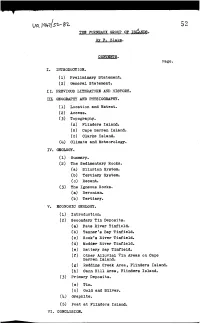
THE FURNEAUX GROUP of Istanns. by F. Blake. CONTENTS. I. INTRODUCTION. (1) Preliminary Statement. (2) General Statement. II
52 THE FURNEAUX GROUP OF IStANns. By F. Blake. CONTENTS. Page. I. INTRODUCTION. (1) Preliminary Statement. (2) General Statement. II. PREVIOUS LITERATURE AND HISTOR~. III. GEOGRAPHY AND PHYSIOGRAPHY. (1) Location and Extent. (2) Access. ( 5) Topography. (A) Flinders Island. (B) Cape Barren Island. (c) Clarke Island. (4) Climate and Meteorology. IV. GEOLOGY. (1) Summary. (2) The Sedimentary Rocks. (a) Silurian System. (b) Tertiary System. (c) Recent. (3) The Igneous Rocks. (a) Devonian. (b) Tertiary. V. ECONOMIC GEOLOGY. (1) Introduction. (2) Secondary Tin Deposits. (a) Pats River Tin:field. (b) Tanner's Bay Tin:field. (c) ROOk's River Tin:field. (d) Modder River Tin:field. (e) Battery Bay Tin:field. (f) Other Alluvial Tin Areas on Cape Barren Island. (g) Reddins Creek Area, Flinders Island. (h) Cann Hill Area, Flinders Island. (3) Primary Deposits. (a) Tin. Cb) Gold and Silver. (4) Graphite. (5) Peat at Flinders Island. VI. CONCLUSION. 53 TEE FURNEAUX GROUP OF ISLANDS I. INTRODUCTION (1) Preliminary Statement. Flinders and Cape Barren Islands have been steady, though small, contributors to the tin output of this State over a period of 45 years. During this time no outstanding mining events have taken place and the development has proved to be of slow progression. No large mines are in existence and mining generally has been confined to the winning of alluvial tin on a small scale. Flinders Island is better known for the splendid grazing areas along the west coast belt, which are so suitable for dairy-farming, and cattle and sheep raising. (2) General Statement. The field work in the Furneaux Group was carried out during the period between the 6th May and 29th June, 1935. -

"Permo-Carboniferous Fossil Cliffs" at Darlington, Maria Island
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by University of Tasmania Open Access Repository FUKTHER NOTES ON THE "PERMO-CAR- BONIFEROUS FOSSIL CLIFFS" AT DARLINGTON, MARIA ISLAND. By R. M. Johnston, F.S.S. (Bead lOfh May, 1900.; Maria Island, lying to the east of Spring Bay, must be regarded as the most southerly outline of the great granite axis forming the eastern fringe of Tas- mania, traceable northwards through Schouten Island, Freycinet's Peninsula, Bicheno, Falmouth, St. Helens, Eddystone Point, to Gladstone. Crossing the narrow Banks' Strait it may be further traced through Clarke Island, Cape Barren Island, Long Island, Goose Island, Hummock Island, the Strzelecki Peaks, and Killicrankie Range of Flinders Island, and the elevated masses of granite forming the interesting cluster of islets known as the Kent's Group. From this point the granite axis is again traceable through the rocky shoals, reefs, and islets to the most southerly Hmit of the Australian main- land at the granite headlands of Wilson's Promontory. Maria Island, like Bruni Island, is divided into two parts— North Maria and South Maria. The two divisions are connected, between Oyster Bay on the west and Reidle Bay on the east, by a narrow strip of sand two or three miles long, giving the island^ as a whole, somewhat the appearance of an ancient hour-glass. The greatest length lies between Cape Boulanger on the extreme north, and Cape Peron on the extreme south, covering a distance of about 15 miles. The greatest breadth, about 10 miles, lies in a line between Long Point on the west, and Ragged Head on the east ; that is within the larger division of the North Island. -

Tasmanian Mainland and Islands As Shown to 2Nm Coastline*
. Erith Island 145°12'E 145°15'E Deal Island 1 42° 30.22' S 145° 12.39' E Outer Sister Island 2 42° 30.22' S 145° 15.72' E Dover Island Inner Sister Island 3 43° 32.64' S 146° 29.22' E Babel Island 4 43° 34.64' S 146° 29.22' E King Island er S S ' v ' S i S 0 0 ° R ° 3 3 0 r 0 ° ° 4 M e 4 2 o dd 2 Flinders 4 4 Island Three Hummock Island Sources: Esri, GEBCO, NOAA, Walker Island Cape Barren Island National Geographic, DeLorme, Hunter Island Robbins Island HERE, Geonames.org, and Perkins Island other contributors Clarke Island 145°12'E 145°15'E Waterhouse Island Swan Island S S ° ° 1 1 4 4 Area extending seawards from the coastline of the Tasmanian mainland and islands as shown to 2nm Coastline* S S ° ° 2 2 4 GEODATA Coast 100K 2004 is a vector representation of the topographic 4 features depicting Australia`s coastline, and State and Territory borders. T A S M A N II A Data are derived from the1:100,000 scale National Topographic Map Series and contains: 146°27'E 146°30'E Schouten Island t in o - Coastline features (as determined by Mean High Water) P r a - Survey Monument Points (survey points used to define State/Territory borders) rr u See Inset A P - State and Territory land borders S S ' ' Maria Island 3 3 - Island features. 3 3 ° ° 3 3 4 4 The coastline includes the main outline of the land and includes bays, the outer edge of mangroves and closes off narrow inlets and S S ° ° 3 3 4 watercourses at or near their mouths.